Integumentary Anatomy
advertisement

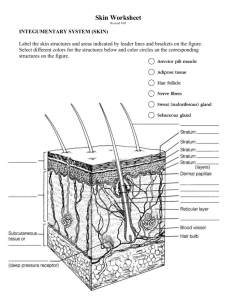
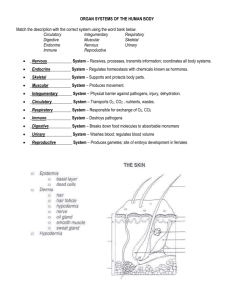
Integumentary Anatomy Laura E. Edsberg, Ph.D. The Skin • Epidermis • Dermis • Subcutaneous Fat Largest Organ System • 1/3 of cardiac output is directed to skin • Surface area 18-20 Sq Ft • 7% of body weight • Thickness 1.5-4mm Functions of The Skin • Large & Complex • Sensory Functions • Barrier – Harmful Chemicals – Ultraviolet Radiation – Infection • Temperature Regulation & Sweating • Required for Vitamin D Production Epidermis • Tough, leathery outer surface • Composed mainly of Keratinocytes • .06-.6mm, thickest portion palms and soles • Epidermis avascular, receives nutrients by diffusion through semi-permeable Basement Membrane (BM) Epidermal Cellular Layers • Five Layers – Represent different stages of cellular differentiation, gradual loss of nuclear material & accumulation of keratin proteins – New cells form – Older cells elongate, membranes thicken as they are pushed up Basal Layer • Stratum Basale, deepest layer, attached to dermis by thin, acellular (BM) • Single row of keratinocytes • Typically, mitotic activity of keratinocytes is confined to this layer • Epidermal turnover time Approx. 4 weeks • Keratinocytes produce Keratin (protective protein) Stratum Spinosum • Above Stratum Basale • Several rows of more mature keratinocytes • Appear spiny due to keratin filaments Stratum Granulosum • Above Stratum Spinosum • Three to five flattened cell rows • Increased concentration of Keratin Stratum Lucidum • Above Stratum Granulosum • As keratinocytes migrate up away from their dermal blood supply, they slowly die • Stratum Lucidum contains layers of flattened dead keratinocytes Stratum Corneum • • • • • “Horney” Layer Consists of dead keratinocytes 20-30 cells thick 75% of thickness of the epidermis Cells are continuously abraded & replaced by cells below • A cells journey from the basale layer up through the corneum takes 14-21 days • Friction or pressure will increase the thickness of the stratum corneum (Callus) Epidermal Cells • Keratinocytes - Keratin (protective protein) • Merkel Cells – Specialized mechanoreceptors (light touch) • Langerhan’s Cells – deeper layers of epidermis assist in fighting infection (attack & engulf foreign material) • Melanocytes Melanocytes • Produce pigment Melanin – Protects skin from UV – Gives the skin its color • More = Darker • Less = Lighter • Grey Hair - loss of melanocytes in hair bulb – Faster turnover in scalp vs body Epidermal Appendages • Specialized epidermal structures, extend down into the dermis - Hair, Glands, and Nails • Hair Follicles (soft keratin) – everywhere except palms and soles – Helps regulate body temp by trapping air between hair and skin surface • Sebaceous Gland – Each hair follicle contains a sebaceous gland – Secretes Sebum – oily substance that lubricates skin & hair – May slow bacterial growth, reducing colonization Epidermal Appendages • Sudoriferous Glands – Present everywhere except lips and ears – Secrete sweat into ducts that lead to skin’s surface – Evaporation of sweat helps cool the body • Nails – dorsal tips of digits – Hard Keratin – Protect terminal digit & assist with function Functions of the Epidermis • Provides a physical & chemical barrier • Regulates fluid • Provides light touch sensation • Assists with thermoregulation • Assists with excretion • Assists with vitamin D production • Contributes to appearance Basement Membrane Zone Dermo-Epidermal Junction • Where epidermis and dermis join • Contains many proteins and structures • Site of inflammation in many diseases • Congenital defects • Important in skin neoplasia Aging and the DermoEpidermal Junction • Flattening with age – Dermal papillae – Epidermal rete pegs • Flattening = Less Surface Area – Less communication – Less resistance to shearing Dermis • 2 to 4mm thick, fibrous part of skin • Contains collagen and elastic fibers contained in an amorphous ground substance, nerve fibers, and nerve-end sensory organs • Highly vascular – Capillaries provide color (pale pink to rosy red) – Superficial Lymphatics • Assist in returning H2O, proteins, and other substances from tissue to blood stream • Dermis should appear shiny or moist due to high H20 content Dermal Layers • Two layers – Papillary Dermis (thin superficial) • Loosely woven fibers embedded in gelatinous matrix (ground substance) • Blisters occur here if friction between epidermis & dermis – Reticular Dermis • Dense irregular arranged connective tissue • Provide increased structural support to the skin Aging and the Dermis • Decreased thickness • More Avascular • Decrease in elastin content Dermal Cell Types • Fibroblasts – main cells found in dermis, produce collagen & elastin fibers, ground substance – Give dermis strength & flexibility • Macrophages & Polymorphonuclear Leukocytes (neutrophils) – Help fight infection by engulfing harmful substances & releasing destructive enzymes Dermal Cell Types • Mast Cells – Specialized secretory cells • Produce chemical mediators of inflammation such as histamine – Attract other cells and cause vasodilation to fight infection or repair injury • Dermis also contains sensory receptors for: – – – – Touch Vibration Temperature Pressure Functions of the Dermis • Support & nourish epidermis • House epidermal appendages • Assists with infection control • Assists with thermoregulation • Provides sensation Subcutaneous Tissue • Hypodermis • Supports the skin • Adipose Tissue – Highly Vascular, loose connective tissue, stores fat for energy, insulation, protection (cushion over structures such as bony prominences) – Healthy adipose is glisteny white to pale yellow (darker if dehydrated) • Fascia – Highly fibrous connective tissue – Separates and surrounds structures, facilitates movement between adjacent structures (muscle, tendon, bone) • Deeper lymphatic vessels are located in subcutaneous tissue Deeper Tissues • Wounds can extend beyond subcutaneous tissue • Muscle – Regularly arranged fibers surrounded by fascia – Rich vascular supply – red in color – bleeds easily – Non-viable muscle will appear gray or black in color • Tendons – Regularly arranged fibers, may be enclosed in fibrous sheath Deeper Tissues • Ligaments & Joint Capsules – – – – – consist of dense connective tissue Ligaments – regularly arranged fibers Joint Capsule – direction of fibers vary When Healthy, glisteny (silky) white appearance Non-viable, dry, leathery, dark, and may be disconnected • Bone – Shiny, smooth, milky white appearance, hard when probed – Unhealthy – moth-eaten, irregular surface, dark discoloration • Pressure ulcers, Diabetic lesions, or burns may involve these deep tissues Depth of Tissue Involvement • Extent of tissue involvement is characterized as: – Superficial – Partial-thickness – Full-thickness Superficial Wounds • Affect only the epidermis – Ex. Abrasion – top layer of integument is removed • Dermis may be exposed Partial-thickness Wounds • Involve epidermis & part of the dermis – Ex. Second degree burn (sunburn), deep with blistering & peeling Full-thickness Wounds • Extends through epidermis & dermis to the subcutaneous tissue layer • May be further categorized as – Subcutaneous – Sub-dermal ** if tissues such as: tendon, muscle, or bone are involved Pressure Ulcer Stages • National Pressure Ulcer Advisory Panel (NPUAP) classification system Stage I: Nonblanchable erythema of intact skin Stage II: Partial-thickness skin loss involving epidermis or dermis or both. The ulcer is superficial and presents clinically as an abrasion, blister, or shallow crater. Pressure Ulcer Stages Stage III: Full-thickness skin loss involving damage or necrosis of subcutaneous tissue, which may extend down to, but not through, underlying fascia. The ulcer presents clinically as a deep crater with or without undermining of adjacent tissue. Stage IV: Full-thickness skin loss with extensive destruction, tissue necrosis or damage to muscle, bone, or supporting structures (e.g., tendon, joint capsule, etc.). Questions ????