Click Here to - Orthopedic Stem Cell Institute
advertisement

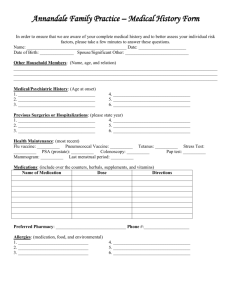
HISTORY AND PHYSICAL (Please complete carefully and thoroughly) NAME: ___________________________________ AGE__________ BIRTH DATE________________ HEIGHT ___________________WEIGHT________________ REVIEW OF SYMPTOMS (circle any of these symptoms you many have had in the past year) GENERAL: Poor appetite, weight change HEAD: Headaches EYES: Blurred or double vision THROAT: Chronic sore throats, difficulty swallowing MOUTH: Loose of false teeth, dental problems LUNGS: Shortness of breath, chronic cough Weakness in paralysis HEART: HAVE YOU EVER HAD A BLOOD TRANSFUSION? NO YES ABDOMEN: GU: NEUROLOGIC Chest Pain, heart pounding, swollen ankles/hands Nausea, vomiting, change in bowel habits, blood in stool, recurrent indigestion, abdomen pain Frequent urination, pain or burning with urination Headaches, numbness/tingling in hands/feet frequent falls, dizziness, burning in hands or feet PAST MEDICAL HISTORY (circle if you have ever had any of the following) Anemia Epilepsy/Seizure Lung Disease/COPD Diabetes/Adult/Child Anxiety/Depression Fibromyalgia Multiple Sclerosis Insulin Dependent Arthritis Hard of Hearing Nervous Breakdown Emphysema Blood Clots in Legs/Lungs Heart Disease Pneumonia Jaundice Bowel Disease Hernia-Hiatal/Other Polio Kidney Disease Breast cysts or lumps Hepatitis Poor Vision Liver Disease Bleeding Disorder High Blood Pressure Rheumatic Fever Tuberculosis Chronic Bronchitis High Cholesterol/Triglycerides Skin Disease Ulcers Dizziness HIV Thyroid Problems MRSA Sleep Apnea Cancer Gout Other____________________________ CARDIAC HISTORY Have you ever been treated for a heart problem? YES NO Name and Number of cardiologist: __________________________________ Last visit/EKG _________________________________ FAMILY HISTORY Maternal or Paternal Blood Disease Heart Attack Cancer Diabetes Tuberculosis Problems with Anesthesia Lung Disease Birth Defects Liver Disease Kidney Disease History of Drug or Alcohol abuse? ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ YES NO SOCIAL HISTORY Do you smoke cigarettes? Packs/Day Have you ever smoked cigarettes? When did you stop? Do you chew tobacco? Do you use “street” drugs? Do you drink alcohol daily? Have you ever taken Cortisone? Any problems with Anesthesia? Are you LEFT or RIGHT handed? YES NO ______ YES NO ______ YES NO YES NO YES NO YES NO YES NO R L LIST ALL MEDICATIONS YOU ARE CURRENTLY Do you use medical marijuana? YES NO TAKING OR HAVE TAKEN OVER THE PAST YEAR LIST ALL KNOWN ALLERGIES/REACTIONS Name/Strength/Frequency _____________________________________________ _____________________________________________ _____________________________________________ _____________________________________________ __________________________________________________ __________________________________________________ __________________________________________________ __________________________________________________ __________________________________________________ LIST ALL MAJOR OPERATIONS, INJURIES, OR CHRONIC ILLNESSES DATE TYPE OF INJURY OR ILLNESS ______________ __________________________________________________________________ ______________ __________________________________________________________________