Intro To Physiology
Intro To Physiology
Nervous System
Master regulator for the body
Takes sensory input, integrates it, and elicits motor output
Two divisions o CNS
Consists of the brain and the spinal cord
Mostly responsible for integration o PNS
Spinal nerves
Afferent/Sensory
Towards the CNS
Sensory input from sensory receptors
Enters the dorsal side of the spinal cord
No synapses- cell bodies exist in a dorsal root ganglion
Efferent/Motor
Away from the CNS to effectors
Effectors are muscles and glands
Two divisions o ANS (Autonomic NS)
Involuntary
Visceral motor control of glands and smooth muscle
Two divisions
Sympathetic-fight or flight o Synapses right outside the spinal cord in sympathetic trunks o Uses ACH in the first path, Epi or Norepi in the second path
Parasympathetic-rest and digest o Synapses close to the effector organ o Uses ACH for both paths
Both divisions have their first path myelinated while the second path is unmyelinated o Somatic NS
Voluntary motor control
From the CNS to skeletal muscles
Single neuron all myelinated
Uses ACH as the neurotransmitter
Glial cells-non neuronal cells in the nervous system o Many more glial cells than neurons
o Insulation (myelin)
Oligodendrocytes in the CNS
Can wrap more than 1 neuron
Schwann Cells in the PNS
Can only wrap 1 o Protection
Astrocytes
The majority of glial cells
Provide nourishment to the cells
Create the Blood Brain Barrier o Circulation
Ependymal cells
Ciliated
Circulate (do not produce) CSF o CSF is produced by a choroid plexus o Immunity
Microglia
Macrophages
Immune system isn’t allowed into nervous system
Neuron o Dendrites
The receptive region of the neuron
Contains Na and K ion channels to start depolarization
Receives neurotransmitter via receptors
Post synapse
The signal goes electrical, chemical, electrical o Membrane potential
Resting cells are at -70 mv
Action potential brings them to +30
Opening of Na channels brings + charges into the cell
Causes the climb in charge
Depolarization
Repolarization is caused by the delayed opening of the K gated ion channel
(activated at the same time but delayed) allowing K ions out of the cell
Also slow to close, causing hyperpolarization
This has the added benefit of making sure the neuron cant fire too much too fast
Na/K pump restores ion concentrations after
The anions in the cell are mostly responsible for the negative charge
Charges balance out
An electrical equilibrium is created based on the regular charge of the cell, or based on an outside charge (experimentally)
Charges flow to make the charges equal
Add + charge to cell, it wants to decrease the potential so it flows out
Add – charge to cell, it wants to increase the potential so ions flow in
Threshold potential of the neuron is reached at -55 mv
Reached at the axon hillock
-58 mv is the K ion potential equilibrium o Graded potentials
Depolarizes one region of the cell
Can be any level
-34
-24
-85 (so it can even be hyperpolarization)
Etc
The cell region is depolarized yet does not reach threshold at -55 mv
Graded potentials can lead to Action potentials
Can be summed in time or in space
Temporal summation o One after another, they add up
Spatial summation o In the same space, add together o Action potential
Reaches threshold
Generated at the axon hillock
Depolarization due to Na channels opening
Reaches about +30
Then K ion channels open up and there is repolarization
Then hyperpolarization as they are slow to shut
Then the gradient is reestablished by the Na/K pump
Another one cannot be fired for 4-5 ms
Needs to be strong to overcome hyperpolarization
Absolute refractory- nothing can be fired
Relative refractory-only a very strong graded potential will lead to an AP
The number of AP’s determines the stimulus strength o Variables
Size
Increase diameter, the speed increases
Myelination
Myelination increases speed by a lot
Saltatory conduction
o In jumps only to the nodes of ranvier o Makes it so that only at the nodes of ranvier does the AP have to occur o Three types of neurons
Multipolar
Most common
Bipolar
Found only in special senses
Unipolar
Sensory receptors o Three functions
Sensory (afferent)
Motor (efferent)
Interneurons
CNS
Most common (99%)
Neurotransmitters o Diffuse from high to low gradient across the synaptic cleft o IPSP
Inhibitory
Hyperpolarizes
EX: Cl- or GABA o EPSP
Excitatory
Depolarizes
EX: glutamate o EPSP and IPSP can fight each other to try and create (or not create) an AP o The distance from the axon hillock makes a difference, as the depolarization decreases as the distance increases
