Seminar in Advanced Physiology of Exercise
advertisement

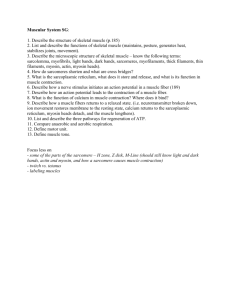
Muscle Three types of muscle: • smooth • cardiac • skeletal All muscles require ATP to produce movement. Thus, muscles are chemotransducers Skeletal Muscle • • • • • • • Muscle organization Muscle innervation Architecture and structure Excitation-contraction Fiber type characteristics Training adaptations Exam 1 (Feb 8) Skeletal muscle organization Connective tissue layers • Epimysium • Perimeysium • Endomysium Muscle fiber covering • Sarcolemma – basement membrane – plasma membrane • Plasma membrane has – membrane receptors – ion channels – integrins – satellite cells – multinuclei Muscle Architecture Effect on force output and shortening velocity Muscle Architecture Muscle architecture Muscle Architecture Parallel Unipennation Multipennation Pennation: Effect on Physiological Crosssectional Area (PCSA) Greater PCSA when fiber is at angle to line of force B A A Pennation: Effect on Force and Shortening Distance/Velocity Fiber B Fiber A Equal number of sarcomeres in both examples, but Fiber A has longer fiber and smaller PSFA than Fiber B, which allows for greater shortening distance/velocity at sacrifice of force. Identify which muscles are best suited for force; for speed A B C D Muscle Architecture • quadriceps and planter flexors designed for force production – larger pennation angles – large PCSAs • hamstrings and dorsiflexors designed for velocity – smaller pennation angles – intermediate PCSAs Muscle Architecture Summary – Muscles designed to fit purpose of joint • Muscles designed for velocity have longer fiber length and small pennation angle • Muscles designed for force have shorter fiber length and larger pennation angle Review questions 1. Describe the difference between a muscle with a fusiform architecture and one with a uni- or multipennate architecture. Identify a muscle for each type of architecture. 2. Discuss how muscle architecture affects force output and shortening velocity. Provide a general explanation as to why some muscles are designed more for rapid shortening velocity (e.g. hamstrings) or higher force output (e.g. quadriceps muscles). Muscle Innervation Motoneurons, neuromuscular junctions, motor units Motoneurons • muscle fibers innervated by large (alpha) myelinated nerves • motoneurons originate from spinal cord • nerve ending ends at neuromuscular junction • motor unit composed of motor neuron and all the fibers it innervates Action Potential • • • • depolarization – influx of Na+ repolarization – efflux of K+ refractory period – hyperpolarization threshold level – minimal stimulus required to elicit response • muscle and nerve follow “all or nothing principle” Membrane potential (mV) +20 0 -20 -40 -60 -80 Time (ms) Na+ K+ Na+ Na+ Na+ Na+ K+ Na+ Na+ Na+ Na+ channel K+ K+ K+ intracellular K+ K+ K+ Na+ Na+ Na+ Na+-K+ exchange pump K+ Na+ Na+ K+ K+ Na+ ATPase K+ ADP Pi K+ Na+ Na+ K+ channel K+ K+ Na+ ATP Na+ K+ K+ K+ K+ Na+ K+ Neuromuscular Junction Electromyography (EMG) 10.0000 5.00000 volt 0.00000 s Describe the relative weights being lifted -5.00000 -10.0000 Review questions 1. Define the motor unit. 2. Describe the events that occur as an action potential approaches the nerve terminal. 3. Explain the purpose of acetylcholinesterase and the consequences of its absence. 4. A common agent found in flea powders is a low dose of an antiacetylcholinesterase inhibitor. Explain the effects that the flea powder would have on fleas. 