Acid Base Balance Interactive Tutorial
advertisement

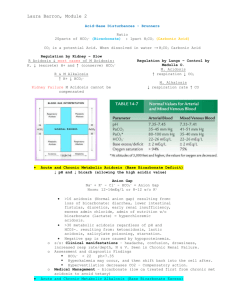
Acid-Base Balance Interactive Tutorial Emily Phillips MSN 621 Spring 2009 E-mail: emmalemmaRN@hotmail.com All images imported from Microsoft Clipart & Yahoo Image gallery How to navigate this tutorial: To advance to the next slide click on the box To return to the previous slide click on the box To return to the Main Menu: click the box Hover over underlined text for a definition/explanation To return to the last slide viewed click on the button Click the for additional information Objectives: Define acid base balance/imbalance Explain the pathophysiology of organs involved in acid base balance/imbalance Identify normal/abnormal and compensated/uncompensated lab values Explain symptoms related to acid base imbalances and compensated vs. uncompensated Appropriate interventions and expected outcomes Main Menu: Acid-Base Pretest The Buffer Systems Acid-Base Review test Metabolic Distubances Respiratory Disturbances Acid-Base Compensation Diagnostic Lab Values ABG Interpretation & Case Studies Acid-Base Pretest: What is the normal range for arterial blood pH? 7.38 – 7.46 7.40 – 7.52 7.35 – 7.45 Acid-Base Pretest: What 2 extracellular substances work together to regulate pH? Sodium bicarbonate & carbonic acid Carbonic acid & bicarbonate Acetic acid & carbonic acid Acid-Base Pretest: Characterize an acid & a base based on the choices below. Acids release hydrogen (H+) ions & bases accept H+ ions. Acids accept H+ ions & bases release H+ ions Both acids & bases can release & accept H+ ions Acid-Base Pretest: Buffering is a normal body mechanism that occurs rapidly in response to acidbase disturbances in order to prevent changes in what? HCO3- H2CO3 H+ Acid-Base Pretest: What are the two systems in the body that work to regulate pH in acid-base balance & which one works fastest? The Respiratory & Renal systems Renal The Respiratory & Renal systems Respiratory The Renal & GI systems Renal Acid-Base Balance: Homeostasis of bodily fluids at a normal arterial blood pH pH is regulated by extracellular carbonic acid (H2CO3) and bicarbonate (HCO3-) Acids are molecules that release hydrogen ions (H+) A base is a molecule that accepts or combines with H+ ions Acids and Bases can be strong or weak: A strong acid or base is one that dissociates completely in a solution - HCl, NaOH, and H2SO4 A weak acid or base is one that dissociates partially in a solution -H2CO3, C3H6O3, and CH2O The Body and pH: Homeostasis of pH is controlled through Protein Buffer system HCO3Buffer system K+ - H+ Exchange extracellular & intracellular buffering systems Respiratory: eliminate CO2 Renal: conserve HCO3- and eliminate H+ ions Electrolytes: composition of extracellular (ECF) & intracellular fluids (ICF) - ECF is maintained at 7.40 Quick Review: Click the Boxes A donator of H+ ions An Acid is: w/ pH <7.0 An acceptor of H+ A Base is: ions w/ pH >7.0 Regulated by EC pH is: H2CO3 & HCO3 Controlled by EC pH is: & IC buffer systems Eliminates CO2 Conserves HCO3Renal System: Eliminates H+ ions Respiratory System: Respiratory Control Mechanisms: Works within minutes to control pH; maximal in 12-24 hours Only about 50-75% effective in returning pH to normal Excess CO2 & H+ in the blood act directly on respiratory centers in the brain CO2 readily crosses blood-brain barrier reacting w/ H2O to form H2CO3 H2CO3 splits into H+ & HCO3- & the H+ stimulates an increase or decrease in respirations Renal Control Mechanisms: Don’t work as fast as the respiratory system; function for days to restore pH to, or close to, normal Regulate pH through excreting acidic or