Terminal bulbs o Ca ion channels (voltage gated) open when the AP reaches, and the influx of Ca pushes vesicles containing NTs to the wall of the terminal bulb o This causes their release into the synapse
Ionotropic receptors o Everything discussed here o Fast
Metabotropic receptors o Use second messengers o Usually G-protein linked o And takes longer due to the second messengers
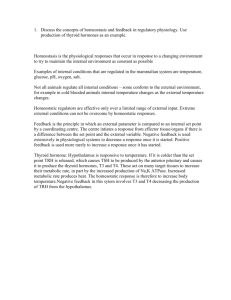
Endocrine System
Method of communication in the body o Use the blood stream o Hormones are long distance
Hypothalamus- top of the pituitary gland- master control
Pituitary-second in command
Lipid soluble hormones can go directly through the bilayer and attach to a receptor inside the cell
Hormones are usually controlled by metabotropic receptors o Their effect takes longer than neurotransmitters
Due to amplification
Target cell activation depends on 3 factors o Number of hormones in the blood o Number of receptors o Affinity for receptors (how tightly they bind)
cAMP second messenger o G s
on a G-protein receptor o Response is amplified o Activates PKA o Hormones that use this cAMP
Cattecholamines
Acth
FSH
LH
Glucagon
PTH
TSH
Calcitonin
Pip second messenger o DAG and IP3 activated Calcium ion release and therefore PKC o Hormones
Catecholamines
TRH
ADH
GnRH
Ocytocin o G q
subuinits
Hormone interactions o Antagonism o Permissiveness o Synergism
Endocrine gland stimulations o Humoral (nutrients in blood) o Hormones o Neuronal
Faster than hormonal
Pituitary gland portal system o Regular portal system is arteriole-capillary-venule o Pituitary portal system is capillary-vein-capillary
Goes quickly from hypothalamus to pituitary
More concentrated hormones in a shorter distance
Speed and concentration
Pituitary o Posterior pituitary
Oxytocin
Made in the paraventricular nuclei of the hypothalamus and sent to the posterior pituitary to be released
ADH
Supraoptic nuclei in the hypothalamus make it o Anterior pituitary
TSH, GH, ACTH, prolactin, LH, FSH
Aneurysm o Saccular-bulb at risk of rupturing o Fusiform-not as dangerous-> longer elongation o Ruptured-broken open
Kidneys o Adh production
Mechanism?
Triggers kidneys to reabsorb water, therefore increasing blood volume and pressure
Based on osmolality
Thyroid hormone o Major metabolic hormone o T3 and T4 (needs IODINE) o Path
Hypothalamus-TSH (ant pituitary)-thyroid-thyroid hormones
PTH vs Calcitonin o PTH increases the blood Ca level and breaks the bone down o Calcitonin decreases blood Ca level by building the bone up
Insulin vs Glucagon o Insulin decreases blood glucose level o Glucagon increases glucose level
Aldosterone o Directly brings in Na and water into the blood in the kidneys o Controlled
Increased K+ level in blood
Decreased blood volume or blood pressure
Acth released by anterior pituitary
Increased blood pressure or volume
Inhibitory o Targets kidney tubules o Antagonized by ANP release by the heart
Stress response o CRH released by hypothalamus (corticotropin releasing hormone) o Causes the adrenal medulla to release catecholamines (epi/norepi) o Catecholamines release ACTH to raise the blood pressure o Catecholamines short term stress response o Mineralo and glucocorticoids=long term stress response
Different behavior? o Due to different receptors
Muscles
Smooth, cardiac, and skeletal
Skeletal is under conscious control
Smooth and cardiac are unconscious
Four functional characteristics of muscle tissue o Contraction o Extension o Elastic o Excitability
Skeletal o Striated o Multinucleated o Cylindrical o ACH binds to it and is always excitatory
Cardiac o Striated o Multibranched o Pacemaker o Cells connected by calated discs
Smooth o No striations o Spindle shaped
o Shortens with calmodulin
Skeletal muscles o Contract small to large o Smaller motor units first
Each bundle separated by perimysium o Bundle=fascicle
Muscle fiber (cell) o Surrounded by the endomysium
Myofibrils o Contains two filaments (myofilaments)
Actin and myosin
Each muscle fiber contains many myofibrils
Motor unit o The motor neuron and all of the muscle fibers it innervates o Vary in size
Myosin and actin o Work together to contract the muscle
T tubules o Allow the AP to go down into cell and release Ca from the sarcoplasmic reticulum
Sarcoplasmic reticulum o Calcium ion storage
Glycosomes o Storage of glycogen for quick energy
Sarcomere o The smallest unit of the muscle o Z disc to z disc o H zone is based on thick filaments only o I bands only thin o A band length of myosin
