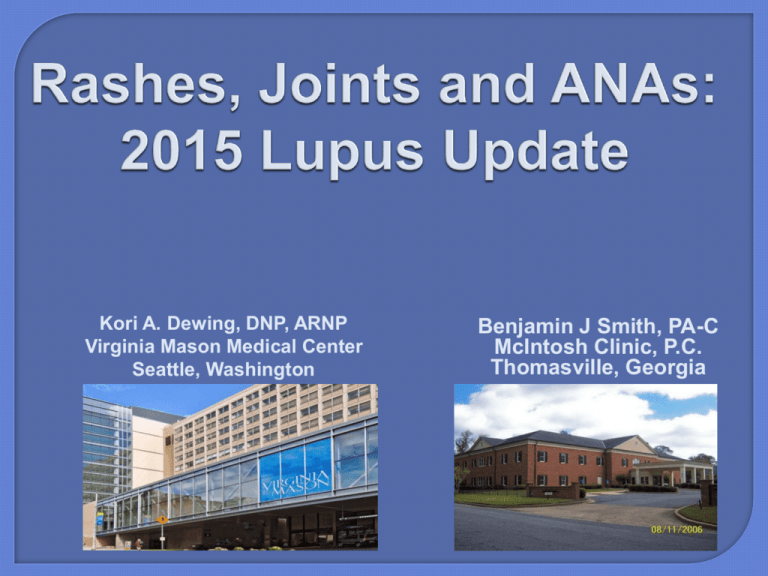
Kori A. Dewing, DNP, ARNP
Virginia Mason Medical Center
Seattle, Washington
Benjamin J Smith, PA-C
McIntosh Clinic, P.C.
Thomasville, Georgia
-Presentation was developed in
collaboration with The Lupus Initiative
http://thelupusinitiative.org/
-No conflicts of interest to disclose
Member, AAPA Commission on
Continuing Professional Development
and Education
3
Disclosure of ABIM Service:
Benjamin J. Smith, PA-C
I am a current member of the Rheumatology Board.
To protect the integrity of certification, ABIM enforces strict
confidentiality and ownership of exam content.
As a current member of the Rheumatology Board, I agree to keep
exam information confidential.
As is true for any ABIM candidate who has taken an exam
for certification, I have signed the Pledge of Honesty in which
I have agreed to keep ABIM exam content confidential.
No exam questions will be disclosed in my presentation.
Upon completion of this session, participants should
be able to:
-Summarize the diagnostic criteria for lupus,
including the American College of Rheumatology
classification criteria.
-Discuss current health disparities that exist for
persons with lupus.
-Select the proper laboratory tests when evaluating a
person with lupus symptoms.
-Describe the currently available therapeutic options
for the treatment of lupus.
1. Which of the following is not
considered part of the current criteria
for classification of systemic lupus
erythematosus:
a. discoid rash.
b. rosacea.
c. serositis.
d. oral ulcers.
2. Which of the following lupus treatments
requires a periodic eye exam?
a. prednisone.
b. azathioprine.
c. hydroxychloroquine.
d. belimumab.
3. Which of the following ANA results is most likely not to
be a false positive result?
a. ≥1:1280, homogenous in a 20 y.o female with joint pain
and 2+ proteinuria.
b. 1:160, speckled in a 85 y.o male with no other symptoms
c. 1:80, speckled in a 32 y.o. female with arthralgia/myalgia,
sleep difficulty and fatigue.
d. 1:40, homogenous in a 35 y.o female with low back pain.
-www.rheumatology.org
-www.uptodate.com
-The Rheumatology Image Bank (http://images.rheumatology.org/)
-The Lupus Initiative (http://thelupusinitiative.org/)
-West, Sterling, M.D. Rheumatology Secrets, 2nd Edition.
Philadelphia: Hanley & Belfus, Inc.; 2002.
- Hochberg MC. Updating the American College of Rheumatology
revised criteria for the classification of systemic lupus
erythematosus [letter]. Arthritis Rheum 1997;40:1725.