5. Explain the interpretation of an EMG tracing. Sarcomere Structure Skeletal Muscle Structure Cross-Sectional View of Skeletal Muscle (X40) Skeletal Muscle Structure • sarcomeres (smallest functional unit) are linked end-to-end to form myofibrils • myofibrils are bunched to form fibers • sarcomeres are composed of thick and thin filaments Scanning EM 1 4 2 3 5 Thick Filament • composed of numerous myosin protein strands • flexible “heads” protrude outward all around filament (except center) • myosin heads attach to “active” sites on actin (thin) filament • myosin heads contain ATPase to break down ATP Myosin filament Myosin Filament Thin Filament Composed of three proteins • actin - two protein strands twisted around each other, contain “active sites” • tropomyosin - thin strand laying in actin groove that covers active sites • troponin - attached to actin and tropomyosin strands; has strong affinity for Ca2+ Thin Filament Cytoskeleton (structural) proteins • M-band – located in middle of thick filament; provides structural support to myosin filaments; contains creatine kinase (CK) • Titan –connects myosin filament to Z-disk; stabilizes myosin in middle of sarcomere. • Z-disk –thin filaments attachment; composed of several cytoskeletal proteins Actin-myosin orientation Transverse Tubule • in human skeletal muscle, each sarcomere has two transverse tubules running perpendicular to fiber • T-tubules extend through fiber and have openings at sarcolemma allowing communication with plasma • cardiac fibers have only one T-tubule which lies at Z-line Sarcoplasmic Reticulum (SR) • made up of terminal cisternae and longitudinal tubules • serves as a storage depot for Ca2+ • terminal cisternae abut T-tubules • longitudinal tubules cover myofibrils and connect terminal cisternae 1. On what component does Ca2+ bind to? a. b. c. d. Sarcoplasmic reticulum Myosin heads Troponin Tropomyosin 2. What protein returns Ca2+ to the sarcoplasmic reticulum? a. b. c. d. Myosin head Ca2+ pump Ca2+ channels tropomyosin Review questions 1. Describe the myosin filament of a skeletal muscle fiber. Include a detailed description and function of the myosin head. 2. Describe the thin filament of a skeletal muscle fiber. 3. Describe the cytoskeleton proteins and their functions in the sarcomere. 4. Describe the sarcoplasmic reticulum and its role in excitation-contraction. Excitation-Contraction How muscle contracts Excitation-Contraction Coupling • action potentials, generated at neuromuscular junction travel around sarcolemma and through T-tubules • T-tubules signal SR to release Ca2+ into sarcoplasm (cytosol) • Ca2+ saturates troponin (in non-fatigued state) • troponin undergoes conformational change that lifts tropomyosin away from actin filament E-C Coupling (cont.) • myosin head attaches to active site on actin filament • after attaching to actin, myosin head moves actinmyosin complex forward and releases ADP and Pi • ATP binds with myosin head, which releases actin, and returns to original position • in resting state, myosin head contains partially hydrolyzed ATP (ADP and Pi) E-C Coupling Schematic E-C Coupling (cont.) • entire cycle takes ~50 ms although myosin heads are attached for ~2 ms • a single cross-bridge produces 3-4 pN and shortens 10 nm • as long as action potentials continue, Ca2+ will continue to be released • when action potentials cease, SR Ca2+ pumps return Ca2+ ceasing contractions • skeletal motor units follow “all or nothing” principle Excitation-Contraction 1. AP causes vesicles to release Ach 2. Muscle AP travels down ttubules 3. SR releases Ca2+ into sarcoplasm 4. Ca2+ binds to troponin 5. Myosin heads bind to actin; mysoin ATPase splits ATP 6. ATP binds to myosin heat; releases from actin 7. Crossbridge action continues while Ca2+ is present 8. When AP stops, Ca2+ pumped back to SR 9. Tropomyosin covers active sites EC Coupling QuickTime Movie of sliding filaments • http://www.sci.sdsu.edu/movies/actin_myosin.html • Click on Link • Click on Actin Myosin Crossbridge 3D Animation 3. What will happen if ATP is depleted in muscle? a. b. c. Nothing Muscle will relax Muscle will not relax 4. What will happen if sarcoplasmic reticulum of fiber is enhanced? a. b. c. d. Fiber will develop tension more quickly Fiber will relax more quickly Nothing Both a and b will occur Review questions 1. Discuss the signaling process of the T-tubules that leads to Ca2+ release by the sarcoplasmic reticulum. 2. Describe ATP hydrolysis by the myosin filament. 