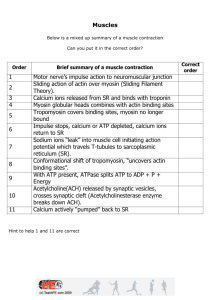
Calcium o The final trigger for the muscle contraction, what is the initial trigger for the muscle cell
Muscle contraction steps o Na enters and AP propagated along the cell and down the t tubule o AP triggers Ca channel in the SR to open o Ca binds to troponin
Changes the shape of tropomyosin and actin active sites are exposed o Contraction
Myosin heads bind to active sites on actin and use energy by ATP to push o Removal of calcium from the cytosol o Tropomyosin blockage restored
Thin filaments
o Actin o Two actin molecules helix shape o Actin associated with troponin and tropomyosin o Troponin binds to Ca ions o Tropomyosin covers active sites
Myosin o Thick filaments o 2 lobed heads
Cross bridge o Myosin head attaches and forms a cross bridge o ATP is released to push the cross bridge
Power stroke o ATP attaches to dislodge crossbridge o The ATP to ADP charges it for its next powerstroke
Sliding filament theory o Myosin pulls actin closer o The H band gets smaller
Rigor mortis o Crossbridge remain engaged after death
High tension o Muscles need ATP to relax
Motor unit recruitment and wave summation o Increasely strong muscle contractions o Motor unit recruitment recruits more motor units o Wave summation work for one motor unit increasing in force (not calling more)
Size principle for motor units o Small-meduim-large
Muscle contaction o Isometric
Same length
No shortening of the sarcomere
Develop tension in the muscle o Isotonic
Shortening
Same tension
Tension is at or above the load so the muscle shortens
Energy o Creatine phosphate
Directly converts ADP to ATP for quick energy o Anaerobic mechanism
Hlycolysis and lactic acid forms
o Aerobic mechanism
Glucose and fatty acids from fat tissue
Provides hours of energy
3 types of fibers o Slow oxidative
Endurance activities
First recruited o Fast oxidative
Sprinting/walking o Fast glycolytic
Short term intense movement
Oxygen debt o Spend more energy than can be provided o Lactic acid build up needs to be corrected
Blood Vessels
Deoxygenated blood comes from a capillary into the right atrium from the vena cava
Pulmonary circuit is lower pressure
Systemic circuit is high pressure
Arterioles go away from the heart
Veins go towards the heart
Pulmonary veins-left atrium-left ventricle-aorta-arterioles-capillary-venules-veins-vena cavaright atrium-right ventricle-pulmonary arteries
Cardiac output o HR X (EDV-ESV) o EDV- amount of blood left in ventricle when the heart is relaxed o ESV- amount of blood left in ventricle during contraction
The highest pressure of anywhere in the circulatory system is in the left ventricle (to get it into the aorta)
Average of 5.25L of blood per minute
Preload o Greater preload leads to a higher stroke volume o Unless they are too high, which decreases stroke volume
Stretches the sarcomere too much
Contractility o The contractile force of the heart o Increased by the amount of Ca ions released
More calcium, more crossbridges
Afterload o The amount left over o Greater left over, need more pressure to push the blood out
Sympathetic nervous system increases the heart rate
Parasymp decreases the heart rate
ADH and aldosterone can affect the volume of the blood
CHF caused by MI, high Bp, etc o Pulmonary CHF
Left side fails first and the blood backs up in the lungs o Peripheral CHF
Right side fails first and the blood pools in extremities
Norepi or epi o Released in adrenal medulla o Activate cAMP mechanisms o Allows more Ca into the cell and cause a stronger contraction
Vessels o Capillaries are responsible for a gas exchange o Types
Fenestrated
Holes in the walls (window)
Intestines
Filtration or absorption is their function
SI is the site of most absorption
Endocrine glands also use fenestrated capillaries
Continuous
No holes/spaces
Lungs-gasses are small enough you just need PM
Specialized continuous capillaries are in the brain
Sinusoidal
Allows cells to go through
WBC’s move around
Arteries o Elastic-conducting o Muscular-distributing o More elastic tissue
Withstand higher pressure o Thicker tunica media
Veins o Valves o Lower pressure
Capillary beds o Perfusion depends on the sphincter of arteriole o Can control which capillary beds are open or closed at a time
Mean arteriole pressure pushes blood through the heart
o Diastolic pressure + 1/3 (pulse pressure (difference between systole and diastole)) o
Pressure through blood vessels is steady-does not vary up and down
How do the veins return blood to the heart o Skeletal muscle contractions o Breathing o Valves in the veins preventing backflow
