CardiacDrugs
advertisement

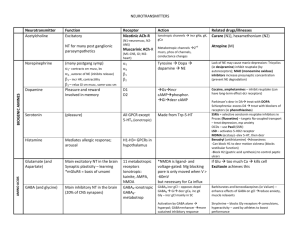
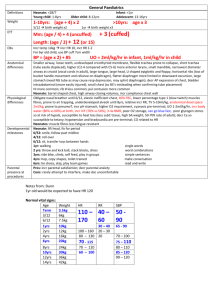
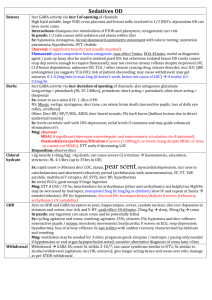
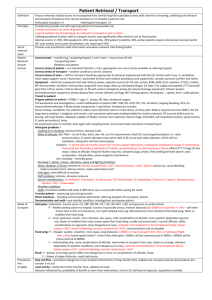
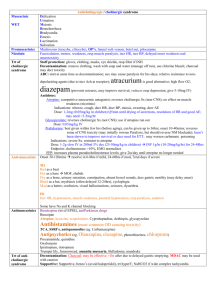
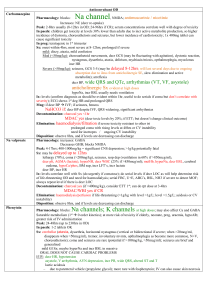
Drugs used in Heart Failure, Angina, and Arrhythmia But, first, some muscle review! Regulation of cardiac myocyte Ca2+ flux Regulation of cardiac contractility by β-adrenergic receptors Cellular Mechanisms of Contractile Pathophysiology Drugs used in Heart Failure • Heart failure: insufficient cardiac output to adequately perfuse the tissues, despite normal filling of the heart. • Congestive heart failure: combined right and left heart failure to produce pulmonary congestion and peripheral edema. • Causes: hypertension, valvular disease, cardiomyopathy, and most commonly, coronay artery disease. Drugs used in Heart Failure (cont’d) • Low cardiac output incr sns activity stimulates the rate and force of the heart beat and maintains bp by incr vascular resistance. • In the failing heart, this afterload further decr cardiac output. • The resultant decr renal blood flow renin secretion and incr plasma and angiotensin and aldosterone levels • Na+ and H2O retention incr the blood vol and bp incr P(edema). Drugs used in Heart Failure (cont’d) • These compensatory Δs at first help maintain cardiac output, but in the long run,… • Lead to Δs (e.g., abnormal ventricular dilation) that incr morbidity and mortality. • Only drugs that inhibit these neurohormones involved in these compensatory Δs incr patient survival with CHF (i.e., ACE inhibitors, β-blockers). Drugs used in Heart Failure (cont’d) • Treatment of mild HF usually starts with an angiotensin converting enzyme (ACE) inhibitor. - decr load on the heart. - decr symptoms. - slow disease progression. - prolong life. - For more severe cases, add a diuretic (e.g., bendroflumethiazide, furosemide). - For severe cases, in which a ACE inhibitor and diuretic fail, then an inotropic drug (e.g., Digoxin), which incr the force of cardiac muscle contraction by incr the rise of [Ca2+]cyto that accompanies each AP (inhibit the Na+/K+-ATPase). [See below] - β-blockers may be added. - Additional diuretics (next time) may be added. ACE Inhibitors • The most appropriate vasodilators used in HF, because they decr both arterial and venous resistance. • Preventing the incr in (vasoconstrictor) angiotensin II that is often present in HF. • Result: Incr cardiac output and because of the decr in renovascular resistance, there is an incr in RBF… • This, plus the decr in aldosterone, incr Na+ and H2O excretion decr blood vol and venous return to the heart. • Also decr direct growth action that angiotensin has on the heart. • [Angiotensin antagonists (e.g., losartan)may not have the same benefits as ACE inhibitors]. β-Receptor Antagonists (β Blockers) • Acutely, β-blockers can decrease myocardial contractility and worsen HF. • Long-term, however, administration has been shown to improve the survival of stable patients with HF (blocking the damaging effects of overactive sympathetic activity). • Start with a low dose and gradually incr over wksto-mos. • Carvedilol, bisoprolol, and metaprolol, given with an ACE inhibitor and diuretic for ~1 yr has been shown to reduce mortality from 11-17% to 712%. Inotropic Drugs • Digoxin – a cardiac glycoside extracted from foxglove leaves (Digitalis sp) is the most important inotrope. • Increase the contractile force. • Particularly indicated in patients with atrial fibrillation. • Inhibits the Na+/K+-ATPase, which is responsible for Na+/K+ exchange across the muscle cell membrane incr [Na+]in incr [Ca2+]in incr force of myocardial contraction. • Digoxin and K+ ions compete for a “receptor” (Na+/K+ATPase) on the ext membrane. • So, the effects of digoxin may be dengerously incr by hypokalemia, produced, for example, by diuretics. Positive Inotropic Mechanism of Digoxin Inotropic Drugs (cont’d) • Direct Effects: - AP and refractory period are shortened because.. - The incr [Ca2+]in stimulates K+ channels. - Toxic concentrations cause depol and oscillatory