Stroke Prevention in AF
advertisement

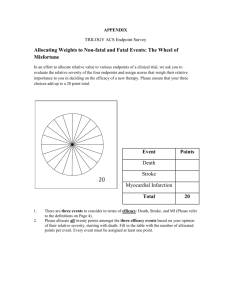
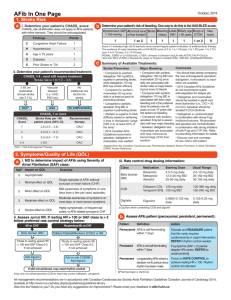
Primary Care Education Progam Steering Committee FAMILY PRACTITIONERS: Dr. Carl Fournier, Montreal, QC Dr. Peter Lin, Toronto, ON Dr. Vinod Patel, St. John’s, NFLD Dr. Kevin Saunders, Winnipeg, MB Dr. Richard Ward, Calgary, AB SPECIALISTS: Dr. Paul Dorian, Toronto, ON Dr. Victor Huckell, Vancouver, BC Dr. Mukul Sharma, Ottawa, ON Dr. Jeffrey Weitz, Hamilton, ON Incidence of AF: Expected to Increase as Population Ages Projected Number of Persons With AF in the US: 2000- 2050 Millions Age- and Sex-Adjusted Incidence of AF in 1995-2000 Year Circulation 2006;114:119 Perspectives on Stroke • About 80% of all strokes are ischemic1 • Effect of first ischemic stroke in patients with AF: 60% are disabling, 20% are fatal2 • ICH has a 30-day mortality rate of 35% to 52%3 • Severe strokes are viewed by many patients as equal to or worse than death4,5 1Heart and Stroke Foundation; 2 Gladstone Stroke 2009;40:235; 3AHA Stroke 1999;30:905-15; 4Gage Arch Intern Med 1996;156:1829; 5Solomon Stroke 1994;25:1721 Embolic Stroke • Noncontrast CT brain scan showing two discrete areas of infarction (arrows) within the right middle cerebral artery Kelley RE & Minagar A. Southern Medical Journal 2003;96(4):343-349 Stroke Severity in Patients with AF Effect of first ischemic stroke in patients with AF (n=597) 60% % of patients 50% 40% 30% 20% 10% 0% AF=atrial fibrillation Disabling Fatal Gladstone DJ et al. Stroke 2009; 40:235-240 Warfarin in Atrial Fibrillation: • Warfarin reduces stroke in non-valvular AF by 64% - Significant increase in intracranial and other hemorrhage • Registries show 50-60% of eligible patients receive warfarin • In clinical trials, time in therapeutic range (TTR) is 60-68% • In general practice, TTR is typically <50% 1Hart Ann Int Med 2007;146:857; 2Hylek Stroke 2006;37:1075; 3Singer Chest 2008;13;3:546S 4Gladstone Stroke 2009;40:235; 5Matchar Am J Med 2002;113:42; 6Bungard Pharmacotherapy 2000;20:1060 CCS 2012 Update to AF Guidelines Assess Thromboembolic Risk (CHADS2) CHADS2 = 0 CHADS2 = 1 CHADS2 ≥ 2 Increasing stroke risk No antithrombotic No additional risk factors for stroke ASA Either female sex or vascular disease OAC* Age ≥ 65 yrs or combination of female sex and vascular disease OAC = Oral anticoagulant ASA = Aspirin 1. Skanes AC, et al. Can J Cardiol 2012;28:125-136. OAC* *Aspirin is a reasonable alternative in some as indicated by risk/benefit OAC Consider stroke risk vs. bleeding risk Only when the stroke risk is low and bleeding risk is high does the risk/benefit ratio favour no antithrombotic therapy CCS 2012 Update to AF Guidelines When oral anticoagulant therapy is indicated, most patients should receive dabigatran, rivaroxaban, or apixaban*, in preference to warfarin • Dabigatran and apixaban have greater efficacy and rivaroxaban has similar efficacy for stroke prevention • Dabigatran and rivaroxaban have no more major bleeding and apixaban has less • All three new oral anticoagulants have less intracranial hemorrhage and are much simpler to use *Not yet approved in Canada 1. Skanes AC, et al. Can J Cardiol 2012;28:125-136. Prevention of Stroke Cross-trial comparisons must be interpreted with caution due to differing methodologies and patient populations. Superiority p-value Stroke or Systemic Embolism Dabigatran 110 mg BID Dabigatran 150 mg BID 0.90 0.29 0.65 Rivaroxaban 20 mg QD Apixaban 5 mg BID 0.88 Dabigatran 150 mg BID 0.01 1.11 0.35 0.76 0.03 0.94 Rivaroxaban 20 mg