Infection Control - Respiratory Therapy Files
advertisement

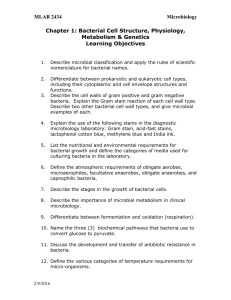
Infection Control Definition of Terms • Asepsis – Absence of disease-producing microorganisms • Sterility – Complete absence of all microorganisms Definition of Terms • Pathogen – Microorganism capable of causing disease in humans • Hospital acquired infections (nosocomial infections) – Infection acquired during the course of hospitalization. – Accounts for 2 million infections, 4.5 billion dollars and 90,000 deaths annually in the U.S. Definition of Terms • Cross contamination – Transmission of microorganisms between places or persons • Contamination – Presence of a microorganism in an otherwise sterile environment Definition of Terms • Virulence – Heightened ability of an organism to produce infection in its host • Exotoxin – Poisonous substance produced primarily by gram positive bacteria and secreted into surrounding media; some are extremely lethal Definition of Terms • Endotoxin – Poisonous substance produced by gram negative bacteria and released when the bacterial cell is destroyed • Vector – Insect, animal, or other carrier that transfers an infecting agent from one host to another Etiology • Primary source of HAI’s are humans (visitors, personnel, other patients) • There are 3 major routes for transmission of human sources of infection in the hospital: – Direct and indirect contact • Direct contact - Person to person (infection from the host to another) • Indirect contact – Transfer of organism thru a contaminated object or intermediate person (unwashed hands passing a pathogen picked up from one patient and passing it on to another patient) • The most frequent route of pathogen transmission in the hospital setting is via indirect contact Etiology • There are 3 major routes for transmission of human sources of infection in the hospital (cont): – Respiratory droplets • Coughing, sneezing, talking • Use mask within 6 feet of patient or when entering room – Airborne droplet nuclei (respirable particles < 5 micrometers) • Remains suspended in air for long periods • TB, Varicella, Variola, Rubeola, SARS • Requires negative pressure room • Requires N-95 fit tested mask Infection Prophylaxis • The techniques used by most hospitals to reduce host susceptibility to infection focus mainly on the employee. These include: – Immunizations and chemoprophylaxis – OSHA mandates that employers provide Hepatitis B vaccinations – Postexposure chemoprophylaxis is recommended after exposure to B. pertussis, N. meningitides, B. anthracis, Influenza virus, HIV, and group A streptococci – Hand washing for at least 15 seconds is still the single most important procedure for reducing hospital acquired infections Infection Prophylaxis – Multi-dose vials of saline, water, and medications should be time/dated when opened and discarded if contaminated and/or not used within 24 hrs. – Most disposable respiratory equipment should be discarded and replaced every 48 hrs., This includes ventilator circuits large and small volume nebulizers and humidifiers. – Once a piece of equipment has been used and becomes contaminated, that piece of equipment must be thrown out if disposable, cleaned or sterilized – Gloves are not 100% pathogen proof. – Hand washing between patients is not the same hand washing you would use going into a NICU or OR Biohazardous Waste • Defined as: – Laboratory waste including specimen cultures, live and attenuated vaccines, surgery specimens and blood – Waste containing discarded materials/equipment contaminated with exudate or secretions from patients required to be isolated – Contaminated sharps including needles, blades, broken glass, or any items capable of cutting or piercing – Any disposable item such as dressings, gloves, gowns etc., visibly soiled with recognizable human blood or body fluids Biohazardous Waste • What it is not: – Unless it contains fluid blood, the following are NOT considered biohazardous waste pursuant to the California Department of Health • Urine • Feces • Saliva/sputum • Nasal secretions • Sweat • Tears • Vomit • Always refer to your clinical sites policy and procedures Infection Prophylaxis • Disposal of biohazardous medical waste – All glass, sharps, guide wires, stylets must be placed in an approved sharps container. – Dry wound dressings, dry gloves, diapers and other forms