1/1231 - Lectur'ED beta
advertisement

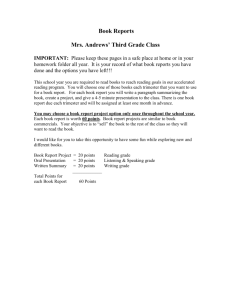
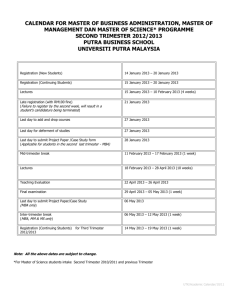
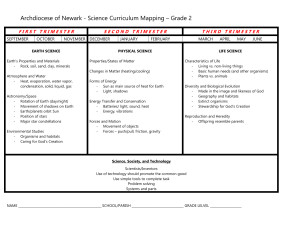
Prenatal Testing And Screening Lecture Outline 1. Definitions 2. Age related risks 3. Etiology and phenotype of chromosome anomalies 4. Risks, phenotype and testing options of ONTD 5. 1st and 2nd Trimester Prenatal Testing Options 6. 1st and 2nd Trimester MS Screening Options 7. New approaches to combining these tools 8. Ultrasound as a screening tool Testing Defined A procedure that (in most cases) provides a definitive answer to the question that is being asked. Tests that have low false positives and negatives are considered diagnostic. In the case of prenatal testing there is a risk of miscarriage associated with all the currently available diagnostic invasive tests. Screening Defined • Identify those at increased risk who are not be perceived to be at risk • Does not dx definitively • Follow-up options available for definitive information • Sensitivity=True positives/all affected • Specificity=True negatives/all unaffected Baseline Risk for Having a Child With a Serious Birth Defect 3-5% WE DON’T GET BETTER WITH AGE Maternal Age 20 30 33 34 35 36 37 38 39 40 41 DS Risk Birth All Chrom Abn Birth DS risk Mid trimester 1/185 1/592 1/465 1/384 1/285 1/243 1/385 1/287 1/225 1/177 1/178 1/149 1/123 1/105 1/139 1/109 1/80 1/63 1/1231 1/685 1/452 1/352 1/274 1/213 1/166 1/129 1/100 1/80 1/85 1/48 1/61 NORMAL MALE KARYOTYPE 46,XY NORMAL FEMALE KARYOTYPE 46, XX WHEN MEIOSIS FAILS Nondisjunction Normal Sex cell production Sex Cells Sex Cells Monosomy T21 Tid Bits • ~70% T21 due to an error in maternal meiosis I • ~ 20% maternal meiosis II • ~ 5% occur during spermatogenesis (meiosis II) • 5% of trisomic 21 error in mitosis – no advanced maternal age and there is no preference for which chromosome 21 is duplicated in the mitotic error • most common chromosomal abnormalities in liveborn children ~1/700 Phenotype • Moderate mental retardation • Characteristic facies – – – – upslanting palpebral fissures epicanthic folds, midface hypoplasia, macroglossia • Congenital malformations – heart (30-40%), atrioventricular canal – gastrointestinal tract, such as duodenal stenosis or atresia, imperforate anus, and Hirschsprung disease – Leukemia (both ALL and AML) 10-20x – acute megakaryocytic leukemia occurs 200 to 400 times more frequently in the Down syndrome – 90% have significant hearing loss, usually of the conductive type Trisomy 18, Edward syndrome 1/8000 Facial Central Nervous System Trisomy 18 •microcephaly with prominent occiput •narrow bifrontal diameter •short palpabral fissures •low-set malformed ears •cleft lip +/- palate •narrow palatal arch •micrognathia Skeletal •neck •webbed •chest •short sternum •widely spaced nipples •hips: •small pelvis, congenital dislocation of the hips, limited hip abduction •extremities: •phocomelia •rockerbottom feet or equinovarus short dorsiflexed big toes fixed flexion deformity of the fingers (overlapping of the 2nd and 5th fingers over the 3rd and 4th fingers) simple arch pattern of the fingers and toes hypoplasia of fingernails single crease of 5th finger or all fingers severe mental retardation hypotonia -> hypertonia neural tube defects poor suck and weak cry failure to thrive ocular anomalies Respiratory •apnea Cardiovascular( >95%) •major: VSD, ASD, PDA •minor: transposition, ToF, coarctation, anomal coronary artery, dextrocardia, •aberrant subclavian artery, arteriosclerosis, P bicuspid aortic and/or pulmonic valves Gastrointestinal •inguinal, umbilical, and/or diaphragmatic hernia •congenital defects: •diastasis recti, heterotopic pancreas, malrota Meckel's, tracheoesophageal fistula Genitourinary •cryptorchidism •congenital defects: double ureter, ectopic