depolarizing after pot appear after normal Aps (caused by incr [Ca2+]in. - If these delayed afterpot reach T0, Aps are generated, causing ‘ectopic’ beats. -With incr toxicity, the ectobic beat itself elicits further beats, causing a self-sustaining arrhythmia (vent tach), which may vent fibrillation. Inotropic Drugs (cont’d) • Indirect Effects: – Digoxin incr vagal activity and faciliates muscarinic transmission to the heart. This… i. Slow HR ii. Slows atrioventricular conductance. iii. Prolongs the refractory period of the atrioventrivular node. Effects on Other Organs: Digoxin may cause anorexia, nausea, vomiting or diarrhea by affecting the smooth muscle of the gut. Inotropic Drugs (cont’d) • Toxicity: -Digoxin toxicity is quite common because arrhythmias can occur at concentrations that are only 2-3 x that of the optimal therapeutic dose. - Treatment may entail K supplements, antiarrhythmic drugs (lidocaine or phenytoin) or even digoxin-specific Ab fragments (Fab). Sympathomimetic Agents • Activate cardiac β-receptors AC cAMP phosphorylation of L-type Ca2+ channels (opens) incr [Ca2+]influx and the force of myocardial contraction. • Dobutamine used in acute severe HF. • Dopamine incr renal perfusion by stimulates dopamine receptors in the renal vasculature. Drugs Used in Angina Drugs Used in Angina – Pathogenesis of Acute Coronary Syndrome Drugs Used in Angina • Angina pectoris – ischemia of the heart muscle as a result of coronary artery occlusion or blockage. • Drugs use to decr the work load of the heart and hence, O2 demand. • Nitrates are the 1st-line drugs peripheral vasodilation, especially in the veins by acting on vascular smooth muscle that involves the formation of NO and [cGMP]cyto. Nitrates (cont’d) • The cGMP pooling of blood in the veins decr venous return and the ventricular vol is decr. • Decr in the distension of the heart wall decr O2 demand and the pain is quickly relieved. Nitrates • Short-acting nitrates: Glycerol trinitrate (sl, tablet, or spray) acts for ~ 30 min. -More useful in preventing attacks than in stopping them once they have begun. -Patches (transdermal) have longer duration of action (~ 24 hr). • Long-acting nitrates are more stable and effective for several hr. – Isosorbide dinitrate widely used, but metabolized rapidly by liver. – Isosorbide mononitrate (active metabolite) of dinitrate avoids the variable absorption and unpredictable 1st pass metabolism of the dinitrate. Nitrates (cont’d) • Adverse effects: Aterial dilation headaches, hypotension and fainting, and in severe cases, reflex tachycardia. - Can be counteracted with β-blockers. - Prolonged high doses can methemaglobinemia. Mechamism of action: Starts with formation of nitrite ions (see figure). Nitrates (cont’d) • Tolerance to nitrates occurs regularly, but is poorly understood. • But, perhaps depletion of sulphydral group donors may be involved, because tolerance to nitrates in vitro can sometimes be reversed by N-acetylcysteine. -Peroxynitrite formed from NO inhibits cGMP formation from GTP. β-Adrenoceptor Antagonists • Used as an angina prophylaxis. • Better to use cardio-selective (e.g., atenolol, metoprolol) β-blockers, rather than nonspecific ones (propranolol). • All β-blockers must be avoided in asthmatics as they may ppt bronchospasms. Calcium Antagonists • Widely used for angina and with fewer sideeffects than with the β-Blockers. • Ca antagonists block L-type VG Ca channels in arterial smooth muscle relaxation and vasodilation. • Ca channels in the myocardium and conducting tissues of the heart are also affected by Ca antagonists, which… • Produce negative inotropic effects by decr Ca2+ influx during the plateau phase of the AP. Calcium Antagonists (cont’d) • Dihydropyridines (e.g., nifidipine, amlopidine) have relatively little effect on the heart because they have much higher affinity for channels in the inactive state. • Such channels are found more in vascular smooth muscle because it is more depolarized than cardiac muscle (50 vs. 80 mV). • At clinical used doses, vasodilation reflex increase in sympathetic tone that mild tach and counteracts the mild inotropic