-Schur, Peter H. The Rheumatologist. Know Your Labs: Part 1
and 2. February and April 2009.
http://bcove.me/5w0pa1xw
(0:00
to 4:09)
-An inflammatory, multisystem,
autoimmune disease of unknown
etiology with protean clinical and
laboratory manifestations and a
variable course and prognosis
-Lupus can be a mild disease, a
severe and life-threatening illness,
or anything in between
Prevalence: 2–140/100,000 worldwide but as high as 207/100,000
Incidence: 1–10/100,000 worldwide
Population at highest risk:
Women in their reproductive years
Female:male ratio is approximately 9:1 postpuberty and
premenopausal
Variation in race/ethnicity: More common in African American
(3−6x), Hispanic and Native American (2–3x), and Asian (2x)
populations
Cost: There are direct costs associated with treatment
(eg, $100 billion in healthcare cost associated with
autoimmune diseases) and indirect cost related to lost
productivity and wages
Death rates have decreased by 60% in the United States
since the 1970s, especially for infections and renal disease
Risks of death increased in females, Blacks, and
younger-onset patients
Most common causes of death in SLE patients in the
United States
Heart disease and stroke (1.7 x general population)
Hematologic malignancies and lung cancer
(2.1 x general population)
Infections (5 x general population; also a common cause
of hospitalization)
Renal disease (7.9 x general population)
Bernatsky S, Boivin JF, Joseph L, et al. Arthritis Rheum. 2006;54(8):2550-2557.
Upon completion of this session, participants should
be able to:
-Summarize the diagnostic criteria for lupus, including
the American College of Rheumatology classification
criteria.
-Discuss current health disparities that exist for
persons with lupus.
-Select the proper laboratory tests when evaluating a
person with lupus symptoms.
-Describe the currently available therapeutic options
for the treatment of lupus.
-Systemic Lupus Erythematosus
-Cutaneous Lupus Erythematosus
-Drug-induced Lupus Erythematosus
-Neonatal Lupus
Definite — Procainamide, hydralazine, minocycline, diltiazem,
penicillamine, isoniazid, quinidine, anti-tumor necrosis factor
alpha therapy, interferon-alfa, methyldopa, chlorpromazine, and
practolol.
Probable — Anticonvulsants (phenytoin, mephenytoin,
trimethadione, ethosuximide, carbamazepine), antithyroid
drugs, antimicrobial agents (sulfonamides, rifampin,
nitrofurantoin), beta blockers, lithium, paraaminosalicylate,
captopril, interferon gamma, hydrochlorothiazide, glyburide,
carbamazepine, sulfasalazine, terbinafine, amiodarone,
ticlopidine, hydrazine, and docetaxel.
Possible — Gold salts, penicillin, tetracycline, reserpine,
valproate, statins (eg, lovastatin, simvastatin, and atorvastatin)
griseofulvin, gemfibrozil, valproate, lamotrigine, ophthalmic
timolol, and 5-aminosalicylate.
Schur PH, et al. Drug-induced lupus. UpToDate. Accessed 05
May 2014.
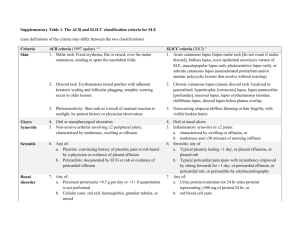
Malar rash
Fixed erythema, flat or raised, sparing the
nasolabial folds
Discoid rash
Raised patches, adherent keratotic scaling,
follicular plugging; older lesions may cause
scarring
Photosensitivity
Skin rash from sunlight
Oral or nasopharyngeal
ulcers
Usually painless
Arthritis
Nonerosive, inflammatory in two or more
peripheral joints
Serositis
Pleuritis or pericarditis
- Hochberg MC. Updating the American College of Rheumatology revised criteria
for the classification of systemic lupus erythematosus [letter]. Arthritis Rheum
1997;40:1725.
Renal disorder
Persistent proteinuria or cellular casts
Neurologic disorder
Seizures or psychosis
Hematologic
Hemolytic anemia, leukopenia (<4,000/mm3),
lymphopenia (<1,500/mm3), or
thrombocytopenia (<100,00/mm3)
Immunologic disorder
Antibodies to dsDNA or SM or positive
antiphospholipid antibodies (IgG or IgM
antibodies, lupus anticoagulant, or falsepositive serologic test positive serologic test
for syphilis)
Antinuclear antibody test
Positive
- Hochberg MC. Updating the American College of Rheumatology revised criteria
for the classification of systemic lupus erythematosus [letter]. Arthritis Rheum
1997;40:1725.
Malar rash
Discoid rash
Photosensitivity
Oral ulcers
Arthritis
Serositis
Renal disorder
Neurologic disorder
Hematologic disorder
Immunologic disorder
Antinuclear antibody
American College of Rheumatology Slide Collection of Rheumatic
Diseases, 3rd Edition, 2004.
Malar rash
Discoid rash
Photosensitivity
Oral ulcers
Arthritis
Serositis
Renal disorder
Neurologic disorder
Hematologic disorder
Immunologic disorder
Antinuclear antibody
American College of Rheumatology Slide Collection of
Rheumatic Diseases, 3rd Edition, 2004.