kidney, horseshoe kidney, hydronephrosis, polycystic kidney 47,XXY •severe mental retardation •coloboma, •(a cleft palate) and/or a cleft lip •hypotonia •skeletal abnormalities (polydactyly) •Renal • T13 Patau syndrome heart defects • 1/5,000 •holoprocencephaly 1/1000 Kleinfelter syndrome 45, X 45, X Miscarriage Turner syndrome 1/3000 liveborns Neural Tube Defects • Second most common major congenital defect (1-2/1000) • Not a chromosome anomaly • Routinely tested and screened for in pregnancy • Failure neural tube to close at 28 days gestation • 20% are closed lesions and difficult to detect prenatally Open Neural Tube Defects Open lesions Closed lesions In 1976 the American College of Obstetrics and Gynecology recommended prenatal diagnosis be offered to all women 35 years of age and older at delivery. INDICATIONS FOR PRENATAL DIAGNOSIS Maternal age > 35 years at EDC Abnormal maternal serum screening for: DS cut off > 1/270 Increased risk Trisomy 18 or 13 Smith-Lemli-Opitz syndrome ONTD Previous child with chromosomal abnormality or diagnosable genetic disorder Balanced translocation carrier Ultrasound anomaly (soft sign vs frank anomaly) PRENATAL DIAGNOSTIC PROCEDURES AMNIOCENTESIS CHORIONIC VILLUS SAMPLING PERCUTANEOUS UMBILICAL CORD SAMPLING AMNIOCENTESIS PERFORMED ROUTINELY 16-20 WEEKS ULTRASOUND GUIDED AMNIOCENTESIS Amniocentesis Testing • Chromosome analysis • AF-AFP levels • Acetylcholinesterase ONTD • Risk of miscarriage associated with procedure 1/100-1/400 Advantages • • • • Highly reliable results 99+% Familiar Long standing reputation NTD detection Disadvantages • Late in gestation – Decision making – Privacy – Mom feels movement • Fear of needles • Needle invades the sac Fetus: 12 weeks gestation Chorionic Villus Sampling Performed >10 wks-13 weeks Transcervical Chromosome analysis Risk 1/100-1/200 Transabdominal • trophoblastic shell cells • Syncitiotrophoblasts – poly-proliferate tissue type=directs • cytotrophoblasts • Mesodermal core=tissue culture • frorm finger-like extensions Disadvantages • Placental mosaicism 1% of CVS is confirmed in the fetus ~ 10-40% • Second trimester amniocentesis mosaicism ~ 0.1-0.3% & confirmed in a fetus up to 70% of the time. • ?LRD risk prior to 70 days gestation (10 weeks) • Higher loss rate • Less access to procedure • Higher chance of insufficient sample • Early test=risk of sampling a fetus potentially destined to miscarry • No ONTD testing • More risk of vaginal bleeding • Speculum Benefits (1) Earlier in gestation (2) rapidly growing cell cultures practically free of maternal cell contamination (3) an efficient direct method to obtain high quality metaphases from the of the syncitiotrophoblasts tissue which the fetal karyotype is defined within a few hours of chorionic villi sampling (specialty cyto techinque) (4) is suitable for a rapid, direct diagnosis of the related metabolic diseases. (5) placental mosaicism (trisomic rescue in fetus) can increase the risks of genetic abnormalities such as uniparental disomy G. Simoni1, Human Genetics 1983 Fetal Blood Sampling “PUBS” Percutaneous Umbilical Cord Sampling (PUBS) or Cordocentesis • ~2% risk of loss • Technically difficult prior to 20 weeks • Blood disorders such as hemophilia and anemia – Useful for detection of Rh isoimmunization of the fetus (blood cell count and oxygen level)→erythroblastosis fetalis (HDN) • Chromosomal abnormalities Fetal karyotype in 48 hours • Infections such as toxoplasmosis and rubella. • The procedure is also used to perform blood transfusions to the fetus and to administer medication directly into the fetal blood supply. Reproductive Decision Making RISK Fetal Aneuploidy Procedure Related RISK TO TEST OR NOT TO TEST I want to know The benefits outweigh the risks Options are desirable Because my doctor says so….. Not sure I want to know Risks are a big worry Options stink Because my doctor says so…. So what to do what to do………….. SECOND TRIMESTER MATERNAL ANALYTES FOR ANEUPLOID SCREENING FETAL Alpha-fetoprotein- AFP Estriol- uE3 PLACENTAL Estriol- uE3 Human chorionic gonadotrophin- hCG Inhibin-A nd 2 Trimester MSS Overview Used for detection of: 1. 