effect. • Alopidine < nifidipine, verapamil < diltiazem depress the SA node mild resting bradycardia. • Verapamil binds preferentially to open channels and is less affected by the RMP. • Conduction at the AV node is slowed and slows the ventricular rate of atrial arrhythmias. Calcium Antagonists (cont’d) • The negative inotropic effects of verapamil and diltiazem are partially offset by the reflex incr in adrenergic tone and the decr in afterload. • Tobacco smoking: Smoking is prothromic and atherogenic – it decr coronary blood flow and the nicotine-induced rise in HR and bp incr O2 demand of the heart. – Also, carboxyHb decr O2-carrying capacity of Hb. – Some patients markedly improve on giving up smoking. Pharmacologic Management of Acute Coronary Syndrome Drugs used in Arrhythmia • Rhythm of the heart determined by pacemaker cells in the SAN. • Supraventrocular arrhythmias arise in the atrial myocardium (AVN), whereas ventricular arrhythmias arise in the ventricles. • Ectopic focus: firing at a higher rate than the normal SAN cells. • Re-entry mechanism: Delayed APs (some pathology) re-invade near-by muscle fibers, which, no longer being refractory, again depolarize, establishing a loop of depolarizaiton (circus movement). Drugs used in Arrhythmia (cont’d) Three Classes: 1. Supraventricular arrhythmias 2. Ventricular arrythmias 3. Drugs used in both. The Action Potential in Skeletal and Cardiac Muscle Figure 20.15 Drugs used in Arrhythmia (cont’d) Drugs used in Supraventricular arrhythmias • Adenosine stimulates A1-adenosine receptors and opens Ach-sensitive K+ channels. - This hyperpolarizes the cell membrabe in the AVN and slows conduction in the AVN (by inhibiting Ca2+ channels). • Digoxin stimulates vagal activity Ach release which slows conduction and prolongs the RP in the AVN and Bundle of His. - By delaying atrioventricular conductance, digoxin incr the degree of block and slows and strengthens the ventricular beat. • Verapamil blocks L-type Ca channels, especially on the AVN, where conduction is entirely dependent on Ca2+ spikes. - Also inhibits Ca2+ influx during the plateau phase of the AP and therefore, has negative inotropic action. Drugs used in Arrhythmia (cont’d) Drugs used in ventricular arrythmias • Class 1B agents block VD Na+ channels. • Lidocaine (iv) used after myocardial infarction. - blocks inactivated Na+ channels. - works in ischemic (anoxia causes depol and antithrombogenic activity), but not healthy, tissue. Drugs used in Arrhythmia (cont’d) Drugs used in supraventricular and ventricular arrythmias • Class IA agents block open VD Na+ channels. • Slow Phase 0 and lengthen the RP • Produce a freq (use)-dependent block. • During diastole, when the Na+ channels are closed, Class IA agents dissoc rel slowly; so, if the freq is high, drug is still bound to the channel, which, therefore, cannot contribute to the AP. Drugs used in Arrhythmia (cont’d) Drugs used in supraventricular and ventricular arrythmias • Disopyramide (po) and quinidine to prevent recurrent ventricular arrythmias. - has negative inotropic effects. - may cause hypotension and may aggravate cardiac failure. - Other side-effects: nausea, vomiting, marked anticholinergic effect. Drugs used in Arrhythmia (cont’d) Drugs used in supraventricular and ventricular arrythmias • Class IC agents dissociate very slowly from Na+ channels and strongly depress myocardial conduction. - Flecainide – used mainly in prophylaxis of paroxysmal atrial fibrillation. - has negative inotropic effects. Drugs used in Arrhythmia (cont’d) Drugs used in supraventricular and ventricular arrythmias • Class III agents slow the repolarization (Phase 3) and prolong the AP and RP in all cardiac tissues. • Amiodarone blocks several channels (e.g., K+ and inactivated Na+ channels) and β-adrenoceptors. - Often effective when other drugs have failed, but should be used sparingly, as it causes serious sideeffects (e.g., photosensitivity, thyroid disorders, neuropathy, and pulmonary alveolitis). Sotalol has both Class III and Class II (β-blocking) actions, but lacks the side-effects of amiodarone, but has the side-effects of β-blockers.