alkaline urine; excreting excess H+ & regenerating or reabsorbing HCO3 Excreting acidic urine decreases acid in the EC fluid & excreting alkaline urine removes base H+ elimination & HCO3conservation Mechanisms of Acid-Base Balance: The ratio of HCO3- base to the volatile H2CO3 Phosphate Buffer system Ammonia Buffer system determines pH Concentrations of volatile H2CO3 are regulated by changing the rate & depth of respiration Plasma concentration of HCO3- is regulated by the kidneys via 2 processes: reabsorption of filtered HCO3- & generation of new HCO3-, or elimination of H+ buffered by tubular systems to maintain a luminal pH of at least 4.5 Acid-Base Balance Review test: The kidneys regulate pH by excreting HCO3- and retaining or regenerating H+ TRUE FALSE Acid-Base Review test: H2CO3 splits into HCO3- & H+ & it is the H+ that stimulates either an increase or decrease in the rate & depth of respirations. TRUE FALSE Acid-Base Review test: Plasma concentration of HCO3- is controlled by the kidneys through reabsorption/regeneration of HCO3-, or elimination of buffered H+ via the tubular systems. TRUE FALSE Acid-Base Review test: The ratio of H+ to HCO3- determines pH. TRUE FALSE Acid-Base Review test: Secreted H+ couples with filtered HCO3- & CO2 & H2O result. TRUE FALSE Metabolic Disturbances: Alkalosis: elevated HCO3- (>26 mEq/L) Causes include: Cl- depletion (vomiting, prolonged nasogastric suctioning), Cushing’s syndrome, K+ deficiency, massive blood transfusions, ingestion of antacids, etc. Acidosis: decreased HCO3- (<22 mEq/L) Causes include: DKA, shock, sepsis, renal failure, diarrhea, salicylates (aspirin), etc. Compensation is respiratory-related Metabolic Alkalosis: Caused by an increase in pH (>7.45) related to an excess in plasma HCO3 Caused by a loss of H+ ions, net gain in HCO3- , or loss of Cl- ions in excess of HCO3- Most HCO3- comes from CO2 produced during metabolic processes, reabsorption of filtered HCO3-, or generation of new HCO3- by the kidneys Proximal tubule reabsorbs 99.9% of filtered HCO3-; excess is excreted in urine Metabolic Alkalosis Manifestations: Signs & symptoms (s/sx) of volume depletion or hypokalemia Compensatory hypoventilation, hypoxemia & respiratory acidosis Neurological s/sx may include mental confusion, hyperactive reflexes, tetany and carpopedal spasm Severe alkalosis (>7.55) causes respiratory failure, dysrhthmias, seizures & coma Treatment of Metabolic Alkalosis: Correct the cause of the imbalance May include KCl supplementation for K+/Cldeficits Fluid replacement with 0.9 normal saline or 0.45 normal saline for s/sx of volume depletion Intubation & mechanical ventilation may be required in the presence of respiratory failure Metabolic Acidosis: Primary deficit in base HCO3- (<22 mEq/L) and pH (<7.35) Caused by 1 of 4 mechanisms Increase in nonvolatile metabolic acids, decreased acid secretion by kidneys, excessive loss of HCO3-, or an increase in Cl- Metabolic acids increase w/ an accumulation of lactic acid, overproduction of ketoacids, or drug/chemical anion ingestion Metabolic Acidosis Manifestations: Hyperventialtion (to reduce CO2 levels), & dyspnea Complaints of weakness, fatigue, general malaise, or a dull headache Pt’s may also have anorexia, N/V, & abdominal pain If the acidosis progresses, stupor, coma & LOC may decline Skin is often warm & flush related to sympathetic stimulation Treatment of Metabolic Acidosis: Treat the condition that first caused the imbalance NaHCO3 infusion for HCO3- <22mEq/L Restoration of fluids and treatment of electrolyte imbalances Administration of supplemental O2 or mechanical ventilation should the respiratory system