Contractility is defined by a sarcomere length o At a stable sarcomere length still get increased contraction due to higher calcium levels
Kidney compensation o Multiple ways the kidneys can affect BP o Renin Angiotensin aldosterone system
Angiotensin II causes an increase in BP
Constricts blood vessels by impairing NO synthesis o Increases aldosterone production
Retains Na and water increasing blood volume and blood pressure
Intrinsic mechanisms o Local o Distribute blood flow to individual organs as needed o Metabolic controls and myogenic controls
Extrinsic mechanisms o Global o Nerves and hormones o Control levels all over the body, not just to specific places
Factors determine fluid in and out
o Hydrostatic pressure-force fluid out o Osmotic pressure-water moving in o Net filtration pressure
Respiratory System
4 processes of respiration o Inspiration o Expiration o External respiration o Internal respiration
Continuous capillaries
Breathing o Air passes to alveoli where gas exchange occurs o Inspiration
O
2
into the body o Exhalation
CO2 out
Conducting zone o Filter and warm (nasal cavity) o Moisten the air o Rigid tube with cartilage o Cilia/structures that help filter
Bronchi split until they reach the terminal bronchioles
Alveoli pop up in the respiratory bronchioles
Dividing line is between the terminal bronchioles and respiratory bronchioles
Respiratory zone o Less rigid o Some smooth muscle o Smooth muscle wrapped around the respiratory bronchioles
What controls the dilation of the airway o Smooth muscle controlled by
Gas
Sympathetic
Dilates!!!!!!!!!
α receptors constrict (found in the vessels)
β receptors dilate (found in the lungs)
also found in coronary arteries and skeletal muscle arteries
external respiration membrane o 3 or 4 structures o Alveoli o Continuous capillaries
o 2 types of cells that make up an alveolus
Type 1-shared respiratory membrane
Type 2-surfacant secreting
Detergent that breaks surface tension
Basement membrane (fused) o Immune cells in our lungs
Macrophages constantly hunt for bacteria and pathogens
Macrophage is stuck in alveoli
Negative pressure breathing o Generate a negative pressure to pull air in o Inhalation is active
Contract the muscles o Exhalation is passive
Relax muscles and push air out o Breathing muscles
Diaphragm and intercostal muscles
Lungs automatically want to collapse, chest pushing out
Creates an interplural pressure that is always negative relative to the atmospheric pressure
Visceral pleura lines lungs
Parietal pleura lines the inside of the chest wall
Relative to ATM o Interpulmonary pressure negative on inspiration, zero at break, and positive on expiration
Transpulmonary pressure at 0? o Pneumothorax
P p
=P
T
X C o Partial pressure= total pressure X concentration
Gasses diffuse from high to low o Tissues are in need of oxygen, oxygen diffuses into them
Dead air space o Mixes oxygen o 150 mL o Conducting structures
Dead air space causes expired O2 to be higher than alveolar O2 o The alveolar oxygen is low due to it perfusing into the capillaries
High altitude o Breathing rate increases o More Red Blood cell production
Respiratory groups o Ventral respiratory group
Generate normal breathing
GABA o Dorsal Respiratory Group
Modulates the VRG
Can sense changes in parameters, to then effect o Pontine respiratory center
Can change rate
Respiratory stimulant o CO2 levels drive breathing o CO2 produced from tissues o Decreases the PH of the blood by being converted to carbonic acid which lowers the PH
Hyperventilation o Usually a V/Q match o Ventilation o Perfusion o Need to match
Oxygen carried in the blood by hemoglobin (Hb)
90% of Oxygen attached to Hb o Gives it more solubility o 4 bonds pere Heme
The affinity of hemoglobin for oxygen changes with the extent of oxygen saturation
More oxygen there is, the more affinity there is for O2
High levels of O2 sat o Usually unladed fast to the tissues, and difficult to load to the Hb
Decreased CO2 pressure leads it to be harder to unload
Increased CO2 pressure? Easier to unload
Lower body temperature triggers decreased co2 levels
High metabolic activity leads to increased CO2
CO2 o Typically carried in the blood o Bicarbonate ion o 70% is bicarbonate ion o 20% is dissolved directly in the plasma o 10% bound to Hb
Carbonic anhydrase o Converts CO2 to carbonic acid o In the Red Blood Cell
Cl- comes into the RBC as the HCO3- ion leaves to balance the charges
Haldane effect o Lower O2 levels?