QD 0.59 0.92 Apixaban 5 mg BID 0.50 0.12 0.79 Ischemic Stroke Dabigatran 110 mg BID <0.001 0.75 1.00 0.42 1.25 HR (95% CI) Comparator better 1.50 Warfarin better Connolly N Engl J Med 2010;363:1876; Patel N Engl J Med 2011;365:883; Granger N Engl J Med 2011;365:981 Boehringer Ingelheim (Canada) Ltd. cannot recommend the use of products outside the Canadian approved Product Monograph. Reducing the Bleeding Risk Cross-trial comparisons must be interpreted with caution due to differing methodologies and patient populations. Intracranial Hemorrhage Dabigatran 110 mg BID Dabigatran 150 mg BID Rivaroxaban 20 mg QD Apixaban 5 mg BID Superiority p-value 0.30 <0.001 0.41 <0.001 0.67 0.02 0.42 ISTH Major Bleeding Dabigatran 110 mg BID <0.001 0.80 0.003 0.93 Dabigatran 150 mg BID 0.31 1.04 Rivaroxaban 20 mg QD 0.58 0.69 Apixaban 5 mg BID 0.25 0.50 <0.001 0.75 1.00 1.25 HR (95% CI) Comparator better Warfarin better Boehringer Ingelheim (Canada) Ltd. cannot recommend the use of products outside the Canadian approved Product Monograph. Connolly N Engl J Med 2010;363:1876; Patel N Engl J Med 2011;365:883; Granger N Engl J Med 2011;365:981 New OAC vs. warfarin in moderate CKD (eGFR <50 ml/min) Stroke or Systemic Embolism RR (95% CI) Dabigatran 110 mg BID 0.77 (0.51-1.18) Dabigatran 150 mg BID 0.55 (0.40-0.81) Rivaroxaban 15 mg QD 0.86 (0.63-1.17) Apixaban 2.5/5 mg BID 0.79 (0.57-1.20) 0.50 0.75 1.00 1.25 1.50 HR (95% CI) New Agent Better Warfarin Better Hart RG, et al. Nat Rev Nephrol 2012 (on line) Connolly SJ, et al. N Engl J Med. 2009; 361:1139 Fox KAA et al. Euro Heart J 2011; 32: 2387 Granger C, et al. N Engl J Med. 2011; 365: 981 New OAC vs. warfarin in moderate CKD (eGFR <50 ml/min) Major bleeding RR (95% CI) Dabigatran 110 mg BID 0.99 (0.76-1.28) Dabigatran 150 mg BID 1.03 (0.80-1.34) Rivaroxaban 15 mg QD 0.95 (0.72-1.26) Apixaban 2.5/5 mg BID 0.50 (0.38-0.66) 0.50 0.75 1.00 1.25 1.50 HR (95% CI) New Agent Better Warfarin Better Hart RG, et al. Nat Rev Nephrol 2012 (on line) Connolly SJ, et al. N Engl J Med. 2009; 361:1139 Fox KAA et al. Euro Heart J 2011; 32: 2387 Granger C, et al. N Engl J Med. 2011; 365: 981 Safety Outcomes: RELY D 110 mg vs. W RR 95% CI P D 150 mg vs. W RR 95% CI P D 110mg Annual rate D 150mg Annual rate W Annual rate Major or Minor Bleeding 14.62% 16.42% 18.15% 0.78 0.73-0.83 <0.001 0.91 0.85-0.96 0.002 Intracranial Bleeding 0.23 % 0.32 % 0.76 % 0.30 0.19-0.45 <0.001 0.41 0.28-0.60 <0.001 Major Bleeding 2.87 % 3.32 % 3.57% 0.80 0.70-0.93 0.003 0.93 0.81-1.07 0.32 Life-Threatening Major Bleed 1.24 % 1.49 % 1.85 % 0.67 0.54-0.82 <0.001 0.80 0.66-0.98 0.03 Fatal Bleed* 0.19 % 0.23 % 0.33 % 0.58 0.35-0.97 0.039 0.70 0.43-1.14 0.15 GI Major Bleed 1.15 % 1.56 % 1.07 % 1.08 0.85-1.38 0.52 1.48 1.18-1.85 0.001 Connolly NEJM 2010;363:1876; *Eikelboom Circulation 2011;123:2363 Safety Outcomes*: ROCKET AF Rivaroxaban Warfarin Event Rate (per 100 patient/years) Event Rate (per 100 patient/years) HR (95% CI) P-value Primary: Major and Non-Major Clinically Relevant Bleeding 14.9 14.5 1.03 (0.96, 1.11) 0.44 Major: 3.6 3.4 1.04 (0.90, 1.20) 0.58 >2 g/dL Hgb drop 2.8 2.3 1.22 (1.03, 1.44) 0.02 Transfusion (> 2 units) 1.6 1.3 1.25 (1.01, 1.55) 0.04 Critical Bleeding 0.8 1.2 0.69 (0.53, 0.91) 0.007 Fatal Bleeding 0.2 0.5 0.50 (0.31, 0.79) 0.003 0.5 0.7 0.67 (0.47, 0.93) 0.02 3.2 % of pts 2.2% of pts Not reported <0.001 11.8 11.4 1.04 (0.96, 1.13) 0.35 10.1% of pts 8.6 % of pts Not reported <0.05 Intracranial Hemorrhage Major GI Bleeding Non-Major Clinically Relevant Bleeding Epistaxis *Based on Safety On-Treatment