1. dia
advertisement

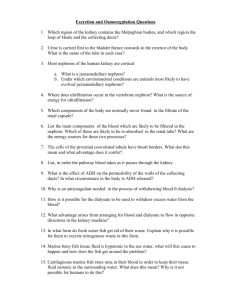
The Ad Hoc Cimmittee Reports on Estimating the Future Workforce and Training Requirements for Nephrology J. of ASN; 5(Suppl 9) May, 1997. Number of ESRD in USA: -has been growing by 12% per year since 1970s because of: - ~9% increase in prevalance (number of cases/million population) - ~2% increase in size of population - shift towards to non-white population -reason of increase in prevalance: - increase in rate of incidance (new cases/million population) - less importantly slight decline in mortality History Richard Bright (1789-1858): - causal relationship between intrinsic renal disease and the complex abnormalities of uremia (1827) Alexander V. Korányi (1866-1944): - concept of renal insufficiency based upon hyposthenuria (1898) - measurement of urine freezing point depression during water restriction makes possible to detect a clinically latent stage of uremia before its full symptomitic development (1907) Neal S. Bricker: - adapted nephrons of remnant kidney are similar to the normal nephrons in controlateral kidney – „Intact nephron hypothesis” History Robert Platt (1900-1978): - „There are two ways of looking at renal failure. The first is to consider the kidney to be so disorganized that almost anything can happen. This is convenient, usual, but rather unproductive way of looking at renal failure. The other concept is that of a kidney which has largely been destroyed by disease but in which a small proportion of the nephrons are left and are functioning under a stress and load to which a normal kidney is never subjected. The second concept seems to me to provide a much more satisfactory basis for consideration of renal function in disease.” (1951) - suggestion that secundary hyperparathyroidism is due to the acidosis and phosphate retention led to a lowering of serum calcium - „adapted nephrons” Causes of chronic renal failure 1. Glomerulonephritis Diffuse proliferative Focal proliferative Mesangio-capillary Focal glomerulosclerosis Epimemranous nephropathy Henoch-Schönlein disease Polyarteritis nodosa Systemic lupus erythematosis Wegener’s granulomatosis Goodpasture’s syndrome 2. Chronic pyelonephritis 3. Renal vascular disease Hypertensive nephrosclerosis (small vessels) Accelerated hypertension Renal artery obtruction (large vessel) Renal vein thrombosis Systemic sclerosis Diabetes mellitus 4. Metabolic causes Diabetes mellitus Gout Hypercalcaemia Hyperoxaluria Cystinosis Angiokeratoma corporis diffusum (Fabry’s disease) 5. Nephrotoxins Analgesic abuse Heavy metal poisoning – lead, gold, cadmium Worcestershire sauce 6. Obstructive Urethral strictures or valves Bladder neck obstruction Neurological bladder Prostatic enlargement Vesico-ureteric reflux Uretero-vesical obstruction Calculi Tumours Retroperitoneal fibrosis Pelvi-ureteric obstruction 7. Renal tuberculosis 8. Sarcoidosis (Bolton et al. 1976) 9. Dysproteinaemia Myeloma Amyloidosis Mixed IgA-IgM cryoglobulinaemia Waldensröm’s macroglobulinaemia 10. Miscellaneous Balkan nephropathy Sickle-cell haemoglobinopathy Japanese cadmium-nephropathy Radiation 11. Hereditary or congenital Polycystic disease Nephronophthisis (medullary cystic disease) Alport’s syndrome Cystinosis Hyperoxaluria Chronic tubular acidosis Infantile nephrotic syndrome Dysplastic kidneys Course of chronic renal failure months, years, decades renal disease nephron damage remnant nephrons hypertrophy damage of hypertrophic nephrons uremia months, years, decades renal disease nephron damage remnant nephrons hypertrophy nephron tissue volume medullary osmotic concentration H2O and urea rediffusion in remnant collecting ducts polyuria damage of hypertrophic nephrons uremia months, years, decades renal disease nephron damage nephron tissue volume remnant nephrons hypertrophy SNGFR damage of hypertrophic nephrons uremia change in glomerulotubular balance prox. tubular reabsorption increased distal osmotic load (Na , urea ) medullary osmotic concentration osmotic diuresis (10-20 x per nephron) H2O and urea rediffusion in remnant collecting ducts polyuria months, years, decades renal disease remnant nephrons