Quite simply
advertisement

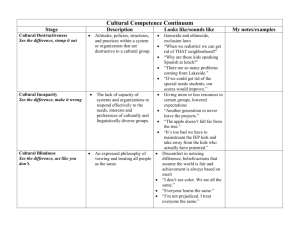
Creating Tomorrow’s Doctors David Taylor That is our task Quite simply, to help our students learn to be the type of Doctor • that we would want them to be • that we would want to treat our parents or children • that we would want to treat us Flexner • It is a hundred years since the first major look at medical education, and internationally there is considerable interest in validation and re-validation. • I serve as a “visitor” for the British General Medical Council, and the equivalent for the Republic of Eire. Regulation Outcomes • We have entered an era where we need to show that we meet measurable outcomes • This is true at undergraduate level but also licensing and re-validation Standards • There is a real debate about what constitutes competence. • What is, in fact, “good enough”? • How do we measure it? • What is a pass mark? • Who says? So much has changed • We know much more than we did • We know more about teaching than we did • Patients expect more than they did • It is not about “doing more” • It is about “doing it cleverer!” I come from Liverpool I am from Liverpool • And we have developed our programme around problem based learning • Obviously we still have lectures But • The route through the syllabus is determined by a series of clinical vignettes, which the students discuss in small PBL groups The Teacher role has developed to include • being able to make small groups work well • Giving students confidence to say what they know • Giving students the responsibility for determining what they still need to know But • We are still expected to know what we are doing • We are still expected to challenge students And • We get to know some of the students very well What do we know? • There have been huge developments in our understanding of education over the past 50 years • There is an unprecedented amount of information available So what are the “big ideas”? Everyone will have their own list, but, looking at the latest editions of my favourite journals: • Delivery methods • Predictors of success • Professionalism Delivery Methods • from “which” to “how best to do it” • emphasised by two AMEE guides. • Taylor and Miflin in 2008 wrote about the benefits and problems with PBL • Edmunds and Brown in 2010 wrote about how best to run small groups. Not only that • Language matters • (Medical Education 44 (8) 2010) • In the way that cases are presented to weaker candidates • In academic performance • In future career performance And • There is an increasing interest in the use of adult learning theories to shape the way that we plan medical programmes. • There is going to be a series of papers published in Medical Teacher on this area. Extrinisic motivation Task Learning style Stage of development planning New learning objective Relevance reflection learner Prior knowledge Organisation intrinsic motivation experience or articulation Feedback Elaboration Refinement Restructuring And • There is a huge literature on whether students should perform dissection (and why/why not)? • What is the role/value of clinical apprenticeships? • What about outcome measures? Predictors of success • Basically, do grades obtained before medical school predict performance at medical school? • It depends how you measure performance! • But as Geoff Norman says“Good students do well”. There is more to this, of course • Do we want to use clinical aptitude tests as a filter? • Multiple mini interviews? • Do we want our students to have a scientific or a more rounded education? • Do we want them to have degree before they enter medical school? Professionalism - (My current interest) • What do we/students/public mean by professionalism? • What constitutes a lapse? • Is there any such thing as a private life? • Is it caught or taught? • Self care What are the components? relationships Qualities Competence Competence Ask for help when necessary Qualities Altruism Relationships Altruism Critical thinking Give patients information they can understand Good clinical judgement Know limits of competence Asks for help Blows whistle Asks for help Blow the whistle Caring Compassion Caring compassionate reflective Technical competence Courage Gives patients information they can understand Good clinical judgement Leadership Professional conduct Knows limits of competence reflective Leadership Respect for others in the team Professional conduct Respect patients right of shared decision making Teamwork Protect confidential information Reflective Respect for colleagues Respects patients rights of shared decision making Submission to ethical code Trustworthy Reliability analysis (Cronbach’s alpha) Protect confidential information Student score Then what? Always Essential Unimportant Never Expectation Self care • There is real interest, and research into the effect of stress upon medical students and trainees • And more importantly on ways of dealing with it (social support, autonomy, “integrated medicine”) What to remember • Medical Education is changing, and changing quickly • It can be overwhelming, but exciting • And there is a lot out there to help • But it is what you do here that matters!