Population Patel N Engl J Med 2011;365:883 Bleeding and Net Clinical Outcomes: ARISTOTLE Apixaban Warfarin Event Rate (per Event Rate 100 patient/years) (per 100 patient/years) Primary: Major Bleeding 2.13 Intracranial Hemorrhage HR (95% CI) Pvalue 3.09 0.69 (0.60, 0.80) <0.001 0.33 0.80 0.42 (0.30, 0.58) <0.001 Other Location 1.79 2.27 0.79 (0.68, 0.93) 0.004 Major GI Bleeding 0.76 0.86 0.89 (0.70, 1.15) 0.37 Major or Clinically Relevant Non-Major 4.07 6.01 0.68 (0.61, 0.75) <0.001 Net Clinical Outcome* 6.13 7.20 0.85 (0.78, 0.92) <0.001 *Net Clinical Outcome: Stroke, systemic embolism, death, or major hemorrhage Boehringer Ingelheim (Canada) Ltd. cannot recommend the use of products outside the Canadian approved Product Monograph. Similarities Across the 3 Novel Oral Anticoagulants: Comparing Dabigatran 150 mg, Rivaroxaban, and Apixaban Vs. Warfarin • All 3 agents were non-inferior to warfarin in reducing the risk of stroke / systemic embolism • All 3 agents reduced ICH • The 3 agents seem to demonstrate a consistent trend towards mortality reduction Cross-trial comparisons must be interpreted with caution due to differing methodologies and patient populations. Connolly N Engl J Med 2010;363:1876; Patel N Engl J Med 2011;365:883; Granger N Engl J Med 2011;365:981 Boehringer Ingelheim (Canada) Ltd. cannot recommend the use of products outside the Canadian approved Product Monograph. Differences: Comparing Dabigatran 150 mg, Rivaroxaban, and Apixaban Vs. Warfarin • Dabigatran and apixaban demonstrated superiority over warfarin in reducing stroke/systemic embolism • Dabigatran reduced ischemic stroke • Apixaban reduced major bleeding • Rivaroxaban is dosed once daily Cross-trial comparisons must be interpreted with caution due to differing methodologies and patient populations. Connolly N Engl J Med 2010;363:1876; Patel N Engl J Med 2011;365:883; Granger N Engl J Med 2011;365:981 Boehringer Ingelheim (Canada) Ltd. cannot recommend the use of products outside the Canadian approved Product Monograph. Patients unsuitable for new anticoagulants AF patients not recommended for therapy with new anticoagulant agents approved for stroke prevention include: • Patients with valvular heart disease • Patients with mechanical valves • Patients with advanced renal impairment (CrCl<30 mL/min) • Patients with active bleeding 1. Pradax™ (Dabigatran Etexilate Capsules) Product Monograph, 2012, Boehringer Ingelheim Canada Ltd. 2. Xarelto™ (Rivaroxaban tablet) Product Monograph, February 2012, Bayer Inc. Case: Patient with hypertension, diabetes, prior TIA Patient Profile: Jack Jack • Jack is a 64-year old Caucasian man • Married, lives with wife • Works from home but frequently travels to the US for work • Goes to the gym twice/week • He is 5’ 11” tall (180 cm) • Weighs 187 lb (85 kg), • BMI is 26.1 • “I’m here only because of my wife … she thinks I had a stroke” Medical History • Jack’s medical conditions are as follows: - Diagnosed with atrial fibrillation 3 years ago - on warfarin - His INR has been stable although he admits this is difficult because of his lifestyle and work-related activities - Hypertension – on ramipril and thiazide - Diabetes – on metformin • Jack smokes 5-6 cigarettes/day, especially when he is travelling • Jack also drinks 1-2 glasses of wine or beer/day - This increases to 2-3 glasses of wine or beer/day when he is travelling (about once/month) Medical History • About 3 weeks ago Jack had a “spell” - While eating dinner he suddenly stopped speaking The right side of his mouth drooped The fork fell from his hand It lasted 20 min • Jack did not go the emergency department - “I felt fine and was about to go on a trip” • His INR one week ago was 1.5 Discussion Questions 1. What was the “spell”? - Do you need any other clinical information or investigations? 