Continuing Competence Frameworks
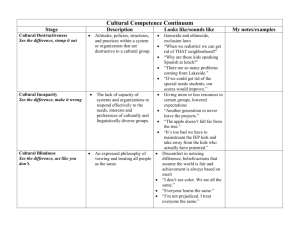
advertisement

OPENING PANDORA'S BOX Education in Nursing, Midwifery and Health Science Research Group Symposium: Confidence in Competence 11 February 2015 Associate Professor Rachael Vernon, RN, PhD Associate Head of School (Academic) School of Nursing and Midwifery University of South Australia Fulbright Scholar This presentation seeks to Explore the interface between professional regulation and competence to practice, particularly in relation to continuing education and performance of competence Explore whether public safety can be assured through performance of competence, or awareness of competence or indeed incompetence Research Question Can performance awareness / insight be identified, measured and assured, and is this preferable to the measurement of competence in clinical performance (at a given point of time), or in relation to requirements for initial registration, registration renewal / recertification? Research Overview Builds on two previous studies Evaluation of the Continuing Competence Framework (Vernon, Chiarella, Papps & Dignam, 2010) and The International consensus model for the assessment of Continuing Competence (Vernon, 2013) Examines aspects of competence assessment to differentiate between performance competence and assessment of insight into, or awareness of competence, or indeed incompetence... Purpose To analyse the assessment and adjudication of nurses with performance related notifications for competence, to: Ascertain any relationship between CPD, recency of practice and performance competence Explore if remediation provides any guarantee of performance competence Identify any relationship between awareness/insight of competence and performance competence Classify how decisions are made related to continuing registration, sanctions or deregistration Continuing Education Ensures Competence to Practise and Assures Public Safety? Previous Findings The purpose of nursing regulation is protection of the public, in many countries it is a legislative mandate Public right to expect that RNs are competent Similarities in legislative requirements, role and purpose of Regulatory Authorities in Australia, Canada, Ireland, New Zealand, the United Kingdom and the United States of America Education and practice standards for RNs are similar between countries Consensus agreement, revalidation, recertification, reregistration should occur annually, associated with requirement to declare/demonstrate the ability to meet required standard of continuing competence Strong similarities in definitions of competence and continuing competence exist Similarities in models for assessment of continuing competence Consistency between the indicators of competence, continuing competence and assurance of public safety Most common 'competence' indicator: Examination Most common 'continuing competence' indicators: CPD, Practice Hours, Self Declaration, Self/Peer Evaluation Issues of validity, reliability and efficacy within and between models, and indicators of continuing competence Influenced by individuals - behavioural and attitudinal traits Variation in distinction between core and higher levels of competence, and the impact of behaviours i.e. ethical comportment and insight Competence is defined as… “the combination of skills, knowledge attitudes, values and abilities that underpin effective and/or superior performance in a profession/occupational area and context of practice” (Nursing & Midwifery Council, 2009). Practice is defined as… Any role in which the individual uses their skills and knowledge as a nurse and/or midwife. For the purpose of the registration standard, practice is not restricted to providing direct clinical care. It also includes working in non-clinical relationship with clients, working in management, administration, education, research, advisory, regulatory or policy development roles, and any other roles that impact on safe, effective delivery of services in the profession and/or use their professional skills (Nursing & Midwifery Board, 2014) Historical overview… National competency standards first adopted by ANMC in early 1990s ANMC worked in conjunction with national state and territory authorities (NMRAs) “to help nurses and midwives to deliver safe and competent care” (http://www.ahpra.gov.au/Search.aspx?q=national%20competency%20standards) National legislation - Health Practitioner Regulation National Law 2009 (Qld), came into effect 1 July 2010 Health Practitioner Regulation National Law (South Australia) 2010 Australian Health Practitioner Regulation Agency (APHRA) - supports the national boards to implement the National Scheme NMBA (31/08/09) – Responsible for regulation of nurses & midwives in Australia; ownership of the national competency standards ANMAC (24/11/10) – Independent accrediting authority for nursing & midwifery professions under the National Scheme Continuing competence is a requirement stipulated in the National Law. Continuing Competence Frameworks Principle function – quality assurance mechanism Promotes consistency of competence standards and assessment processes Regulatory tool that facilitates the assessment and monitoring of the continuing competence of the profession, and as such they have a role in assuring and ensuring public safety Ensures consistency in the monitoring of continuing competence – annual basis Demonstrates to public that the nursing profession is cognisant of / has mechanisms to assess the competence and continuing competence of the profession Continuing Competence Frameworks Australia Nursing and Midwifery Board of Australia (National Legislation and National Framework) Canada Canadian Council of Registered Nurse Regulators (CCRNR 2011) (Incorporated Federated model - National principles - no National Framework) Revalidation of registration annually Maintain a professional portfolio Formal self-declaration of competence annually Practice – must have practised in previous 5 years or completed return to practice programme – statutory declaration from individual or employer indicating hours spent in practice Continuing Professional Development (CPD) minimum of 20 hours annually 2% Audited Annually National legislation, Health Practitioner Regulation National Law 2009 (Qld). Continuing competence is a regulatory requirement stipulated in the Act. Annual revalidation of registration Self-declaration including self-assessment Continuing education (CE) – annual requirements o Report of CE activities and evaluation of learning needs o Development of a learning plan, report on previous plan o Peer feedback / review meetings Practice – minimum of 1,125 hours in previous 5 years *Requirements vary between the legislative jurisdictions - General principles of the CNA implemented in each province *No Audit % stated Separate legislation by Province i.e. Health Professions Act 2009(BC). Continuing competence is a regulatory requirement stipulated in the Act. New Zealand Nursing Council of New Zealand (NCNZ) (National Framework) Annual recertification of practising certificate maintain a professional portfolio Self-declaration (self-assessment against practice standards, domains and competencies) o Practice - minimum of 450 hours (60 days) in previous 3 years o Professional Development minimum of 60 hours in previous 3 years o Physically and mentally able to perform in the role of a nurse *5% Nurses audited Annually National legislation, Health Practitioners Competence Assurance Act 2003 (NZ). Continuing competence is a regulatory requirement stipulated in the Act. United States of America National Council of State Boards of Nursing (NCSBN, Council of regulators Incorporated Federal Model) (National Principles requirements vary across States /Territories United Kingdom Nursing and Midwifery Council (NMC) (National Framework) Annual revalidation of registration – models vary significantly between States. Indicators include Self-declaration, including self-assessment of competence Declaration of criminal convictions, physical, mental, and drug related issues that affect the ability to provide safe effective nursing care. Continuing Education credits Practice hours *Audit requirements exist in some States – Risk based approach in some Separate legislative jurisdictions/Regulatory Boards in each State/Territory. Mutual recognition agreements some States. Renewal of registration every 3 years (certification of practise). Annual fee Maintain professional portfolio Self-declaration – complied with all Prep standards and signed notification of practice or intent to practice o Prep practice standard - minimum of 450 hours in previous 3 years or undertaken approved return to practice programme o Prep Continuing Professional Development (CPD) standard - in previous 3 years *No Audit % stated – Risk based approach One regulatory council (NMC) National legislation, The Nursing and Midwifery Order, 2001 (UK), but separate legislative jurisdictions in each country i.e. Scotland, Northern Ireland, Wales, England, Guernsey, Jersey, Isle of Man, Gibraltar, Falkland Islands etc. Competency standards (for RN) Provide a framework for assessing competence Broad and principle-based Four Domains Professional practice Critical thinking and analysis Provision and coordination of care Collaborative and therapeutic practice Annual renewal of registration Framework for assessing competency standards Important measure to ensure initial and continuing competence of