of contaminated equipment not saturated or dripping with blood or other body fluids may be placed in regular trash – Wet, dripping or fully saturated dressings, IV tubing and their empty bags, ventilator circuits, HME’s, and other pieces of equipment with blood, liquid secretions, liquid mucous, must be placed in a red biohazard bag. – Any equipment coming out of an isolation room including PPE must be placed in a red biohazard bag or sharps container Infection Prophylaxis Biohazard bag Yellow sharps containers and bags are for chemotherapy waste Sharps container Infection Prophylaxis • The 5 key recommended components of an infection control program in the hospital setting are: – – – – – Surveillance Investigation Prevention Control Reporting Classification of Organisms • Eukaryotic – Types • Protozoa • Fungi • Slime molds • Algae (except blue-green) Classification of Organisms • Prokaryotic – Types • Bacteria • Rickettsiae • Mycoplasmas • Blue-green algae Classification of Organisms • Viruses – Simple nucleic acid chain (DNA or RNA) – Has a protein coat – Some debate as to whether they can be classified as living organisms Bacterial Environments Bacterial Environments • Bacterial requirements: – Growth medium – Atmospheric gas – Temperature – pH range – Moisture – Light Requirements For Bacterial Growth • Growth medium – Varies by bacteria from simple to complex nutrients – Simple nutrients • Water, carbon, nitrogen, oxygen, calcium, potassium, etc. – Complex nutrients • Sugars, amino acids, blood products Requirements For Bacterial Growth • Atmospheric gas requirements – Obligate aerobes • Require oxygen for reproduction – Obligate anaerobes • Only reproduce in an oxygen free environment – Aero tolerant anaerobes • Unaffected by exposure to oxygen Requirements For Bacterial Growth • Atmospheric gas requirements (cont) – Facultative anaerobes • Reproduce under aerobic or anaerobic conditions – Microaerophilic anaerobes • Reproduce best at low oxygen levels; high oxygen levels are inhibitory Requirements For Bacterial Growth • Atmospheric gas requirements (cont) – Chemolithotrophic and photolithotrophic bacteria use carbon dioxide as principal source of carbon Requirements For Bacterial Growth • Temperature requirements – Psychrophilic • —5° C to 30° C (optimum range 10° C - 20° C) – Mesophilic (pathogenic) • 10° C to 45° C (optimum range 20° C - 40° C) – Thermophilic • 25° C to 80° C (optimum range 50° C to 60° C) Requirements For Bacterial Growth •Hydrogen ion (pH) requirements o Pathogens o Acidophiles 7.2 to 7.6 (optimum range) 6.5 to 7.0 o Neutrophiles 7.5 to 8.0 o Alkalophiles 8.4 to 9.0 Requirements For Bacterial Growth • Moisture – Essential for all bacterial growth • Light – Most bacteria prefer darkness – Ultraviolet and blue light are destructive to bacteria Bacterial Shapes • Spherical – coccus • Rod – bacillus • Spiral – spirillum, spirochete • Comma-shaped – vibrio • Spindle-shaped – fusiform Staining • Gram staining of bacteria • Purpose: – To separate bacteria into two general categories: gram positive and gram negative bacteria – The technique is based on the fact that the Gram positive cell wall has a stronger attraction for crystal violet when Gram's iodine is applied than does the Gram negative cell wall Staining • Gram's iodine is able to form a complex with the crystal violet that is attached more tightly to the Gram-positive cell wall than to the Gram-negative cell wall. This complex can easily be washed away from the Gramnegative cell wall with ethyl alcohol. Gram-positive bacteria, however, are able to retain the crystal violet and therefore will remain purple after DECOLORIZING with alcohol. Gram Stain Bacteria • Gram positive organisms stain blue or violet • Gram negative organisms stain red or pink Acid-Fast Stain Acid-fastness is a physical property of some bacteria referring to their resistance to decolorization by acids during staining procedures • Used to identify bacteria of the genus Mycobacterium • Acid-fast bacteria appear red against a blue background Acid-Fast Stain • The primary stain used in acid-fast staining, carbolfuchsin, is lipid-soluble and contains phenol, which helps the stain penetrate the cell wall. This is further assisted by the addition of heat. The smear is then rinsed with a very strong decolorizer, which strips the stain from all non-acid-fast