2. What are the options for management? Important Points • The episode was focal, abrupt in onset and brief - It meets the clinical diagnosis of TIA - New criteria require the exclusion of tissue damage with brain imaging • The physical examination is directed toward excluding a deficit which would suggest stroke - Speech, motor function, facial strength, visual fields - BP ( correlates with risk of hemorrhage) • Investigations are directed toward exclusion of other causes of TIA and excluding rare mimics - CT head, carotid Doppler or CTA/MRA 1. Lindsay MP et al. Canadian Best Practice Recommendations for Stroke Care (Update 2010) Canadian Stroke Network. www.hsf.sk.ca/siss/documents/2010 What-if Scenarios • Jack wants to know when he can travel - “They really need me in Peoria next week” • What if his Doppler shows: - < 50% carotid artery stenosis? - 50-69% carotid artery stenosis? • What if Jack’s CT report reads: - Small area of hypodensity in the right centrum semiovale consistent with infarction Key Evidence Most recent guidelines for stroke prevention in patients with AF (CCS, 2012) TIA / minor disabling ischemic stroke is associated with a high early risk of recurrent stroke. TIA is defined as a transient episode of neurologic dysfunction caused by focal brain, spinal or retinal ischemia without infarction while ischemic stroke is defined as an infarction [tissue injury] of central nervous system tissue. 1. Skanes AC, et al. Can J Cardiol 2012;28:125-136. 2. Lindsay MP et al. Canadian Best Practice Recommendations for Stroke Care (Update 2010) Canadian Stroke Network. www.hsf.sk.ca/siss/documents/2010 The Definition of Stroke/TIA A clinical syndrome characterized by the sudden onset of a focal neurological deficit presumed to be on a vascular basis 1. Lindsay MP et al. Canadian Best Practice Recommendations for Stroke Care (Update 2010) Canadian Stroke Network. www.hsf.sk.ca/siss/documents/2010 2. Johnston et al. Ann Neurol 2006; 60: 301–313. Tissue Based TIA Definition • Brief episode (typically <1h) caused by focal brain or retinal ischemia without evidence of infarction • Indicates risk • Encourages neurodiagnostic tests • Facilitates rapid intervention Albers GW et al. N Engl J Med 2002;347:1713-1716. Early risk of stroke after discharge from the emergency department among patients with a first-ever TIA 1. Gladstone D et al. CMAJ. 2004 Mar 30;170(7):1099-104. Key Evidence CHA2DS2- Vasc performed better when patients were categorized as low [score = 0] moderate [score=1] or high [score = >2] risk principally because of more precise estimates of thromboembolic risk in patients with CHADS2 score of 0 or 1. 2 points for age >75 yrs and 1 point for age 65-74 yrs. 1 point each for vascular disease [prior MI, peripheral arterial disease or aortic plaque] or female sex 1. Lip GY et al. Chest 2010;137:263-272. 