Malar rash
Discoid rash
Photosensitivity
Oral ulcers
Arthritis
Serositis
Renal disorder
Neurologic disorder
Hematologic disorder
Immunologic disorder
Antinuclear antibody
American College of Rheumatology Slide Collection of Rheumatic
Diseases, 3rd Edition, 2004.
Malar rash
Discoid rash
Photosensitivity
Oral ulcers
Arthritis
Serositis
Renal disorder
Neurologic disorder
Hematologic disorder
Immunologic disorder
Antinuclear antibody
American College of Rheumatology Slide Collection of Rheumatic Diseases,
3rd Edition, 2004.
Malar rash
Discoid rash
Photosensitivity
Oral ulcers
Arthritis
Serositis
Renal disorder
Neurologic disorder
Hematologic disorder
Immunologic disorder
Antinuclear antibody
American College of Rheumatology Slide Collection of Rheumatic
Diseases, 3rd Edition, 2004.
Malar rash
Discoid rash
Photosensitivity
Oral ulcers
Arthritis
Serositis
Renal disorder
Neurologic disorder
Hematologic disorder
Immunologic disorder
Antinuclear antibody
Jaccoud’s arthropathy
-Prevalence: 30%–65% in adults and 80%
in children
-10% annual incidence in 1 large cohort
-More frequent and severe in children,
Blacks, Hispanics, and males
-Strong predictor of morbidity and
mortality
Bastian HM, Roseman JM, McGwin G Jr, et al; LUMINA Study Group. Lupus. 2002;11(3):152-160. Danchenko N, Satia JA, Anthony MS. Lupus. 2006;
15:308-318. Fernández M, Alarcón GS, Calvo-Alén J, et al; LUMINA Study Group. Arthritis Rheum. 2007;57(4):576-584. Hiraki LT, Feldman CH,
Liu J, et al. Arthritis Rheum. 2012;64(8):2669-2676. Patel M, Clarke AM, Bruce IN, et al. Arthritis Rheum. 2006;54(9):2963-2969. Petri M. Lupus.
2005;14(12):970-973.
-Increase in proteinuria is most common
Measured by spot protein:creatinine ratio >0.5 or 24-hour
collection >500 mg/24 hours
The absolute increase in proteinuria that defines a nephritis flare
is arbitrary
-Microscopic abnormalities on urinalysis
White cells or red blood cells >5 cells/hpf in the absence of
infection or other causes
Cellular casts (white cell or red cell)
White cells and red blood cells are seen more frequently than
casts
Hahn BH, McMahon MA, Wilkinson A, et al. Arthritis Care Res (Hoboken). 2012;64(6):797-808.
-19 case definitions of neuropsychiatric manifestations
-Most commonly:
Cognitive dysfunction
Headache
Psychiatric disorders (anxiety, psychosis,* depression)
Seizures*
Stroke (may be associated with antiphospholipid
antibodies)
Peripheral neuropathies
*Part of the classification criteria for SLE.
Bertsias GK, Boumpas DT. Nat Rev Rheumatol. 2010;6:358-367.
Fatigue
Memory thief
Depression
Signs and Symptoms
Symptoms Occurrence (ever)
Arthralgias
95%
Neurologic
90%
Fever >100 °F (38 °C)
90%
Prolonged or extreme fatigue
81%
Arthritis
80%
Skin rashes
74%
Anemia
71%
Kidney involvement
50%
Pleurisy and/or pericarditis
45%
Butterfly-shaped rash across the cheeks and nose
42%
Sun or light sensitivity (photosensitivity)
30%
Hair loss
27%
Abnormal blood clotting problems
20%
Raynaud’s phenomenon
17%
Seizures
15%
Mouth or nose ulcers
12%
Upon completion of this session, participants should
be able to:
-Summarize the diagnostic criteria for lupus,
including the American College of Rheumatology
classification criteria.
-Discuss current health disparities that exist for
persons with lupus.
-Select the proper laboratory tests when evaluating a
person with lupus symptoms.
-Describe the currently available therapeutic options
for the treatment of lupus.
Health disparities are the differences in the
incidence, prevalence, mortality, and
burden of disease and other adverse health
conditions that exist among specific
population groups in the United States
Healthcare disparities refer to differences in
access to or availability of facilities and
services
National Institutes of Health
-Black women are 3 times more likely to develop
lupus than White women
Affects up to 1 in 250 Black women in the
United States
-Hispanic, Asian, and Native American
populations are also more likely to develop
lupus
-Women are 9 times more likely to develop lupus
than men
Helmick CG, Felson DT, Lawrence RC, et al. Arthritis Rheum. 2008;58(1):15-25. Chakravarty EF, Bush TM, Manzi S, Clarke AE, Ward MM.