3. Discuss factors that could affect the rate of ATP hydrolysis by the myosin head as well as factors that affect tension development. Skeletal Muscle Fiber Types • generally categorized by histochemical criteria • innervating nerve is primary determinant of fiber type • motor units composed of homogenous fibers • all human muscles contain mixture of three general fiber types – slow twitch (ST, oxidative, red, Type I) – fast twitch (FTa, fast-oxidative, white, Type IIa) – fast twitch (FTb, glycolytic, white, Type IIx [often called IIb]) stained for myosin ATPase (pH = 10.3) (dark stained) Type I Type IIa stained for myosin ATPase (pH = 4.3) (light stained) stained for SDH (dark stained) Type IIx Muscle Twitch Characteristics frontalis/orbicularis oculi (15% ST) first dorsal interosseous (57% ST) soleus (80% ST) extensor digitorum brevis (60% ST) Fiber Type Characteristics Performance characteristics affected by: • • • • • • • size of motoneuron size of muscle fibers amount of SR Ca2+-ATPase myosin ATPase aerobic capacity (amount of mitochondria) anaerobic capacity (amount of glycolytic enzymes) Be able to explain the differences in the force responses between motor units. 5. Which fiber reaches peak tension most quickly? a. b. c. Type I Type IIa Type IIx 6. What is the reasoning for your response to Q5? a. b. c. d. e. faster myosin ATPase more Ca2+ channels more Ca2+ pumps faster action potentials none of the above are correct Exam 1 – Thu, Feb 8 • • • • • Begin preparing for exam NOW! Use posted learning objectives as basis for studying Read text to clarify material Initially, study by self, then study with classmates “Teach” each other course material; question accuracy/completeness of other’s explanations • See me if questions remain • You may start the exam at 7:45 am – Bring the medium-sized RED scoring sheet (sheet that enables you to bubble in your name) Motor Unit Recruitment Pattern – Size Principle Muscle Movements • isotonic – develops tension while changing length • isokinetic – resistance to muscle changes with muscle length to ensure equal tension development • isometric (static) – develops tension but no length change • concentric – develops tension while shortening • eccentric – develops tension while lengthening Muscle Performance Characteristics Force and power development dependent on: • • • • • • number of muscle fibers recruited muscle architecture angle of pull length of fiber velocity of shortening load place on muscle Length-Tension Relationship Length-Tension Relationship How sarcomere length affects force output This explains the length-tension relationship At which length would force output by the biceps muscle be greatest? a. b. c. d. When the arm is in full extension When the arm is flexed at 90-100º When the arm is at full flexion Strength (force) would be the same throughout the entire range of motion Force-Velocity Relationship How would the EMG activity to a leg squat during the lowering (eccentric) phase compare to the upward (concentric) phase. a. EMG activity would be the same for both phases. b. EMG activity would be greater for the concentric phase. c. EMG activity would be greater for the eccentric phase. EMG comparison of concentric and eccentric actions 10.0000 5.00000 volt 0.00000 s -5.00000 -10.0000 Muscle Spindles (sensitive to stretch) Golgi tendon organs (sensitive to strain) Resistance Training Adaptations • dependent on neural and physiological adaptations • training specificity determines adaptations Strength Training Adaptations Neural Adaptations • increased motor unit recruitment • decreased neural inhibition of motor unit recruitment • decreased antagonist muscle recruitment • increased neural coordination Muscle Fiber Adaptations • increased fiber size (both types) – increased hypertrophy (1º) – increased hyperplasia (2º) – occurs more to FT fibers than ST • little or no change of fiber types • testosterone explains only part of larger muscle mass in males How does 1. an untrained individual increase strength? 