2. Skanes AC, et al. Can J Cardiol 2012;28:125-136. CHADS2 Score (Simple prediction tool for assessing stroke risk) • 1 point for Congestive Heart Failure • 1 point for Hypertension • 1 point for Age ≥ 75 years • 1 point for Diabetes Mellitus • 2 points for Prior Stroke or TIA CHADS2 Score* Stroke Rate, %/yr (95 %CI) 0 1.9 (1.2 – 3.0) 1 2.8 (2.0 – 3.8) 2 4.0 (3.1 – 5.1) 3 5.9 (4.6 – 7.3) 4 8.5 (6.3 – 11.1) 5 12.5 (8.2 – 17.5) 6 18.2 (10.5 – 27.4) *Score 0: Patients can be administered aspirin *Score 1: Patients can be administered aspirin or anticoagulant therapy *Score ≥2: Patients should be administered anticoagulant therapy 1. Gage BF, et al. JAMA. 2001;285:2864-2870. CHA2DS2-VASc Score • 1 point for Congestive Heart Failure/ LV Dysfunction • 1 point for Hypertension CHA2DS2-VASc Score* One year event rate (95% CI) of hospital admission and death due to thromboembolism† per 100 person year 0 0.78 (0.78 – 1.04) 1 2.01 (1.70 – 2.36) 2 3.71 (3.36 – 4.09) • 2 points for Prior Stroke or TIA1 or TE2 3 5.92 (5.53 – 6.34) • 1 point for Vascular Disease3 4 9.27 (8.71 – 9.86) 5 15.26 (14.35 – 16.24) • 1 point for Age 65-74 years 6 19.74 (18.21 – 21.41) • 1 point for Sex category (female gender) 7 21.5 (18.75 – 24.64) 8 22.38 (16.29 – 30.76) 9 23.64 (10.62 – 52.61) • 2 points for Age ≥ 75 years • 1 point for Diabetes Mellitus *Score 0: Patients can be administered aspirin *Score 1: Patients can be administered aspirin or anticoagulant therapy *Score ≥2: Patients should be administered anticoagulant therapy †Includes peripheral artery embolism, ischemic stroke, and pulmonary embolism 1TIA = Transient ischemic attack; 2TE = Thromboembolism myocardial infarction, peripheral artery disease, aortic plaque 1. Lip GY et al. Chest 2010;137:263-272 3Prior 2. Olesen JB, et al. BMJ 2011;342:d124 3. Task Force or the Management of Atrial Fibrillation of the ESC. Eur Heart J 2010;31:236902429 What-if Scenarios • What if this patient has experienced a TIA more recently, e.g., this morning? - What investigations should be conducted; what are any differences between these investigations and those done if the TIA was experienced 3 weeks ago? - EKG, Blood work (including INR), renal function and lipid profile. • Brain/neurovascular imaging to exclude a bleed or a large infarct Expert Recommendations • Switch to a newer OAC if INR and eGFR are within normal limits • Antithrombotic therapy in CKD patients depends on eGFR - If eGFR >30 such patients should receive antithrombotic therapy according to CHADS2 score as outlined in recommendation for patients with normal renal function Poor Prognosis in Warfarin-Associated Intracranial Hemorrhage Despite Anticoagulant Reversal Dowlatshahi D, et al. Stroke 2012. DOI: 10.1161/STROKEAHA.112.652065 Background • Anticoagulant-associated ICH (aaICH) presents with large hematoma volumes, high risk of expansion, worse outcomes than spontaneous hemorrhage • Prothrombin complex connectrates (PCC) indicated for urgent reversal of anticoagulation Dowlatshahi D, et al. 2012. DOI: 10.1161/STROKEAHA.112.652065 CanPro Registry • Determined outcomes in patients (N=141) with aaICH treated with PCC • Prospective inpatient registry of inpatients with aaICH treated with Octaplex at stroke centres: - Calgary, Edmonton, Ottawa • Primary outcomes: - INR correction - Thrombotic events - In-hospital mortality Dowlatshahi D, et al. 2012. DOI: 10.1161/STROKEAHA.112.652065 Low Rate of Thrombotic Events Thrombotic events associated with prothrombin complex concentrates (PCC) therapy Time from PCC infusion Warfarin Indication Ischemic stroke 21 days Atrial fibrillation Ischemic stroke 5 days Atrial fibrillation Ischemic stroke 1 day Atrial fibrillation Deep vein thrombosis 30 days Atrial fibrillation Deep vein thrombosis 21 days Deep vein thrombosis Myocardial infarction 28 days Atrial fibrillation Myocardial infarction 7 days Pulmonary embolism Thrombotic Event Type • 30 day thrombotic event rate was 5% • Only 3 events within 7d of therapy (2%) Dowlatshahi