Arthritis Rheum. 2007;56(6):2092-2094. Fessel WJ. Rheum Dis Clin North Am. 1988;14(1):15-23.
CDC. MMWR Morb Mortal Wkly Rep. 2002;51:371-374.
“The reality is that to get to the root
cause of disparities, it is not going to be
just one factor. For example, poor health
literacy perpetuates health disparities,
as does a lack of access to care, a lack
of access to a regular provider, and a
lack of access to a medical home. No
single factor can be considered to be the
root cause of disparities.”
Anne Beal, Institute of Medicine
Upon completion of this session, participants should
be able to:
-Summarize the diagnostic criteria for lupus,
including the American College of Rheumatology
classification criteria.
-Discuss current health disparities that exist for
persons with lupus.
-Select the proper laboratory tests when evaluating a
person with lupus symptoms.
-Describe the currently available therapeutic options
for the treatment of lupus.
1948---LE cell test (phagocyte with ingested
nucleus)
Hargraves MM. Discovery of the LE cell and its morphology. Mayo Clin Proc.
1969;44:579-99.
Today’s techniques
*Immunofluorescent microscopy
*Immunodiffusion
*Hemagglutination
*Complement fixation
*Solid-phase immunoassay (ELISA or immunoblotting)
*Radioimmunoassays
1948---LE cell test (phagocyte with ingested
nucleus)
Hargraves MM. Discovery of the LE cell and its morphology. Mayo Clin Proc.
1969;44:579-99.
Today’s techniques
*Immunofluorescent microscopy
*Immunodiffusion
*Hemagglutination
*Complement fixation
*Solid-phase immunoassay (ELISA or immunoblotting)
*Radioimmunoassays
ANA Patterns
Peripheral or “rim”
Speckled
Diffuse
Nucleolar
ANA Pattern
Centromere
- 95 - 99% sensitivity for SLE, discoid
(15%), drug induced (100%)
- <1:160 titers less clinically significant
- Titer not a measure of disease activity
-Normal subjects 3%−4%
-SLE 95%−99%
-Scleroderma 95%
-Hashimoto’s thyroiditis 50%
-Idiopathic pulmonary fibrosis 50%
-Incidence increases with age, chronic
infections, and other chronic
conditions
-ds DNA
-SS-A/SS-B
-ENA (Sm, RNP)
-Scl-70
-Other lab….
Depending on
history, exam and
titer
Antibodies
Lupus Specificity
Clinical Associations
ANA
Low
Nonspecific
Anti-dsDNA
High
Nephritis
Anti-Sm
High
Nonspecific
Anti-RNP
Low
Arthritis, myositis, lung disease
Anti-SSA
Low
Dry eyes/mouth, subacute
cutaneous lupus erythematosus
(SCLE), neonatal lupus,
photosensitivity
Anti-SSB
Low
Same as above
Intermediate
Clotting diathesis
Antiphospholipid
-Department of Defense Serum Repository
Serum of 130 persons before SLE dx (matched controls)
Results-115/130---at least one autoantibody before SLE dx (up to 9.4 yrs, mean 3.3 yrs)
-ANA-78% (dilution of ≥1:120)
-dsDNA-55%
-SS-A-47%
-SS-B-34%
3.4 yrs before dx
-Antiphospholipid ab-18%
-Sm-32%
-RNP-26%
Control group---3.8% (+) for one or more autoantibody
1.2 yrs before dx
See also---Heinlen, LD, McClain, MT, Merrill, J, et al. Clinical criteria for systemic lupus
erythematosus precede diagnosis, and associated autoantibodies are present before
clinical symptoms. Arthritis Rheum 2007; 56:2344.
-Autoantibodies
precede diagnosis
by many years
-We are currently not
able to predict which
subjects with
positive
autoantibody
titers will develop
disease
*
**
*Anti-Ro = Anti-SSA
**Anti-La = Anti-SSB
Arbuckle MR, McClain MT, Rubertone MV, et al. N Engl J Med. 2003;349:1526-1533.
CONCLUSION- “Autoantibodies are
typically present many years
before the diagnosis of SLE…”
See also---Heinlen, LD, McClain, MT, Merrill, J, et al. Clinical criteria for systemic lupus
erythematosus precede diagnosis, and associated autoantibodies are present before
clinical symptoms. Arthritis Rheum 2007; 56:2344.
Upon completion of this session, participants should
be able to:
-Summarize the diagnostic criteria for lupus,
including the American College of Rheumatology
classification criteria.