Higher PCO2 o Higher O2 levels?
Lower PCO2
If oxygen is saturated, harder for CO2 to bind to Hb
BPG o Helps push O2 off of the Hb so high levels in systemic capillaries causes O2 unloading
HAPE o High altitude pulmonary edema o Fluid in the lungs o Causes a decrease in alveolar ventilation
Digestive system
Nutrient competition in the gut between good and bad bacteria
Leptin is made by bacteria and signals body to feed
Many organs have dual functions o Liver o Pancreas o Pharynx
Accessory organs o Support the digestive system (not a part of the alimentary canal) o The alimentary canal is the path from the mouth to the anus
The “tube within the tube” o Pancreas o Gallbladder o Liver o Stomach cells
Mechanical digestion o Occurs via the teeth
Chemical digestion o Chemically breaks down food o First is salivary amylase
Breaks down carbohydrates o HCl degrades food in the stomach
Creates chime
Acid also kills many bacteria o SI
Major place of chemical digestion
Proteins, fats, carbs are all degraded and absorbed
Gallbladder o Stores concentrated bile from the liver o Shunts it to the small intestine via the common bile duct (with the pancreas)
Large intestine o Major site of water reabsorption
o Also produces the feces
The goal of digestion is to get the components of food broken down into usable parts
Long reflexes o Go all the way to the CNS and get integrated o Prepare the body to receive food
Short reflexes o Local (enteric) nerve plexus
Reflexes are stimulated by food
Antacids work by blocking H+ ion production and making the stomach acid less acidic o Has the effect of not killing some of the bacteria o Acid is usually 2-3 pH
Stomach digestion o Breaks down food mechanically and chemically
Mechanical is churning
Chemical is acid and peptidases o Gastrin
Stimulates the secretion of HCl and pepsinogen which works to chemically digest proteins (in its active pepsin form) o Pepsinogen
Activated by HCl
Into pepsin
Pepsin then works to break down proteins o Parietal cells
Make the HCl
Secreted by goblet cells o Chief cells
Make the pepsinogen o Enteroendocrine cells
Hormone producing cells
How does the brain control gastric juice production o Brain senses food and secretes additional gastric juice
Reflect of food…saliva o Symp-less o Parasymp-more o Ph based
Low pH-less gastric juice
Vagus nerve of the parasymp NS stimulates the digestive system
Which 3 chemicals are necessary for maximum HCl production? o Gastrin o ACH
From the parasymp (vagus)
o Histamine
Chyme gets sent to the duodenum o The duodenum produces many hormones
Secretin
CCK (Cholecystokinin)
VIP (vasoactive intestinal peptide) o All of these hormones are known under the collective name enterogastrones
SI o Nutrient absorption
Microvilli
Folds (gyri)
Increased surface area o Microvilli contain brush border enzyme
Bring things to the monomer form
Nutrients absorbed go to the liver o Hepatic portal system o Liver creates bile o Bile salts
Emulsifiers
Help break down fats o Lacteals take the fats to the liver
Triglycerides pass into lacteals
Called chylomicrons
Liver o Processes SI blood o Liver stores the glycogen o Detoxifies compounds o Arterioles and venules send blood the same way
Arterioles supply oxygen
Venules supply nutriets
o Kupffer cells
WBC (macrophages) o Liver can regenerate o Bile production
CCK-singals the gallbladder to release
Secretin
Tells the liver to make bile
H+ is neutralized in the SI by bicarbonate ion o Comes from the pancreatic juice
CCK induces the pancreas to produce pancreatic juice
Secretin binds and causes copious release of bicarbonate ions in pancreatic juice
Pancreas hormones (in juice) o Trypsinogen trypsin o Chemotrypsinogen chemotrypsin o Procarboxypeptidase carboxypeptidase o Activated by brush boarder enzymes
Large intestine o Water reabsorption o Some absorption of ions occurs with the water o A lot of bacteria in the LI, some good others bad
Immune System
Adaptive vs innate immune system o Innate
First line of defense
Skin barrier
Mucus membranes
Skin secretions
Doesn’t require previous exposure
Present at birth
Enzymes that can directly kill bacteria
Faster and more immediate
Has internal nonspecific defenses
Phagocytes
Fever
Natural killer cells
