Semester One 2015 OSCE Feedback
advertisement

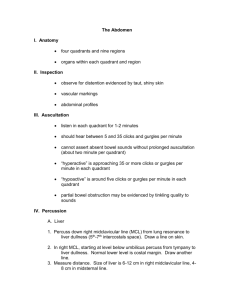
Semester One 2015 OSCE Feedback Physical examination station: Gastrointestinal Examination Pass mark: 25/40 In general, students performed well. Instructions to the patients were clear, and patients were asked if they had pain in their abdomen prior to palpation. The examination was performed systematically, and all facets of the examination were covered. Most students finished the GI examination within the allotted time. There were a few common errors in gastrointestinal examination, and some comments from examiners suggesting areas where technique could be improved: Inspection for spider naevi- many students only checked the anterior chest and neck, instead of the “distribution of the superior vena cava” which includes the back as well. Metabolic flap- many students did not have their patient hold the position for an adequate time. The patient must hold for 15 seconds. Exposure of the abdomen was commonly inadequate- the patients were wearing pants with waistbands at or near the waist, and needed to be asked to pull them down to the hips to expose the lower half of the abdomen. Most students asked the patient to remove their top, but accepted the position of the pants, so inspection and palpation of the lower abdomen was not possible Inspection of the abdomen once the patient was supine was often cursory. Allowing a few breaths to watch the rise and fall of the abdomen provides valuable information in the clinical setting. Superficial and deep palpation of the abdomen was performed systematically but the deep palpation was often too superficial and /or brisk. Watch the patient’s face for any reaction as you palpate for signs of tenderness When feeling for liver and spleen, the hand palpating the anterior abdomen should not move significantly once placed in each position- the organ moves to meet the hand, and the hand is repositioned between breaths. (Similarly for the kidneys, the anterior hand palpates deeply but holds a steady position and waits for the posterior hand to move the kidney towards it.) If the “watching” hand is moving, there is too much sensation to the hand from the movement to accurately feel the liver/ spleen/kidney if it also meets the hand. Palpation of the liver was generally well performed, but measurement of liver span was often performed in the wrong place. The span should be measured in the midclavicular line, but it was frequently percussed too medially, so the liver span appeared to be unusually small. The palpation of the spleen was generally timed with inspiration but many students did not have their hand parallel to the costal margin. In palpation of the kidneys, it is important to have the anterior hand under the costal margin, and place so you are feeling for the kidney with the fingers and not the heel of the hand. Push the kidney anteriorly by flexing the metacarpophalangeal joints of the hand placed posteriorly in the renal angle. Examiner question - When answering the question about the features of chronic liver disease in a male patient many students were not systematic in their answer. A suggestion would be to consider the signs as though you are examining this patient. e.g. Features of general inspection then features in the hands, face, chest and abdomen. i.e jaundice, palmar erythema, Dupuytren’s contracture and leuconychia, icteric sclera, spider naevi, gynaecomastia and features in the abdomen e.g., distention due to ascites, caput medusae, etc. Interview station: Chest Pain Interview Pass mark: 24 /40 This station was done well, with students approaching the case in a systematic manner. Your listening and questioning skills were generally of a high standard. Some possible areas for improvement include the following: If patient unable to describe the pain offer a ‘menu’ of adjectives Always ask about the severity of pain and use the scale of 1 – 10 Always ask about chronology of the pain - including the duration of each episode of pain and the pattern of the episodes over time Remember to ask about the associated features of chest pain including shortness of breath, nausea, sweating, and collapse Ask about past history of heart disease Listen carefully to the examiner question regarding the features of the pain rather than listing risk factors for heart disease