nurses and midwives Guides assessment of competence against NMBA national competency standards for Ens, RNs, NPs & MWs Assessment principles Critical issues Accountability Accountability / responsibility Performance based assessment Includes - knowledge, skills & attributes Evidence based assessment Context Validity & reliability Professional judgement, recognition of cues Participation & collaboration Impartiality, confidentiality, communication Models being used to affirm continuing competence? Occur on continuum, no CC requirements – robust and comprehensive frameworks Models include: Multi – source feedback, including self-assessment 360o evaluation Portfolio Continuing Education credits / education Measurement of hours OSCE, Examination Relationship between CPD and Competence Evidence of Sufficient CPD Competent Not Competent Sufficient CPD Competent No Evidence of Sufficient CPD No CPD NO PROBLEM NO PROBLEM – they will be picked up but they are not dangerous Sufficient CPD Not Competent No CPD Not Competent PROBLEM – Won’t get picked POTENTIAL PROBLEM – Should up as they will meet renewal be picked up through lack of CPD requirements but are not safe (Chiarella and White, 2013) Continuing Professional Development Variation in understandings of what constitutes CPD Lack of understanding of how to articulate / demonstrate CPD Limited / lack of engagement in CPD Influenced by individuals' - behavioural and attitudinal traits, attitudes and beliefs Systems and operational influences Active engagement in CPD assures continuing competence to practise however does not ensure public safety Responsible and Accountable RNs as registered health professionals are: responsible, accountable, ethical, competent and committed to lifelong learning and nursing practice Individual RNs are responsible and accountable for: ensuring their own continuing competence, relevant to the required practice standards, code of conduct, and practice setting Employers and employment settings have a responsibility and role in facilitating and ensuring that their registered nurse workforce is, and continues to be, competent and complies with regulatory requirements i.e. current validation / licensure / certification Research Question Can performance awareness / insight be identified, measured and assured, and is this preferable to the measurement of competence in clinical performance (at a given point of time), or in relation to requirements for initial registration, registration renewal / recertification? Research Method Philosophical approach: interpretive and constructionist Mixed-method evaluation research design Three independent phases of data collection Phase 1- Critical analysis of case law Phase 2 - A comparative analysis of competence assessment (audit) and competence notification data over previous 3 year period Phase 3 - Interviews with key staff employed by the Regulatory Authorities Preliminary Findings Variation in understandings of what constitutes CPD Lack of understanding of how to articulate / demonstrate CPD Limited / lack of engagement in CPD Influenced by individuals - behavioural and attitudinal traits, attitudes and beliefs Systems and operational influences Active engagement in CPD assures continuing competence to practise however does not ensure public safety References Chiarella, M., & White, J. (2013). Which tail wags which dog? Exploring the interface between professional regulation and professional education. Nurse Education Today, 15. doi: 10.1016/j.nedt.2013.02.002 Vernon, R. (2014). Vernon, R. (2014). Competent or just confident? Nursing Review, series 2014, 18. Vernon, R., Chiarella, M., & Papps, E. (2013). Assessing the continuing competence of nurses in New Zealand. Journal of Nursing Regulation, 3(4), 19-24. Vernon, R. (2013). Relationships between legislation, policy and continuing competence requirements for Registered Nurses in New Zealand. Doctor of Philosophy Thesis, University of Sydney. Vernon, R., Chiarella, M., Papps, E., & Dignam, D. (2012). New Zealand nurses' perceptions of the continuing competence framework. International Nursing Review, 60(1), 59-66. Advance online publication, (2012), doi: 10.1111/inr.12001. Vernon, R., Doole, P., & Reed, C. (2011). Where is the international variation in the protection of the public? International Journal of Nursing Studies, 49(2), 243-245. Vernon R., Chiarella M. & Papps E. (2011) Confidence in competence: legislation and nursing in New Zealand. International Nursing Review, 58, 103–108. Vernon, R., Chiarella, M., Papps, E., & Dignam, D. (2010, October). Evaluation of the Continuing Competence Framework. Wellington, New Zealand: Nursing Council of New Zealand. ISBN 978-0-908662-34-0 http://nursingcouncil.org.nz/Publications/Reports