begin to fail Quick Metabolic Review: Metabolic disturbances indicate an excess/deficit in HCO3- (<22mEq/L or >26mEq/L Reabsorption of filtered HCO3- & generation of new HCO3- occurs in the kidneys Respiratory system is the compensatory mechanism ALWAYS treat the primary disturbance Respiratory Disturbances: Alkalosis: low PaCO2 (<35 mmHg) Caused by HYPERventilation of any etiology (hypoxemia, anxiety, PE, pulmonary edema, pregnancy, excessive ventilation w/ mechanical ventilator, etc.) Acidosis: elevated PaCO2 (>45 mmHg) Caused by HYPOventilation of any etiology (sleep apnea, oversedation, head trauma, drug overdose, pneumothorax, etc.) Compensation is metabolic-related Respiratory Alkalosis: Characterized by an initial decrease in plasma PaCO2 (<35 mmHg) or hypocapnia Produces elevation of pH (>7.45) w/ a subsequent decrease in HCO3- (<22 mEq/L) Caused by hyperventilation or RR in excess of what is necessary to maintain normal PaCO2 levels Respiratory Alkalosis Manifestations: S/sx are associated w/ hyperexcitiability of the nervous system & decreases in cerebral blood flow Increases protein binding of EC Ca+, reducing ionized Ca+ levels causing neuromuscular excitability Lightheadedness, dizziness, tingling, numbness of fingers & toes, dyspnea, air hunger, palpitations & panic may result Treatment of Respiratory Alkalosis: Always treat the underlying/initial cause Supplemental O2 or mechanical ventilation may be required Pt’s may require reassurance, rebreathing into a paper bag (for hyperventilation) during symptomatic attacks, & attention/treatment of psychological stresses. Respiratory Acidosis: Occurs w/ impairment in alveolar ventilation causing increased PaCO2 (>45 mmHg), or hypercapnia, along w/ decreased pH (<7.35) Associated w/ rapid rise in arterial PaCO2 w/ minimal increase in HCO3- & large decreases in pH Causes include decreased respiratory drive, lung disease, or disorders of CW/respiratory muscles Respiratory Acidosis Manifestations: Elevated CO2 levels cause cerebral vasodilation resulting in HA, blurred vision, irritability, muscle twitching & psychological disturbances If acidosis is prolonged & severe, increased CSF pressure & papilledema may result Impaired LOC, lethargy/coma, paralysis of extremities, warm/flushed skin, weakness & tachycardia may also result Treatment of Respiratory Acidosis: Treatment is directed toward improving ventilation; mechanical ventilation may be necessary Treat the underlying cause Drug OD, lung disease, chest trauma/injury, weakness of respiratory muscles, airway obstruction, etc. Eliminate excess CO2 Quick Respiratory Review: Caused by either low or elevated PaCO2 levels (<35 or >45mmHg) Watch for HYPOventilation or HYPERventilation; mechanical ventilation may be required Kidneys will compensate by conserving HCO3- & H+ REMEMBER to treat the primary disturbance/underlying cause of the imbalance Compensatory Mechanisms: Adjust the pH toward a more normal level w/ out correcting the underlying cause Respiratory compensation by increasing/decreasing ventilation is rapid, but the stimulus is lost as pH returns toward normal Kidney compensation by conservation of HCO3- & H+ is more efficient, but takes longer to recruit Metabolic Compensation: Results in pulmonary compensation beginning rapidly but taking time to become maximal Compensation for Metabolic Alkalosis: HYPOventilation (limited by degree of rise in PaCO2) Compensation for Metabolic Acidosis: HYPERventilation to decrease PaCO2 Begins in 1-2hrs, maximal in 12-24 hrs Respiratory Compensation: Results in renal compensation which takes days to become maximal Compensation for Respiratory Alkalosis: Kidneys excrete HCO3- Compensation for Respiratory Acidosis: Kidneys excrete more acid Kidneys increase HCO3- reabsorption DIAGNOSTIC LAB VALUES & INTERPRETATION Normal Arterial Blood Gas (ABG) Lab Values: Arterial pH: 7.35 – 7.45 HCO3-: 22 – 26 mEq/L PaCO2: 35 – 45 mmHg TCO2: 23 – 27 mmol/L PaO2: 80 – 100 mmHg SaO2: 95% or greater (pulse ox) Base Excess: -2 to +2 Anion Gap: 7 – 14 Acid-Base pH and HCO3 Arterial pH of ECF is 7.40 Acidemia: blood pH < 7.35 (increase in H+) Alkalemia: blood pH >7.45 (decrease in H+) If HCO3- levels are the primary disturbance, the problem is metabolic Acidosis: loss of nonvolatile acid & gain of HCO3Alkalosis: excess H+ (kidneys unable to excrete) & HCO3- loss exceeds capacity of kidneys to regenerate Acid-Base PCO2, TCO2 & PO2 If PCO2 is the primary disturbance, the problem is respiratory; it’s a reflection of alveolar ventilation (lungs) PCO2 increase: hypoventilation present PCO2 decrease: hyperventilation present TCO2 refers to total CO2 content in the blood, including CO2 present in HCO3 >70% of CO2 in the blood is in the form of HCO3PO2 also important in assessing respiratory function Base Excess or Deficit: Measures the level of all buffering systems in the body – hemoglobin, protein, phosphate & HCO3 The amount of fixed acid or base that must be added to a blood sample to reach a pH of 7.40 It’s a measurement of HCO3- excess or deficit Anion Gap: The difference between plasma concentration of Na+ & the sum of measured anions (Cl- & HCO3-) Representative of the concentration of unmeasured anions (phosphates, sulfates, organic acids & proteins) Anion gap of urine can also be measured via the cations Na+ & K+, & the anion Cl- to give an estimate of NH4+ excretion Anion Gap The anion gap is increased in conditions such as lactic acidosis, and DKA that result from elevated levels of metabolic acids (metabolic acidosis) A low anion gap occurs in conditions that cause a fall in unmeasured anions (primarily albumin) OR a rise in unmeasured cations A rise in unmeasured cations is seen in hyperkalemia, hypercalcemia, hypermagnesemia, lithium intoxication or multiple myeloma Sodium Chloride-Bicarbonate Exchange System and pH: The reabsorption of Na+ by the kidneys requires an accompanying anion - 2 major anions in ECF are Cl- and HCO3 One way the kidneys regulate pH of ECF is by conserving or eliminating HCO3- ions in which a shuffle of anions is often necessary Cl- is the most abundant in the ECF & can substitute for HCO3- when such a shift is needed. Acid-Base Interpretation Practice: Please use the following key to interpret the following ABG readings. Click on the blue boxes to reveal the answers Use the button to return to the key at any time Or use the “Back to Key” button at the bottom left of the screen Acid-Base w/o Compensation: Parameters: pH PaCO2 Metabolic Alkalosis Normal Metabolic Acidosis Normal Respiratory Alkalosis Respiratory Acidosis HCO3- Normal Normal Interpretation Practice: pH: 7.31 Resp. Acidosis Right! PaCO2: 48 Resp. Try Alkalosis Again HCO3-: 24 Try Again Metabolic Acidosis pH: 7.47 Resp.Again Alkalosis Try Metabolic Alkalosis Right! Metabolic Acidosis Try Again PaCO2 : 45 HCO3- : 33 Back to Key Interpretation Practice: pH: 7.20 HCO3-: 14 Try Again Metabolic Alkalosis Try Again Resp. Acidosis Metabolic Right! Acidosis pH: 7.50 Try Again Metabolic Alkalosis PaCO2 : 29 Right! Resp. Alkalosis Resp.Again Acidosis Try PaCO2: 36 HCO3- -: 22 Back to Key Acid-Base Fully Compensated: Parameters: pH Metabolic Alkalosis Normal >7.40 Metabolic Acidosis Normal <7.40 Respiratory Alkalosis Respiratory Acidosis Normal >7.40 Normal <7.40 PaCO2 HCO3- Interpretation