Project GREAT: Bringing Consumerism to Mental Health Education
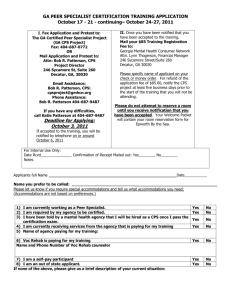
advertisement
Project GREAT: Bringing Consumerism to Mental Health Education and Services Department of Psychiatry and Health Behavior Medical College of Georgia, Augusta, GA Gareth Fenley, MSW Certified Peer Specialist Alex Mabe, PhD Professor and Chief of Psychology Joseph S. Ricci, PhD Administrative Director “…the mental health delivery system is fragmented and in disarray.” Source: New Freedom Commission on Mental Health (2003). Achieving the promise: Transforming mental health care in America. Final Report. DHHS Pub No. SMA-03-3832, Rockville, MD. Mental Illness Affects People in the Prime of Their Lives Half of the lifetime cases of mental illness begin by age 15 and three-quarters by age 24 About half of Americans will meet criteria for a DSM-IV Disorder in their lifetime. Kessler, et al., 2005 Use of Mental Health Services- Adults Between 2001 and 2003, 60 percent of individuals with a mental disorder got no treatment National Comorbidty Survey Replication Study- Wang et al., 2005 Use of Mental Health Services- Serious Mental Illness 55 percent stated that they had not received services because they did not need it. National Comorbidty Survey Study- Kessler et al., 2001 Use of Mental Health Services Delays in making treatment contact range from 6-8 years for mood disorders and 6-23 years for anxiety disorders. 10% dropout by the 5th visit, 18% by the 10th visit, 20% by the 25th visit. National Comorbidty Survey Replication Study- Wang et al., 2005 National Comorbidty Survey Study- Edlund et al., 2002 Medication Regimen Adherence Noncompliance rates well over 50% for most medication treatments of major psychiatric disorders – often not detected by the provider. 100 90 80 70 60 50 40 30 20 10 0 1980 Area Line Line Line Line Line 1990 2000 2006 Access to High Quality Care In the National Comorbidity Study: 78.2 % of mood disorders and 95.9% among nonaffective psychoses did not receive minimally adequate mental health treatment •Wang, Berglund, & Kessler, 2000 1 6 5 4 3 2 Have Psychiatrists Become Medication Managers? From 1987 to 1997: Percent of patients receiving medications doubled. Average number of visits declined from 12.6 to 8.7. •Olfson et al., 2002 Traditional Psychiatric Care Case Vignette Stigma Surgeon General’s Report on Mental Health of 1999, “…despite unprecedented knowledge gained in just the past three decades about brain and human behavior, mental health is often an afterthought and illnesses of the mind remain shrouded in fear and misunderstanding.” Stigma National survey data indicate that 75 percent of the public views individuals with mental illness as dangerous. This negative view has been influenced by negative images of psychosis, poor social skills, poor personal appearance. Stigma is worse for schizophrenia versus depression. Stigma- Mental Health Care People with mental illness often internalize negative attitudes toward those with mental illness, resulting in reluctance to seek and/or maintain adequate mental health care. Recovery and Project GREAT “Houses” by an unnamed child from Vienna Buzz Aldrin - Astronaut The Recovery Model of mental health care …represents a convergence of data and theory and a consumer-driven movement that all clearly point to the enormous benefits of giving individuals a sense of self-determination in their own health and well-being. The Recovery Model Transcends the exclusive focus on symptom reduction that marks the traditional medical model. Instills hope while emphasizing a non-linear process of recovery that includes setback and challenges. Recognizes that people living with mental illness have strengths, goals, and dreams to be honored. Emphasizes holistic and individualized care. Defines recovery as what the patient does. The Recovery Model Insists that health care is to be collaborative. It is a partnership, more like midwifery than surgery, but perhaps characterized best in the words of The Home Depot, “You can do it. We can help.” Used with permission of Larry Davidson, Ph.D. Davidson, L. (2007, January). Recovery and serious mental illness: What it is and how to promote it. Presentation at the Medical College of Georgia Psychiatry Grand Rounds (January 11, 2007). The Essence of the Recovery Model of Mental Health Care Self-Determination Self-Efficacy Support Diane Arbus - Photographer Project G.R.E.A.T. (Georgia Recovery-Based Educational Approach to Treatment) System transformation to a Recovery model of care through teaching and dissemination. Funded by the Georgia Department of Human Resources, Division of Mental Health, Developmental Disabilities, and Addictive Diseases with special assistance by the Carter Center in Atlanta. Project G.R.E.A.T. The Team Peter F. Buckley, MD Gareth Fenley, MSW P. Alex Mabe, PhD Scott A. Peebles, PhD Project G.R.E.A.T. The Goals To transform an academic department into a Recovery Model program. To disseminate the Recovery Model to mental health agencies and medical schools throughout Georgia and beyond. Project G.R.E.A.T. The Challenges “If it ain’t broke, don’t