cells but does not permeate the cell wall of acid-fast organisms. The decolorized non-acid-fast cells then take up the counterstain. Common Gram Positive Bacteria • Bacillus anthracis – Rod-shaped, arranged in chains, spore forming – Secretes endotoxin – Causes skin infections, septicemia, enteritis, meningitis, anthrax, and pneumonia (wool-sorter’s disease) Common Gram Positive Bacteria • Clostridium botulinum – Rod-shaped pairs, spore forming – Causes botulism Common Gram Positive Bacteria • Clostridium perfringens – Rod-shaped in pairs, spore forming – Causes gas gangrene Common Gram Positive Bacteria • Clostridium tetani – Rod-shaped in pairs, spore forming – Causes tetanus Common Gram Positive Bacteria • Streptococcus pneumoniae – Coccus, arranged in chains, may produce capsules – Aerobic – Causes lobar pneumonia; may cause empyema, septicemia, meningitis, and peritonitis Common Gram Positive Bacteria • Staphylococcus aureus – Coccus arranged in irregular, grapelike clusters – Aerobic, facultative anaerobe – Produces exotoxin and endotoxin – Causes pneumonia, empyema, and wound infection Common Gram Negative Bacteria • Pseudomonas aeruginosa – Rod-shaped, found as a single organism – Aerobic, facultative anaerobe – Responsible for up to 10% of all hospital acquired infections – Causes pneumonia with characteristic green odoriferous sputum; also causes wound infection, urinary tract infection, empyema, meningitis, and septicemia Common Gram Negative Bacteria • Serratia marcescens – Rod-shaped – Aerobic – Causes empyema, septicemia, wound infections; responsible for some hospital epidemic Common Gram Negative Bacteria • Escherichia coli – Rod-shaped, found as a single organism – Aerobic – Responsible for 45% of all nosocomial infections – Causes necrotizing pneumonia, septicemia, endocarditis, meningitis, wound infections, and urinary tract infections Common Gram Negative Bacteria • Klebsiella pneumoniae – Short rod found as a single organism, produces capsules – Aerobic, facultative anaerobe – Causes necrotizing pneumonia with characteristic “red currant jelly” sputum; also causes lung abscesses, endocarditis, and septicemia Common Gram Negative Bacteria • Hemophilus influenzae – Minute rod found as a single organism – Aerobic, facultative anaerobe – Common cause of epiglottitis in children; also causes meningitis, laryngitis, croup, and sub acute bacterial endocarditis Common Gram Negative Bacteria • Salmonella typhi – Rod-shaped, found as a single organism – Aerobic, facultative anaerobe – Produces exotoxin – Resistant to freezing – Transmitted through contaminated water and, less frequently, food Common Gram Negative Bacteria • Salmonella enteritidis – Rod-shaped – Aerobic, facultative anaerobe – Found in animals, particularly shellfish, swine, and fowl Common Gram Negative Bacteria • Salmonella enteritidis – Transmitted orally via contaminated milk, turtles, eggs, undercooked chicken, fish, clams, and pork – Causes enteritis that may progress to meningitis, encephalitis, or nephritis Common Gram Negative Bacteria • Bordetella pertussis – Minute, non-motile coccobacillus – Causes whooping cough Common Gram Negative Bacteria • Neisseria meningitides – Coccus found as diplococci – Aerobic – Causes meningococcal meningitis, bacteremia, and pneumonia Common Gram Negative Bacteria • Proteus mirabilis and Proteus vulgaris – Rod-shaped, found as a single organism – Aerobic, facultative anaerobe – Causes chronic urinary tract infections, pneumonia, gastroenteritis, and bacteremia Common Mycobacterium • General characteristics – Acid-fast, gram positive, aerobic rods – Virulent strains found in cords – two chains in side-by-side parallel arrangement Common Mycobacterium • Mycobacterium tuberculosis – Very slow growing; requires three to six weeks for culture – Causes pulmonary tuberculosis, spinal tuberculosis, and miliary tuberculosis – Transmitted through inhalation of droplet nuclei – Causes necrotizing lesion with caseating center Common Mycobacterium • Mycobacterium leprae – Transmission is intimate contact – Causes leprosy Common Mycobacterium • Mycobacterium avium complex (MAC) and Mycobacterium avium intracellulare (MAI) – Non-tuberculous forming mycobacterium – Does not require same level of precautions – Causes chronic pulmonary infections Common Fungi • Characteristics – Primarily work to