Antimicrobial proteins
Inflammation
NK cells recognize antigen (just that it has an antigen) and releases chemicals called granzymes to perforate the membrane
Macrophages
Derived from monocytes
Stem cell is the hemocytoblast
General macrophages eat bacteria
Search for food and engulf them through a process known as phagocytosis
Arrive after neutrophils (part of innate defense)
Phagocytosis
Success rate increased (opsonization)
Antibodies specific to the antigen are produces and coat the bacteria o Neutralization o Agglutination
o Precipitation
Inflammatory response o Neutrophils enter blood from the bone marrow o Margination
They stick to the sides of the blood vessel wall via CAM (cell adhesion molecules) o Diapediesis
Walk to the site o Positive chemotaxis
Call more WBC o Four cardinal signs
Swelling
Edema
Heat
Increased blood flow
Pain
Leaked protein rich fluid
Histamine released
Redness
Increased blood flow
Increased temperature short term helps fight the infection
Long term fever can be dangerous for the organism
Interferons and complement proteins enhance the innate defenses by attacking microbes directly o Interferons are local o Complement proteins are more whole body
Adative immune system o Specific o Made to attack very specific microbes o Vascular o Antibodies o Lymphocytes vs leukeocytes
Lymphocyte is one of three specific types of WBC
Leukeocytes are WBC overall (larger category) o Immunocompetance (need to get educated)
Happens in the T gland for T cells
Bone marrow for B cells
Have not been exposed to antigen? Naïve o APC (antigen presenting cells)
Big 3?
Dendritic cells
B cells
Macrophages o T cells
Recognize our own MHC proteins
If they recognize it? They are killed off to avoid an autoimmune reaction
Surviving cells are self tolerant o Activated immune cells are “selected” and begin to divide o B cells
Plasma B cells-antibody secreted
Memory B cells-stay around for next reaction for less of a lag time o Humoral immunity-antibody mediated (B-cell)
Active-make antibodies
Natural-antibodies/reaction
Artificial-vaccine
Passive-pass antibodies
Natural-passed from mom
Artificial-serum (antibodies) o Cell mediated immunity
T cell response
Helper T cells recognize and help mount an attack o CD4 o Respond to class II MHC’s via the APC’s
Cytotoxic T cells kill directly o Induce apoptosis with granzymes and perforin o CD8 o Respond directly to class I MHC proteins
MHCII
Only present in APC
Taken in by APC cells (endocytosed) and combined with a MHCII receptor
Only an antigen fragment is displayed (antigenic determinant)
MHCI
All cells carry it
Display any antigens that invade the cell
Urinary System
Kidney is at the center of the urinary system o Major functions
Filter blood
Excrete urine
pH balance is important
o blood comes from the aorta and feeds the kidneys o pair of ureters collects the urine
nephrons-functional unit of the kidney o also the urine forming units
Proximal convoluted tubule (PCT) o Cells have lots of mitochondria and microvilli
Absorption function
Kidneys modulate the systemic BP o Catcholamines o Angiotensin o Renin o ADH
Glomerulus is where renin is released o Can sense the BP o Renin raises the BP (vasoconstrict)
Proteins cannot pass throught he glomerular filtration membrane because it is too selective
three forces determine the filtrate formation o glomerular hydrostatic pressure
out o osmotic pressure
in o capsular hydrostatic pressure
in o net outward pressure is 10mm hg
three mechanisms help maintain glomerular filtration rate when systemic bp is altered o myogenic o tubuloglomerular o hormonal
afferent arterioles enter the glomerular capsul
efferent arterioles leave
the macula densa cells in the ascending loop of henle sense alteration of the filtrate flow and the NaCl concentration
The water in kidneys follows solutes out passively
Proximal Convoluted Tubule o Contains the Na/K pump that establishes the gradient to maintain ion balance
Primary and secondary active transport for absorption
Transport maximum exists for everything but Na ion o Maximum number of carriers are operating
DCT o Primary control of tubular secretion/reabsorption
Sends things back IN to the Tube if there is too much in the blood