Practice: pH: 7.36 PaCO2: 56 Compensated Resp. Alkalosis Try Again Compensated Metabolic Acidosis Try Again HCO3-: 31.4 Right!Resp. Acidosis Compensated pH: 7.43 Compensated Resp. Alkalosis Right! PaCO2 : 32 Compensated Metabolic Alkalosis Try Again HCO3: 21 Try Again Compensated Metabolic Acidosis Back to Key Acid-Base Partially Compensated: Parameters: Metabolic Alkalosis Metabolic Acidosis Respiratory Alkalosis Respiratory Acidosis pH PaCO2 HCO3- Interpretation Practice: pH: 7.47 Partially Compensated Metabolic Alkalosis HCO3-: 33.1 Right! PartiallyTry Compensated Again Resp. Alkalosis Partially Compensated Try AgainMetabolic Acidosis pH: 7.33 Partially Compensated Try AgainMetabolic Alkalosis PaCO2: 49 PaCO2 : 31 PartiallyTry Compensated Again Resp. Acidosis HCO3- : 16 Right! Metabolic Acidosis Partially Compensated Back to Key Case Study 1: Mrs. D is admitted to the ICU. She has missed her last 3 dialysis treatments. Her ABG reveals the following: pH: 7.32 PaCO2: 32 HCO3-: 18 The=pH is: Low, WNL 7.35-7.45 The PaCO Low, WNL = 35-45mmHg 2 is: The HCO Low, WNL = 22-26mEq/L 3 is: Assess the pH, PaCO2 & HCO3-. Are the values high, low or WNL? Case Study 1 Continued: What is Mrs. D’s acid-base imbalance? Partially Compensated Right!Metabolic Acidosis Try Again Fully Compensated Resp. Acidosis Remember the difference between full & partial compensation. Go back & use the appropriate key if necessary. Case Study 2: Mr. M is a pt w/ chronic COPD. He is admitted to your unit pre-operatively. His admission lab work is as follows: pH: 7.35 PaCO2: 52 HCO3-: 50 The pH is: WNL = 7.35-7.45 The PaCO High, WNL = 35-45mmHg 2 is: The HCO High, WNL = 22-26mEq/L 3 is: Assess the above labs. Are they abnormal or WNL? Case Study 2 Continued: What is Mr. M’s acid-base disturbance? Fully Compensated Metabolic Acidosis Try Again Fully Compensated Right!Resp. Acidosis Think about appropriate interventions- if the problem is metabolic, the respiratory system compensates & vice versa Case Study 3: Miss L is a 32 year old female admitted w/ decreased LOC after c/o the “worst HA of her life.” She is lethargic, but arouseable; diagnosed w/ a SAH. Her ABG reads: pH: 7.48 PaCO2: 32 HCO3-: 25 The=pH is: High; WNL 7.35-7.45 The PaCO Low; WNL = 35-45mmHg 2 is: The HCO High; WNL = 22-26mEq/L 3 is: What is the significance of her ABG values? Case Study 3 Continued: What is Miss L’s imbalance? Resp. Alkalosis Right! Try Again Metabolic Alkalosis Great Job! You’ve reached the end of the tutorial & I hope you found it helpful. Thank you! REFERENCES: http://www.healthline.com/galecontent/acid-basebalance?utm_medium=ask&utm_source=smart&utm_campaign=article &utm_term=Acid+Base+Equilibrium&ask_return=Acid-Base+Balance. Retrieved 3/5/09. Porth, C.M. (2005). Pathophysiology Concepts of Altered Health States (7th ed.). Philadelphia: Lippincott Williams & Wilkins. http://en.wikipedia.org/wiki/Dissociation_(chemistry). Retrieved 3/6/09. http://www.clt.astate.edu/mgilmore/pathophysiology/Acid and Base.ppt#1. Retrieved 3/6/09. http://www.uhmc.sunysb.edu/internalmed/nephro/webpages/Part_E.htm. Retrieved 3/6/09. http://medical-dictionary.thefreedictionary.com/Volatile+acid. Retrieved 3/6/09. REFERENCES http://wiki.answers.com/Q/How_does_the_phosphate_buffer_system_help_ in_maintaining_the_ph_of_our_body. Retrieved 3/10/09. Alspach, J.G. (1998). American Association of Critical-Care Nurses Core Curriculum for Critical Care Nursing (5th ed.). Philadelphia: Saunders. http://medical-dictionary.thefreedictionary.com. Retrieved 4/14/09. Acid-Base Balance & Oxygenation Power Point. (2007). Milwaukee: Froedtert Lutheran Memorial Hospital Critical Care Class.