decompose dead and decaying matter (saprophytes) – Some parasitic types derive food from living plants or animals – May cause pulmonary infection or pneumonia through inhalation – Yeast: single cell forms Common Fungi • Pneumocystis carinii – Normally not pathogenic – Dormant in most individuals – Mode of transmission is inhalation Common Fungi • Pneumocystis Carinii – Common infection in immunosuppressed hosts; common in HIV patients – Causes diffuse panlobular pneumonia with abrupt onset, fever, tachypnea, hypoxia, cyanosis, and possible asphyxia in the acute stage Isolation Procedures Types of PPE Used in Healthcare Settings • Gloves – protect hands • Gowns/aprons – protect skin and/or clothing • Masks and respirators– protect mouth/nose – Respirators – protect respiratory tract from airborne infectious agents • Goggles – protect eyes • Face shields – protect face, mouth, nose, and eyes 59 Isolation Procedures • Handwashing – The single most important act to prevent spread of infection – Wash hands after touching blood, body fluids, secretions, excretions, or contaminated items, even if wearing gloves – Wash hands between patient contacts or between procedures on the same patient Isolation Procedures • Standard precautions – Hand washing – Gloves: clean, non-sterile gloves when touching blood, body fluids, secretions, mucus membranes, and contaminated equipment Isolation Procedures • Standard precautions – Gowns: clean, non-sterile gowns to protect against activities that may generate splashes or spray of blood, body fluids, secretions, or excretions – Mask and eye protection: if danger of splashes or spray Isolation Procedures • Contact precautions – Standard precautions apply – Required in treatment of patients where transmission of pathogens occurs from body-to-body contact – Gloves required – Gowns for direct contact with patient – Private room – Equipment dedicated to only one patient Isolation Procedures • Droplet precautions – Surgical mask when within six feet of patient – Private room – Door may remain open – Standard precautions apply Isolation Procedures • Airborne precautions – N95 mask is required unless isolation is for measles or chicken pox and the caregiver is immune – Negative-pressure room required – Standard precautions apply Isolation Procedures • Reverse Isolation – Protects immunocompromised patients from visitors and healthcare workers – Standard precautions apply – Gowns, gloves, surgical masks required How to Don a Gown Select appropriate type and size Opening is in the back Secure at neck and waist If gown is too small, use two gowns – Gown #1 ties in front – Gown #2 ties in back 67 How to Don a Mask Place over nose, mouth and chin Fit flexible nose piece over nose bridge Secure on head with ties or elastic Adjust to fit 68 How to Don a Particulate Respirator Select a fit tested respirator Place over nose, mouth and chin Fit flexible nose piece over nose bridge Secure on head with elastic Adjust to fit Perform a fit check – – Inhale – respirator should collapse – Exhale – check for leakage around face 69 How to Don Eye and Face Protection Position goggles over eyes and secure to the head using the ear pieces or headband Position face shield over face and secure on brow with headband Adjust to fit comfortably 70 How to Don Gloves Don gloves last Select correct type and size Insert hands into gloves Extend gloves over isolation gown cuffs 71 How to Safely Use PPE Keep gloved hands away from face Avoid touching or adjusting other PPE Remove gloves if they become torn; perform hand hygiene before donning new gloves Limit surfaces and items touched 72 Where to Remove PPE At doorway, before leaving patient room or in anteroom* Remove respirator outside room, after door has been closed* * Ensure that hand hygiene facilities are available at the point needed, e.g., sink or alcohol-based hand rub 73 How to Remove Gloves (1) Grasp outside edge near wrist Peel away from hand, turning glove inside-out Hold in opposite gloved hand 74 How to Remove Gloves (2) Slide ungloved finger under the wrist of the remaining glove Peel off from inside, creating a bag for both gloves Discard 75 Remove Goggles or Face Shield Grasp ear or head pieces with ungloved hands Lift away from face Place in designated receptacle for reprocessing or disposal 76 Removing Isolation Gown Unfasten ties Peel gown away