D, et al. 2012. DOI: 10.1161/STROKEAHA.112.652065 Hematoma Growth Significant hematoma growth despite INR correction with PCC. This patient was treated with 1000 U of PCC and 10 mg vitamin K 98 minutes after baseline CT scan. Repeat INR was 1.3, 42 minutes after PCC treatment and 1.2 the next day. INR = international normalized ratio; PCC = prothrombin complex concentrate Dowlatshahi D, et al. 2012. DOI: 10.1161/STROKEAHA.112.652065 Poor Outcomes Outcome by anticoagulant-associated ICH Number In-hospital mortality* Discharge mRS (Median IQR)† Intraparenchymal 71 30 (42.3% 5 (3)‡ Subdural 61 21 (34.4% 3 (4)§ Epidural 1 0 3 Subarachnoid 8 1 (12.5%) 3 (3) Intracranial hemorrhage type ICH = intracranial hemorrhage; mRS = modified Rankin Scale; IQR = interquartile range *P = 0.3; †P=0.012; ‡mRS missing in 9; §mRS missing in 2 Dowlatshahi D, et al. 2012. DOI: 10.1161/STROKEAHA.112.652065 Conclusion • Prothrombin complex concentrates (PCC) therapy rapidly corrected INR in the majority of patients with anticoagulant-associated ICH, yet mortality and morbidity rates remained high • Outcomes after anticoagulant-associated ICH can be devastating even with a reversal strategy Dowlatshahi D, et al. 2012. DOI: 10.1161/STROKEAHA.112.652065 Expected number of fatal hemorrhages, intracranial hemorrhages, strokes and deaths with different antithrombotic treatments 1. Eikelboom JW, et al. J Thromb Hemost 2012:10;966-968. The potential role of antidotes Agent Half life Antidote Use Heparins 1 hr Protamine CABG LMWH 3-6 hrs Protamine* Rare New OAC 6-18 hrs Nil ?? Fonda 17-21 hrs Nil Rare Warfarin DAPT 20-60 hrs K, PCC, FFP 7-10 d Platelets† Common Common *Protamine (partial). †Platelets (partial for clopidogrel) Management of Bleeding in Patients Treated with Dabigatran Mild bleeding Delay next dose or discontinue treatment as appropriate 1. van Ryn J, et al. Thromb Haemostat 2010;103:1116-1127 2. Hankey GJ & Eikelboom JW. Circulation 2011;123:1436-1450 Management of Bleeding in Patients Treated with Dabigatran Moderate to severe bleeding • Stop dabigatran • Monitor aPTT and TT • Oral charcoal (if within 2 hr of drug ingestion) • Mechanical compression • Fluid replacement and hemodynamic support • Blood product support • Surgical intervention Life threatening bleeding • Consider rFVIIa or PCC* • Charcoal filtration* or hemodialysis *Recommendation based only on non-clinical data (no experience in patients) aPTT = activated partial thromboplastin time TT=thrombin time rFVIIa=recombinant factor VIIa PCC=prothrombin complex concentrates Bleeding continues Adapted from: 1. van Ryn J, et al. Thromb Haemostat 2010;103:1116-1127 2. Hankey GJ & Eikelboom JW. Circulation 2011;123:1436-1450 3. Crowther MA & warkentin TE. J Thromb Hemostat 2009;7 (Suppl 1):107-110 4. Pradax Monograph 2010, Boehringer Ingelheim Canada Ltd Summary/Conclusions • Bleeding is the most common complication of antithrombotic therapy • Prevention is better than cure • Careful management of interruption and general measures are foundation • Specific measures (hemostatic agents, charcoal, dialysis) are available but will be rarely needed • When considering anticoagulation, all AF patients should have appropriate assessment of both stroke and bleeding risk using validated risk assessment tools • In cases of minor bleeding, hold 1 or 2 doses of the anticoagulant and eliminate any unnecessary concomitant medications that may increase bleeding risk Rich Multimedia Simple Navigation Reg i ster at w w w. eDu cateh eal th . ca Peer Reviewed Content Interactive Models