2. a trained individual further increase strength? a. neuromuscular adaptations b. hypertrophy c. both neuromuscular adaptations and hypertrophy Exercise-Induced Muscle Damage and Soreness Unaccustomed exercise stimulates sequence of events that: • diminishes performance • causes ultrastructure damage • initiates inflammatory reaction • causes delayed-onset muscular soreness (DOMS) Muscle Damage/Repair Overview • damage occurs during lengthening (eccentric) movements • damage commonly occurs to sarcolemma, Zdisk (streaming), T-tubules/SR, myofibrils, cytoskeleton • initial muscle damage followed by inflammatory-induced damage • produces muscle swelling • affects FT fibers more than ST fibers • repair begins ~3 d post-exercise Z-line streaming Muscle Fiber Damage – Sarcolemma damage Exercise-Induced Muscle Damage • extent of injury more related to length than force or velocity • weaker fibers become overstretched, which become damaged (Morgan, 1990) Stages of Muscle Damage 1. During exercise: Mechanical (strain) damage results in: – sarcolemma damage – SR damage – myofibrillar damage – Ca2+ influx 2. After exercise: Inflammatory response causes: Effects of Elevated intracellular Ca2+ • activates proteases – damages cytoskeleton proteins • activates phospholipases – generates free radicals – damages plasma membranes Acute Phase Response Promotes clearance of damaged tissue and initiates repair • circulating neutrophils (w/in 1-12 h) and monocytes (w/in 1-3 d) – enters injury site and phagocytizes damaged tissue – release cytotoxic factors (e.g., oxygen radicals) Typical Times of Peak Effects • Ultrastructural damage 3-d postexercise • DOMS 1-2 d postexercise CK from 60-min Downhill Running 1000 CK (IU) 800 600 400 200 0 pre 0 24 48 72 Postexercise sampling time (h) Kolkhorst, unpublished observations Effects on Performance/Soreness • greater damage to FT fibers • prolonged strength loss – primary cause failure of SR-Ca2+ release – ultrastructure damage secondary cause of strength loss • muscle swelling/DOMS – DOMS caused by tissue breakdown products that sensitize pain receptors Muscle Repair • macrophage infiltration required for activation of satellite cells • satellite cells located between basement membrane and plasma membrane • in response to signal from injury site, satellite cells migrate to injury • differentiate into myoblasts, which fuse into myotubes Muscle repair Immediately after crush injury 2 days • At 2 d, damaged fibers have undergone necrosis, with digestion/removal by macrophages. • At 5 d, several newly formed myotubes are visible. 5 days • At 10 d, myotubes have transformed into fibers, many of which have linked up with fibers stumps on either side. Which type of activity would likely cause the most severe DOMS or muscle damage? a. level running (involves about half concentric and half eccentric movements) b. rowing exercise (involves mostly pulling motion, a concentric movement) c. running down stadium stairs (involves more eccentric than concentric movements) d. cycling (entirely concentric movements) e. none of the above would cause DOMS Eccentric exercise a. causes the greatest damage at the shortest muscle lengths. b. causes the greatest damage to ST fibers. c. initiates an inflammatory response that causes further myofibril damage. d. stimulates macrophage infiltration to the damaged area, which is essential for muscle repair. e. both c and d are correct The greater the load placed on a muscle during a shortening movement, the _____ it can shorten. This illustrates the _____ relationship of skeletal muscle mechanics. a. slower; power-load b. slower; length-tension c. faster; length-tension d. slower; force-velocity e. faster; force-tension According to the Force-Velocity relationship, how does force output of a fiber when shortening compare to when it is forced to lengthen? a. b. c. force output is greater when it is allowed to shorten force output is equal regardless of shortening or lengthening force output is less when it is allowed to shorten