hypertrophy nephron damage nephron tissue volume damage of hypertrophic nephrons uremia change in glomerulo-tubular balance SNGFR prox. tubular reabsorption medullary osmotic concentration increased distal osmotic load (Na , urea ) H2O and urea rediffusion in remnant collecting ducts osmotic diuresis (10-20 x per nephron) polyuria hyposthenuria isosthenuria (concentrating oblity ) obligate fluid and salt loss in spite of reduction in total GFR tubular damage no distal Na transport (diluting oblity ) oligo-anuria Isosthenuria in relation to the number of nephrons Specific gravity of urine 1050 1040 Concentrating ability Diluting ability 1030 Isosthenuria 1020 1010 Specific gravity of glomerular filtratum 1000 2 000 000 1 500 000 1 000 000 500 000 Number of the nephrons of two kidney 0 Dynamism of retention First phase: 100-20% GFR („reserve”) Second phase: 25-5% GFR („transitional”) protein intake: 52.5 150 g/ die 100 g/ die 50 g/ die 35 17.5 0 30 GFR 60 90 120 ml / min 75 100 % GFR 0 Na, Mg, PO4, etc Third phase: <5% („end stage”) 70 Blood carbamid- N mmol/l Stages of CRF based on GFR changes 25 50 100% 30 60 90 120 GFR, ml/min Signs and Symptoms of Uremia Behavioral, mental or neurological Depressive: fatigue, asthenia, malaise, mental dullness, shortening of concentration, memory defects sluggishness or „heaviness”, anorexia drowsiness by day, suicidal thoughts, thanatophobia, stupor precoma coma Irritative: anxiety, fasciculations, twitching, headache, cerebellar signs of ataxia, asterixis, abnormal gait, vertigo, compulsive actions, central nausea, convulsions Psychiatric: personality change, bizarre behavior (e.g. compulsive, paranoid, etc.), phobias organic psychosis, selective amnesia, denial, food and drug kleptomania Peripherial: pruritus, paresthesias, burning foot, restless leg syndrome, foot flap and drop, monoplegia paraplegia, sensory and motor defects, bladder atony and dysfunction Ophthalmic: nystagmus, miosis, asymmetric pupils (anisocoria), blurring, amaurosis, the red eye sydrome due to conjunctival irritation from calcium deposits, band keratopathy Gastrointestinal Membrane problems: cheilitis, glossitis, stomatitis, parotitis, esophatigis, enteritis, pancreatitis, colitis, ileus Functional problems: anorexia, dysgeusia and ageusia, nausea, vomiting, hematemesis, constipation, diarrhea, abdominal distention Structural problems: peptic and colonic ulceration Cardiovascular-pulmonary Pericarditis, acute and constrictive Cardiomegaly Pleuritis Congestive heart failure Change in blood pressure Arrhytmias Vascular calcification Accelerated atherosclerosis Cheyne-Stokes and/or Kussmaul breathing Hematological Anemia (normochromic normocytic) Bleeding abnormality (prolonged bleeding time, abnormal platelet aggregation) Lymphopenia, mild thrombocytopenia Dermatological Pallor Excoriations and pruritus Urea frost Purpuraand ecchymosis Rash „Pseudo-clubbed” fingers of severe hyperparathyroid bone disease „Brown nail” of uremia Cutaneous and subcutaneous calcification Peripheral tissue necrosis and ulceration Metabolic Musculoskeletal muscle pain and weakness, proximal myopathy, bone pain, bone pain, bone fractures, aseptic necrosis of bone Disturbances in multiple endocrine systems Carbohydrate intolerance Hyperlipidemia Gout and pseudogout Wasting and abnormalities in protein metabolism Sexual and reproductive Impotence Decreased libido Reduced nocturnal penile tumescence Infertility Amenorrhea Frigidity Gynecomastia Galactorrhea Immunological Reduced T-cell-mediated immune function Impaired phagocytosis and chemotaxis Atrophy of the lymphoid system including thymus Reduced immune surveillance of neoplasia Miscellaneous Reduced wound healing Hypothermia Impaired response to pyrogen Uremia Excretory failure -H2O -Na+ -H+ -HPO24-, SO24-urea, kreatinin -toxins (?!) Renal biosynthetic failure -erythropoietin -prostaglandins -kinins -1.25 (OH)2, vitamin D3 -HCO3 -NH3 Regulatory failure (disruption of homeostatically useful hormonal feedback sontrol systems) 1. distribution of hormonal control system -PTH -natriuretic hormone 2. disturbed renal (or extrarenal) catabolism of polypeptide hormones -insulin, glucagon -PTH, STH secretion 3. end-organ resistance at the receptor or postreceptor level -insulin -PTH List of suspicious agents Urea 2,3- Butylene glycol Creatinine Lipochromes Methylguanidine Glucagon Guanidinosuccinic acid Growth hormone Other guanidines Gastrin Uric acid Renin Pyridine derivatives ß2 – microglobulin Amino acids Lysozymes Aliphatic amines Retinol-binding protein Polyamines ß2 – glucoprotein Indoles Ribonuclease Myoinositol Natriuretic hormone Mannitol Middle molecule Glucuronic acid PTH Parathyreoid hormone and the uremie manifestations Nephron loss Phosphate retention Se-Ca++ Renal production Responsiveness Decreased PTH of 1.25 (OH)3 of bone to PTH metabolism in vitamin D3 kidney Absorption of Ca in gut Se-Ca++ Secunder hyperparathyreodism Effects of PTH ++ 1. Ca - content of cells 2. Cell membrane permeability changed 3. Cyclic AMP activity 4. Soft tissue calcification 5. Increased protein catabolism (protein- kinase ) Parathyreoid hormone and the uremie manifestations Excess PTH Inhibit Bone marrow Hemolysis Reduction in red marrow RNA Heme Synthesis by erythroid precursors Anemia Uremic anemia: parathyreoidectomy improvement PTH decrease utilization of iron Ca- channel blokkers decrease the hemolysis induced by PTH Experimental and clinical evidences for neurotoxicity of PTH Uremia: - increased Ca – content of brain tissue (EEG slows down) and periferial nerves (decreased conduction) - Endogen PTH may induced similar phenomen in dogs. - Adenoma of parathyreoid glands similar phenomen - In uremia the disturbance of renal motor nerves are in correlation with the concentration of PTH in the blood Increased PTH may play a role in the development of: Hypertension Myocardiopathia Hyperlipidemia Leukocytosis, dysfunction of thrombocytes Disturbance of insulin secretion Myopathia Sexual dysfunction Hypertrophy of the remnant kidney Nephrectomy (partial) remnant nephrons hypertrophy afferent vascular resistance SNGFR efferent e.g.: removal of 60% of renal mass adaptation ?! SNGFR increased by 200% Suggested mechanism for glomerulosclerosis Reduced renal mass Decrease in total GFR Systemic hypertension Endothelial damage Intraglomerular hypertension Microaneurysm formation Intraglomerular thrombosis Further in total GFR mesangial traffic of macromolecules Increased number of macrophages Mesangial expansion Liberation of growth factors Fibrosis and liberation of growth factors (platelet DGF) hyalin formation Glomerulosclerosis Observation in human medicine 1, ARF „recovery” later on: uremia 2, Painkiller induced renal dysturbances progression of renal disease continued 3, Glomerulonephritis + renal artery stenosis 4, Pregnancy RBF , GFR drugs stopped uremia better prognosis accelerated progression of renal disease Questions: 1, One „Kidney people” ( trauma, kidney donor etc.): Future prospect: How much of the kidney is lost to get hyperfiltration? 2, May hyperfiltration cause progressive renal lesion in „normal person?” (- number of nephrons decrease by age: 30 years 80 years old GFR number of nephrons ~50% - protein intake?) 3, GFR in type I diabetes increased at the beginning but only 50% gets serious renal damage Kidney disease Number of nephrons Hypertrophy of the remaining nephrons Glomerularsclerosis Hyperfiltration Agents increasing glomerular pressure Conditions deteriorating kidney function Hypertension (untreated) Hyperuricemia Generally known Ca – deposit Hyperlipidemia (triglicerid, preß lipoprotein (type IV) lipoprotein lipase Diet with high protein Diabetes mellitus Sever anemia Other important factors Chronic vasodilatory therapy ( fe. Steroids) Pregnancy Diastolic pressure > 70 mmHg Sever proteinuria Uremia 1, GFR < 10-20 % 2, H2O, Na retention oedema, circulation disturbancy 3, H+- secretion, buffer capacity metabolic acidosis ( death cc. 6.9 pH) 4, K+ - conc. (acidosis, catabolism ): 8 maeq/l 5, Urea, creatinin 6, Anemia: hemolysis , production 7, Hypertension: R-A System hypervolemia 8, Osteomalacia 9, Uremic coma death Maximal urinary osmotic concentration glomerulonephritis 1000 Intestitial nephritis 800 600 papillanecrosis 400 200 0 50 GFR (ml/min) 100