-Discuss current health disparities that exist for
persons with lupus.
-Select the proper laboratory tests when evaluating a
person with lupus symptoms.
-Describe the currently available therapeutic options
for the treatment of lupus.
Eyes
Central nervous
system
Skin
Oral & nasal ulcers
Pleurisy
Kidney
disease
Muscle
Raynaud’s &
vasculitis
Medical Illustration Copyright © 2012. Nucleus Medical Media. All rights reserved.
Pericarditis
Blood
disorders
Joints & arthritis
-Corticosteroids (1955)
-Cyclophosphamide
-Methotrexate
-Mycophenolate mofetil
-Azathioprine
-Hydroxychloroquine (1955)
-Belimumab (2011)
-Aspirin (1948)
http://www.fda.gov/newsevents/newsroom/pressAnnounceme
nts/ucm246489.htm (accessed 22 Apr 2014)
-<6.5mg/kg/day (200mg q day to bid)
-Low toxicity
N/V, Myopathy, caution with Psoriasis
-Retinal toxicity---ophthalmologic exam q 6-12
months
-Pregnancy category-Not rated
Immunosuppressive drugs confer an increased risk for
Infection
Cancer
Infertility
Common side effects of corticosteroids
Infections
Diabetes
Cushingoid appearance
Mood disturbances
Osteoporosis
Hypertension
Osteonecrosis
Lipid abnormalities
Immune targeted therapy
B-cell directed
Cytokine inhibitors
Costimulation blockade
Peptide inhibitors
Kinase inhibitors
T regulatory cells
Stem cell transplant
*
*Recently FDA approved for lupus
Yildirim-Toruner C, Diamond B. J Allergy Clin Immunol. 2011;127:303-312.
Management of risks
Cardiovascular disease
Infection
Fracture
Cancer
Hydroxychloroquine used as a background therapy
Reduce mortality
Decrease incidence of diabetes
Antithrombotic effects
Favorable lipid effects
Broder A, Putterman C. J Rheumatol. 2013;40(1):30-33. Tang C, Godfrey T, Stawell R, Nikpour M. Intern Med J. 2012; Jul 25. [Epub ahead
of print]
Address factors that contribute to a poor outcome
Treat hypertension aggressively
Consider the use of ACE inhibitors and angiotensin II receptor
blockers (ARBs)
Address psychosocial factors
Manage long-term atherosclerosis risks
Prevent adverse effects of medications
Consider prophylaxis for infections
Ensure yearly Pap test and other cancer screening as
clinically indicated
For patients taking cyclophosphamide, interventions to
prevent infertility and bladder toxicity should be considered
Manage bone health
-Education and attention to psychosocial factors
Advise sun protection: year-round use of SPF-45 or higher,
clothing that is UV impenetrable and avoidance of UV
exposure when possible
Encourage weight loss and exercise
Encourage compliance with clinic visits and medications
-Keep vaccinations up to date
-Monitor for early detection of flares
-Minimize steroid use
-Treat cardiac risk factors aggressively
-Monitor bone health
-Uncertain diagnosis
-Confusing Lab Results
-Uncomfortable with treatment
-Patient not responding
-Side effects
Upon completion of this session, participants should
be able to:
-Summarize the diagnostic criteria for lupus,
including the American College of Rheumatology
classification criteria.
-Discuss current health disparities that exist for
persons with lupus.
-Select the proper laboratory tests when evaluating a
person with lupus symptoms.
-Describe the currently available therapeutic options
for the treatment of lupus.
https://www.the-pivot-project.org/
1. Which of the following is not
considered part of the current criteria
for classification of systemic lupus
erythematosus:
a. discoid rash.
b. rosacea.
c. serositis.
d. oral ulcers.
2. Which of the following lupus treatments
requires a periodic eye exam?
a. prednisone.
b. azathioprine.
c. hydroxychloroquine.
d. belimumab.
3. Which of the following ANA results is most likely not to
be a false positive result?
a. ≥1:1280, homogenous in a 20 y.o female with joint pain
and 2+ proteinuria.
b. 1:160, speckled in a 85 y.o male with no other symptoms
c. 1:80, speckled in a 32 y.o. female with arthralgia/myalgia,
sleep difficulty and fatigue.
d. 1:40, homogenous in a 35 y.o female with low back pain.
-The diversity of clinical symptoms in
SLE is great, and all organ systems are
vulnerable.
-A positive ANA is not in and of itself
diagnostic of lupus.
-Hydroxychloroquine is a mainstay for
treating those with lupus.
The simplest tasks
can become
impossible because
of rheumatic
diseases.
www.SimpleTasks.org