from neck and shoulder Turn contaminated outside toward the inside Fold or roll into a bundle Discard 77 Hand Hygiene Perform hand hygiene immediately after removing PPE. – If hands become visibly contaminated during PPE removal, wash hands before continuing to remove PPE Wash hands with soap and water or use an alcohol-based hand rub * Ensure that hand hygiene facilities are available at the point needed, e.g., sink or alcohol-based hand rub 78 PPE Use in Healthcare Settings: When to Use PPE • Thus far we have discussed the various types of PPE, considered various factors that go into selecting appropriate PPE, and described how to don, use, and remove PPE safely. This last segment of this presentation will discuss WHEN to use which PPE. 79 Standard and Expanded Isolation Precautions • Decisions regarding when and which type of PPE should be worn are determined by CDC recommendations for Standard Precautions and Expanded Isolation Precautions. 80 Standard Precautions Previously called Universal Precautions Assumes blood and body fluid of ANY patient could be infectious Recommends PPE and other infection control practices to prevent transmission in any healthcare setting Decisions about PPE use determined by type of clinical interaction with patient 81 PPE for Standard Precautions (1) Gloves – Use when touching blood, body fluids, secretions, excretions, contaminated items; for touching mucus membranes and nonintact skin Gowns – Use during procedures and patient care activities when contact of clothing/ exposed skin with blood/body fluids, secretions, or excretions is anticipated 82 PPE for Standard Precautions (2) Mask and goggles or a face shield – Use during patient care activities likely to generate splashes or sprays of blood, body fluids, secretions, or excretions 83 What Type of PPE Would You Wear? Giving a bed bath? Suctioning oral secretions? Transporting a patient in a wheel chair? Responding to an emergency where blood is spurting? Drawing blood from a vein? Cleaning an incontinent patient with diarrhea? Irrigating a wound? Taking vital signs? 84 What Type of PPE Would You Wear? Giving a bed bath? Gown, gloves Suctioning oral secretions? Gloves and mask/goggles or a face shield – sometimes gown Transporting a patient in a wheel chair? Generally none required Responding to an emergency where blood is spurting? Drawing blood from a vein? Gloves Cleaning an incontinent patient with diarrhea? Gloves with or without gown Irrigating a wound? Gloves, gown, mask/goggles or a face shield Taking vital signs? – Gloves Gloves, fluid-resistant gown, mask/goggles or a face shield 85 Disinfection and Sterilization Disinfection and Sterilization • Definitions – Cleaning: the removal of all foreign matter such as sputum, blood, dirt, or organic matter that may provide an environment for bacterial growth – Disinfection: a process to eliminate vegetative, pathogenic microorganisms on inanimate objects; differs from sterilization by lack of sporicidal activity – Sterilization: complete destruction or inactivation of all forms of microorganisms Disinfection and Sterilization • Cleaning – Must be done in an area with separate “dirty” and “clean” sections – Equipment to be cleaned must be completely disassembled Disinfection and Sterilization • Cleaning – Soap, detergent, or enzymatic cleaners must be used – If the object, such as electrical equipment, cannot get wet, then the surface of the device should be cleaned with 70% isopropyl alcohol Disinfection • Disinfection describes a process that destroys the vegetative form of all pathogenic organisms on an inanimate object except for spores Disinfection • Alcohol – Ethyl alcohol and isopropyl alcohol used in healthcare setting – Recommended concentration: 70% – Inactivated by protein – Can damage rubber, plastic, and the shellac mounting of instruments with lenses Disinfection • Quaternary ammonium compounds – Surface acting agents containing ammonium ion that leads to lysis of the cell walls – Best with an alkaline pH – Gram positive bacteria are most susceptible – Ineffective against tuberculosis bacilli, spores, viruses, Hepatitis B, and some fungi – Can be stored and reused for up to two weeks if undiluted Disinfection • Acetic acid (vinegar solution) – Inhibits growth of bacteria and fungi – 1.25% solution appears to have sufficient effectiveness (1 part vinegar