fix it” attitude. Fears that the Recovery Model would infringe on the best practices in traditional care. Time constraints. Stigmatizing attitudes. No administrative precedent for a Certified Peer Specialist. No consumer presence on hospital/clinic advisory boards. Tom Harrell - Jazz Musician Project Great: Defining and Refining as we go. Phase I: Bringing on a Certified Peer Specialist. A “Peer Specialist” or “Peer Support Specialist”: Manages his or her own life with mental illness Provides mental health services to others with mental illness (peers) Winning against Ongoing Challenges The peer specialist May have been disabled by the most severe diagnoses (schizophrenia, PTSD, etc.) May also be in recovery from co-occurring substance abuse May experience continuing symptoms of mental illness The Peer Specialist’s Role Part of a multidisciplinary team Does not treat symptoms Offers role modeling and teaching about Recovery The Georgia Certified Peer Specialist (CPS) Program High school diploma or GED required Competitive admissions process Two-week training Certification exam Continuing education Peer Support in Georgia First ever rewarded with Medicaid reimbursement Has trained residents of 13 US states and Canada 300+ Georgians certified The leading curriculum for peer specialist training internationally Project GREAT and the CPS Project Intimately linked from the beginning Hiring a CPS to join the MCG staff was planned from the outset Several CPSs collaborated to advise MCG on a Steering Committee and in focus groups during the creation of the plan Institutional Barriers Obtaining administrative clearance to hire the CPS took a year after grant funding began CPS credential is not recognized by MCG hospital administration CPS is unable to view medical records or access scheduling system CPS has hospital privileges similar to a volunteer but is full-time paid staff expected to collaborate with clinical treatment teams Opportunities and Challenges Faculty, staff, and residents at all levels have welcomed the CPS Expressed attitudes toward CPS on team have been positive A handful of MDs have made most of the referrals (mostly inpatients who may be difficult to follow up with as outpatients) Many providers have expressed willingness to refer to CPS services, but puzzlement over how the process works Dr. Kay Redfield Jamison- Psychologist, Scientist and Author Project Great: Defining and Refining as we go. Phase II: Developing a Behavioral Health Advisory Council Lunatics Running The Asylum? (Is there a place for PFCC in Mental Health?) Psychiatric patients are traditionally seen as unable to collaborate in their own care due to mental impairment Many family members have been encouraged to surrender care decisions entirely to professionals and even to consider some loved ones “dead” Patient and Family Advisors in Mental Health: Unique Challenges Physical logistics (locked units, unmarked locations) Procedural logistics (heightened confidentiality, separate and often lesser insurance benefits) Funding STIGMA Affecting patients Affecting families Affecting care providers MCG’s Commitment Vision: To be a national leader in patient and family centered teaching, research and care PFCC inaugurated in children’s medical center MCG featured in PBS series “Remaking American Medicine” Under leadership of VP Patricia Sodomka, FACHE, expanding PFCC to entire MCG enterprise Top Level Departmental Leadership has attended meeting and supported the enterprise. MCG’s Behavioral Health Advisory Council Patient and family members referred by clinicians Active participation by psychiatry faculty, staff, and administrators CPS – Serves as the Facilitator Meets monthly. Minutes and policy recommendations distributed to all members of the council and targeted faculty, staff, and administrators. Topics Tackled by the Council Billing procedures Reminder calls and letters Interior decoration/renovation Involving kids in policy making Transition to tobacco free campus Inpatient programming/volunteering Patient and family info leaflet Feedback on patient and family experiences Sigmund Freud – Psychiatrist, Scientist Project Great: Defining and Refining as we go. Phase III: Developing workshops to immerse psychology and psychiatry faculty and students in the Recovery Model of Mental Health Care. Workshop I: Knowledge, Attitudes, and Behavior Active learning is more effective. Expose the learner to individuals with mental illness that promote a more positive sense of what patients can do for themselves. Build “the case” from relevant and empirically supported data. Provide useable tools. Teach skills, not just knowledge. Natalie Cole - Singer Jack Dreyfus – Business Leader Eleanor Roosevelt – Political Leader The Primacy of Choice and Personal Responsibility: Example of Data Provided Langer and Rodin (1976) – a field study of nursing home residents. For one group it is stressed that their care and well-being is the responsibility of the staff. For the other group it is stressed that they are responsible for themselves. Langer & Rodin (1976) The effect of choice and enhanced personal responsibility for the aged: A field experiment in an institutional setting. J of Personality and Social Psychology, 34, 191-198. The Effects of Choice and Enhanced Responsibility Good care by the staff on behalf of the residents resulted in 71% becoming more debilitated. 