o Aldosterone-sends Na in o Parathyroid hormone (PTH)-sends Ca in
Loop of henle o Descending limb-water reabsorption passive o Ascending limb-solute reabsorption (mostly active)
Collecting duct o Water reuptake
Concentrates the urine o ADH affects it
Higher levels, more aquaporins, more water reabsorption o Water is reabsorbed into the vasa recta as to not affect the ion concentrations
Reproduction
Meiosis evolved o Mechanism to correct for error without cell division o Ploidy cycle-sometimes benefit from being haploid
Genes required for mitosis were repurposed for meiosis
Sex started-evolution occurred rapidly
Meiosis o Two stages
Meiosis I-hapliod but still replicated
Meiosis II-haploid and only one copy o Genetic variability
Random assortment in metaphase I
Crossing over in prophase I
Random fertilization o 4 gametes out of the male process o 1 viable gamete for females (3 polar bodies)
Male gametes made in the seminiferous tubules o Edge cells move towards the lumen and become sperm
Spermatogonia o The male stem cells o Type A and B daughter cells
Sustentacular cells (sertoli cells) o Surround and protect the spermatogonia o Keep the immune system out
Tight junctions o Produce ABP (andreogen binding proteins)
Respond to FSH and LH o APB and testosterone combine to form the complex needed to form mature sperm
FSH and LH
o Stimulated by GnRH
Females o Meiosis produces polar bodies
These polar bodies are not viable gametes
Nonfunctional o 1 function oocyte is produced o a woman has 2 million primary oocytes present at birth o only 10% make it to primary follicle stage o Always more than one oocyte going through stages
Only one responds best to the hormones o Follicular phase and luteal phase
Follicular phase
Initial follicle to the thick follicle
Primary to secondary oocyte
14 days average
Lueteal phase
Almost always 14 days
Antrum, secondary oocyte, and its release o Thecal cells
Release male hormones (androgens) o Granulosa cells
Convert androgens to estrogens o Sometimes more than one oocyte is released
Fertilized by 2 different sperm?
Fraternal twins o Fertilized
Once it is fertilized, the blastocyst is implanted into the uterine wall to allow it to grow o Sperm cell is only good for 1-2 days because the mitochondria die out and use up all the energy o 3-4 days for an oocyte
Has all of the cytoplasm and organelles needed to survive o Increasing LH/FSH surge
Induces the follicle growth o LH
Receptors on the thecal cells create androgens o FSH
Receptors on the follicle cells o Estrogen release in the blood causes a burst of FSH/LH release (not production)
Positive feedback mechanism o Follicle gets larger, produces more estrogen, this triggers a shut off
o FSH and LH surge occurs around 14 days
Estrogen dependent o Surge causes ovulation o After ovulation, the follicle ruptures and this leads to declining estrogen levels in the blood o Estrogen levels decrease, progesterone increases o Follicular cells become the corpus luteum
Under control of LH
Degraded if no fertilization o Estrogen and progesterone
Estrogen=ovulation
Also allows sperm into the uterus by making the mucus slimy
Progesterone=changing in the uterus to prepare for ovulation
Blocks the uterus again o No fertilization?
The uterine lining is shed o Regular bleeding and shedding (monthly)
The purpose is to make sure the uterine wall is responding to the hormones
Also helps disinfect the uterus o Uterine cycle
Menstrual phase (shed lining)
Proliferative phase (builds up)
Secretory phase (postovulatory)
The endometrium prepares for the implantation of the embryo o Implantation occurs
Now the uterus needs to keep the nutrients up o Inner cell mass develops into the blastocyte o The lungs of the baby develop last o Human chorionic gonadotropic (HCG)
Spike helps initially develop the placenta
Develops the corpus luteum
That secretes estrogen and progesterone o Hormones from the corpus luteum maintain the uterus structure o The HCG comes from the oocyte itself if fertilized o HCG drops off?
This leads to estrogen and progesterone getting released from the placenta
This occurs after the embryo is implanted o Fetus is not rejected by the mother because the mother recognizes it