Abdomen Assessment
advertisement

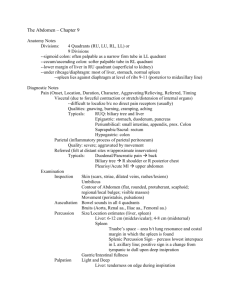
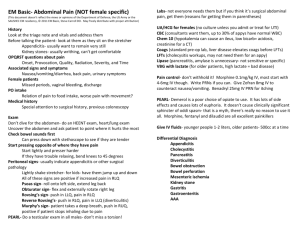
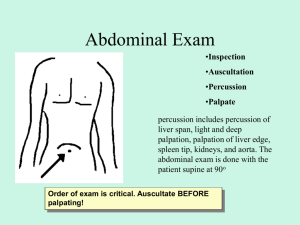
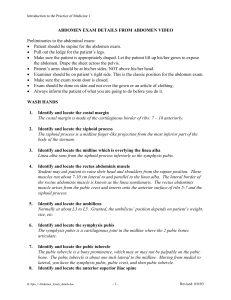
Abdomen Assessment D. Tanner, RN, MSN NUR 211 Fall Semester Anatomy of the Abdomen 4 Quadrants RUQ, RLQ, LUQ, LLQ Midline 9 Regions- epigastric, umbilical, suprapubic The word "abdomen" has a curious story behind it. It comes from the Latin "abdodere", to hide. The idea was that whatever was eaten was hidden in the abdomen. 4 Quadrants 9 Regions Location! Location! Location! RUQ liver gallbladder duodenum (small intestine) pancreas head right kidney and adrenal Location! Location! Location! RLQ cecum appendix right ovary and tube Location! Location! Location! LLQ sigmoid colon left ovary and tube LUQ stomach spleen pancreas left kidney and adrenal GI Variations Due to Age Aging- should not affect GI function unless associated with a disease process Decreased: salivation, sense of taste, gastric acid secretion, esophageal emptying, liver size, bacterial flora Increased: constipation! GI Variations with pregnancy Decrease in gastric motility High incidence of N, V (r/t pregnancy hormones) and “heartburn” or acid reflux Bowel sounds diminished r/t enlarged uterus displacing intestines Linea nigra- increased pigmentation of abd midline Striae Gravidarum Nursing History - Abdomen Subjective Data: Ask about: Appetite Wt gain or loss Dysphagia Intolerance to certain foods Any Abdominal Pain of Nausea and Vomiting Bowel movements Any past abdominal problems Nursing History Infants and Children – Ask: bottle or breast fed, any table foods, how often & how well & how much the baby eat, any problems with constipation, c/o of any abdominal pain TeenagersAsk: nutritional assessment, activity & exercise patterns, recent wt. loss or gain Nursing History Older Adults Ask: how do you get your groceries? prepare your meals? do you have any trouble swallowing? how often do your bowels move? how often do you take anything for constipation? Rx / OTC/ herbs what meds do you take? Nursing Assessment Objective Data: General Observation Inspect Auscultate Percuss Palpate (always last) Focused Health History Nutrition Allergies Medications Cigarette/tobacco ETOH intake Recreational drug use Stool characteristics Urine characteristics Exposure to infectious dz. Recent stressful life events Possibility of Pregnancy Techniques for Exam Provide privacy Good lighting/appropriate temp in rm Expose the abdomen Empty bladder Position pt supine, arms by side & head on pillow with knees slightly bent or on a pillow Warm stethoscope & hands Painful areas last Distraction techniques Inspection Overall observation Abd contour- flat, scaphoid, round, protuberant Abd symmetry and skin color - note any masses, striae, scars, veins, pigmentation Pulsations Auscultation Always done before percussion & palpation Use diaphragm of stethoscope Listen lightly Start with RLQ Auscultation What makes a bowel sound? Note character & frequency of bowel sounds (530 times/minute) Sounds like….. Listen for 5 minutes before documenting absent bowel sounds Listen for bruits- aortic, renal, iliac, femoral Hyper- gastroenteritis, obstruction, hungry Hypo- pregnancy, peritonitis Percussion Gently tapping on the skin to create a vibration Detect fluid, gaseous distention and masses Tympany- gas (dominant sound because of air in sm intestine) Dullness- solid masses, distended bladder Percuss liver, spleen ,kidneys Palpation of Abdomen Light palpation- depress about 1 cm. Assess skin pulsations. Always done first- clockwise Deep palpation- depress skin about 5-8 cm. Always assess tender areas last. Watch pt’s expression during palpation Inspection Abnormal Findings Visible or distended veins- ascites Visible peristalsis- obstruction Spider nevi (cutaneous angiomas)- cirrhosis Asymmetry/ Distention- mass or intestinal obsruction Color changes- jaundice, bluish/cyanotic Abnormal Auscultation Absence/Hyperactive bowel sounds“borborygmi” Bruits- “swoosh” Peritoneal Friction Rub- rough, grating heard over liver & spleen- inflammation of peritoneal surface from tumor, infection, etc. Percussion Abnormal Findings Enlarged organs, palpable masses, distention, ascites Marked tenderness Palpation Abnormal Findings Tenderness- rebound- done away from painful area- done at end of exam Masses- document location, size, shape, mobile, pulsating, smooth, nodular, firm Firmness or muscle guarding/rigidityintraabdominal bleeding- DO NOT CONTINUE TO PALPATE!!!!!! Special Procedures Fluid Wave- need 3 hands- feel for impulse of the wave of fluid across the abdomen= ascites Rebound Tenderness- Blumberg’s Sign Iliopsoas Muscle Test- thigh muscle lift R leg and push down on R thigh= appendicitis Obturator Test- lift R leg and rotate at 90 degrees= muscle is irritated by appendicitis Murphy’s Sign- “inspiratory arrest” palpate the liver should be painless= cholecystitis Special Procedures McBurney’s Point- RLQ midclavicular= appendicitis Referred pain- location of pain is not necessarily where the involved organ is! May be felt where the organ was located in fetal development ex: spleen= L shoulder pain/ kidney= groin pain Hooking technique- palpate the liver- feeling for the liver edge Special Procedures Cullen’s Sign- bluish discoloration around the umbilicus EMERGENCY!!! Kehr’s Sign- abd pain radiating to R shoulder= spleen or pancreatitis Sample Documentation Normal ExamAbdomen soft, rounded and symmetric without distention; no lesions or scars, or visible peristalsis. Aorta midline without bruit or visible pulsation; umbilicus inverted and midline without herniation; bowel sounds present in all 4 quadrants. Liver, kidney and spleen nonpalpable; no tenderness on palpation. Reports good appetite; no constipation, nausea or diarrhea. Voiding well and denies laxative use.