93% of the residents given choice and responsibility increased in their functioning. Langer & Rodin (1976) The effect of choice and enhanced personal responsibility for the aged: A field experiment in an institutional setting. J of Personality and Social Psychology, 34, 191-198. Follow-Up Rodin and Langer - 1977 18 months later: Those given choice and responsibility had a 15% mortality rate. Those given care had a 30% mortality rate. Rodin & Langer (1977) Long-term effects of a control-relevant intervention with the institutionalized aged. J of Personality and Social Psychology, 35, 897-902. Georgia Recovery Assessment Form I. Individualized and Person-Centered Treatment Plan (Goals and Objectives) Goal 1: _______________________________________________________________________________________ _______________________________________________________________________________________ New Patient/Family Tasks ____________________________________________________ ___________________________________________________________________________ New Provider Tasks/Responsibility____________________________________________ ___________________________________________________________________________ Goal 2: _______________________________________________________________________________________ _______________________________________________________________________________________ New Patient/Family Tasks ____________________________________________________ ___________________________________________________________________________ New Provider Tasks/Responsibility____________________________________________ ___________________________________________________________________________ Goal 3: _______________________________________________________________________________________ _______________________________________________________________________________________ New Patient/Family Tasks ____________________________________________________ ___________________________________________________________________________ New Provider Tasks/Responsibility____________________________________________ ___________________________________________________________________________ Georgia Recovery Assessment Form - continued II. List Personal Strengths for Patient related to personal goals: 1. 2. 3. III. Systems-based Treatment Plan Is this individual/family appropriate for referral for Peer Support Services? (e.g., Peer Support Specialist, Friendship Community Center, AA, NA, NAMI, Parent-toParent, Bereaved Parents of America, Health Grandparents Project of Augusta) YES NO Would the patient like to participate in Peer Support Services here at MCG? YES NO Would any of the following community support areas be appropriate for consideration in your treatment planning (Please circle appropriate services): Activities/Hobbies Child Care Financial support Health Care Housing Physical fitness Occupational/job support School/Educational Support Spiritual/religious support Substance Abuse Program Transportation Monica Seles – Tennis Champion Workshop II: All about Attitudes Focused on reversing negative stereotypes regarding those individual living with mental illness. Provided “real examples” of individuals “in recovery.” Emphasized the stories and less so the principles. Hearing first hand from providers who have transformed their practice to the Recovery Model. Workshop II clips Ray Charles - Musician Project Great: Defining and Refining as we go. Phase IV: Putting the Recovery Model into Practice. Follow-Up Implementation of the Georgia Recovery Assessment Form Working with PowerNote technical support to make sure that all psychiatry clinical notes have prompts to complete the three key Recovery-Based questions. Putting into Practice - More Putting the Certified Peer Specialist into the game. Keeping the fire under the Behavioral Health Advisory Council. Data Collection. Relaunching the GREAT Steering Committee. Preliminary Findings Workshop I – Knowledge of Recovery significantly improved. Workshop II – Attitudes regarding the capabilities of those with mental illness to actively participate in their care significantly improved. “Lot Easier Said than Done” Where are the referrals for the Certified Peer Specialist? Logistics of incorporating a Certified Peer Specialist into a traditional academic department. Getting administration to listen to the Behavioral Health Advisory Council recommendations. Changing practice habits is hard! Next Steps More data collection, including comparison academic site. Do a consumer needs assessment. Specific data need to move beyond contemplation of change. Identify Recovery Champions among our faculty and residents. Establish participative decision-making: Establish faculty and resident focus groups. Dr. Patricia Deegan and AssociatesClinical Psychologist, Author, and Co-Founder of the National Empowerment Center Inc.