to three parts water) – Effectiveness reduced when reused – Used extensively in the home care setting by caregivers Disinfection • Phenols (Lysol) – Bactericidal, fungicidal, and tuberculocidal – Retain activity in the presence of organic matter and are active for a significant time after application – Easily absorbed by porous material and may irritate skin through contact Disinfection • Iodophors (iodine solution, betadine) – Bactericidal, virucidal, and tuberculocidal – Can be used on skin – Water soluble, non-staining Sterilization • Glutaraldehydes – Widely used in disinfection/sterilization of non-critical items – All surfaces must be in contact with solution for it to be effective – Generally bactericidal, tuberculocidal, fungicidal, and virucidal when object is in contact with the solution for ten to thirty minutes; sporicidal if immersed for ten hours – Must be rinsed thoroughly after use to avoid skin irritation Sterilization • Sodium hypochlorite (household bleach) – Exposure to 1:50 dilution for ten minutes sufficient to kill vegetative bacteria, bacterial spores, and tuberculosis organisms – CDC recommends 1:10 solution for disinfecting blood spills – Do not allow mixing with any acid solution; toxic fumes result Sterilization • Autoclaving – Use of steam under pressure for a given duration of time – most common settings are 121° C at 15 lb/sq. inch for 15 minutes – Equipment is cleaned and packaged prior to sterilization – Most common, efficient, and easiest sterilization method Sterilization • Autoclaving – Variables for effectiveness • Temperature • Pressure • Concentration of steam • Holding time – minimum time necessary to kill spores at a specific pressure Sterilization • Autoclaving – Heat sensitive indicators demonstrate equipment has been exposed to conditions necessary for sterilization – they do not indicate sterility Before After Sterilization • Ethylene Oxide ((CH2)2O) – Gas at room temperature, but liquefies readily under pressure – Has distinct, almost sweet odor – Causes irritation to tissue, especially mucus membranes – Flammable and explosive Sterilization • Ethylene Oxide ((CH2)2O) – Variables for effectiveness • Gas concentration • Humidity • Temperature • Time of exposure Sterilization • Ethylene Oxide ((CH2)2O) – Packaging material must be permeable to humidity and ETO – Biological indicator necessary to ensure sterilization – Aeration time required – 24 hours in a well ventilated area – Toxicity to humans includes mutagenicity and carcinogenicity EO Burn EO Explosion Respiratory Therapy Equipment • Large volume nebulizers – Most common source of equipment related patient infections – Always use distilled water – When refilling, empty remaining fluid and then refill – Drain tubing away from the patient – Change and sterilize large volume nebulizers every twenty-four hours Depends on facility, once a week Respiratory Therapy Equipment • Small volume nebulizers – Daily between treatments on the same patient, rinse with sterile water, and air dry – Replace every 72 hrs – Use disposable or sterilized units between patients – Use single use medication vials whenever possible Respiratory Therapy Equipment • Ventilator circuits – Infections uncommon due to use of high efficiency particulate air/aerosol filters – Change every 30 days – Sterilize circuits, if non-disposable Respiratory Therapy Equipment • Ventilator circuits – Place bacterial filters proximally to the humidifier – Use sterile water to fill humidifiers – Change heat-moisture exchangers (HMEs) according to manufacturer’s specifications Respiratory Therapy Equipment • Bag-valve-mask devices – Must be sterilized between patients if non disposable, BUT most are disposible – Should be cleaned and exterior disinfected daily when in use with one patient Respiratory Therapy Equipment • Suction systems – Use a fresh, sterile single-use catheter on each patient – Canister and tubing must be changed between patients Respiratory Therapy Equipment • Oxygen therapy equipment – Minimal risk associated with oxygen therapy equipment – If using humidifier, it must be changed between patients Respiratory Therapy Equipment • Pulmonary function equipment – External tubing must be exchanged and sterilized between patients – Inner parts of equipment pose little risk of crosscontamination • Use disposable equipment whenever possible