2. 3. 4. ONTD Down syndrome trisomy 18 Smith-Lemli-Opitz syndrome Second trimester MSS ONTD Serum Marker AFP DS X MoM 0.7 HCG uE3 Inhibin-A 2.1* T18 SLO 0.65 0.36 0.21* 0.7 2.1 0.4* Smith Lemli Opitz Syndrome • Defect enzyme in the conversion of 7-dehydrocholesterol to cholesterol. • Affects 1 in 20,000 to 40,000 births • Autosomal Recessive • Mental Retardation • Slow growth • Heart defects • Facial cleft • Screen positive women have uE3 < 0.4 MoM • ~2% baby affected • Testing AF for 7-8- dehydrocholesterol (7/8-DHC) levels Other…….. Turner Serum Marker AFP HCG uE3 Inhibin-A T13 Triploidy Pregnancy complications uE3 lower than 0.1 MoM • Increase risk for x-linked ichthyosis ONTD screening • Abnormal Screen MS-AFP > 2.5 MoM • Elevated MSAFP recommendations: – Ultrasound – 90% r/o spinal lesions 100% r/o anencephaly – VWD reduced with normal scan – If MSAFP >4.0 MoM and NL U/S offer invasive testing Detection Rates MSAFP • Anencephaly • Spina Bifida 100% 85-90% • VWD – Omphalocele 70% – Gastroschisis 90% Add Ultrasound 100% 90% 95% 95% 2nd Screening for DS Trimester 1/270 Cut-off DR% FPR% • Age 20 5 • Age AFP 30 5 • Age AFP + HCG (Double) • Age AFP+uE3+HCG (Triple) • Age AFP+uE3+HCG+Inhibin-A (Quad) 55 5 61 7 75 5 The detection rate for Down syndrome using the second trimester triple screen is: 50% for women <35 y/o 88% for women >35 y/o and ~60% for all women Quad ~75% First Trimester Integrated Screening For Trisomies =FIRST •Entire analysis performed 11-13 6/7 weeks gestation •MS free Beta hCG and PAPP-A (pregnancy associated plasma protein) -obtained bw 9-13 weeks •Nuchal measurement 11-13 6/7 •Maternal age •Detection Rates: ~80% Down syndrome ~90% trisomy 18 1/270 1/100 Nuchal Translucency (NT) • Gestation 11 to 13 6/7 wks •Mid-sagittal view • Fetus away from amnion • Enlarge head & upper thorax • Widest part of NT First Trimester Screening DS T18 • Free beta HCG • PAPP-A • NT >3.0 mm Down syndrome DR ~1:270 Cut-off FPR MA + NT1 10% DR 71% MA + Biochemistry3 67% MA + NT + Biochemistry2 >80% 5% 1. Schuchter et al. Prenatal Diagnosis 22: 211, 2002 2. Wapner et al. NEJM 349: 1405, 2003 3. Spencer et al UOG 1999 Nasal bone Recommendations 1st Trimester Nuchal >3.5 • CVS • Targeted ultrasound evaluation 18-20 • Echocardiogram • Residual 5-6% risk neonate may have a yet undefined genetic syndrome… Fetal Nasal Bone • 65% DS have absent nasal bone • General population 1% – African Americans 8%-10% • Secondary screen • Difficult to obtain • Higher false positive in 1st Integrated Screening Timeline weeks 10-14 DR: 94-96% FPR: 5% 16-19 18-20 PAPP-A and Nuchal + Quad Screen = Results Screen Positive 1/270 DS 1/100 T18 2.5> ONTD US Amnio Nothing Screen Negative Decision Making 20+ wks Advantages • Increases detection rate • Decreases false positive rate (fewer tests and fewer procedure related losses) Disadvantages • Long wait time for result • Unable to utilize CVS and early detection • Late GA by the time amnio results final Contingent First Trimester Screening High risk Offer CVS Low Risk Intermediate Triple Screening Integration Low Risk Stop High risk US and Amnio Advantages • Increase detection rate 90% • Decrease FPR 2% • Reduce the number of amnios performed in low risk pregnancies Disadvantages •New (limited data) •Hard to determine uptake •Offered at few institutions RISK OF ANEUPLOIDY BASED ON GA AND ANOMALY 3D Ultrasound Fetal Face 24 weeks Gestation Fetal MRI FETOSCOPY Umbilical cord Amnion (stuck twin) QUESTIONS ??