File
advertisement

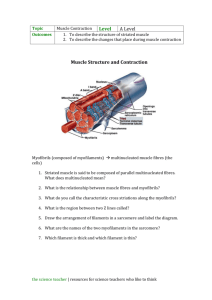
MUSCLE PHYSIOLOGY Myology Muscles – the study of muscles make up 40-50% of body’s mass TYPES OF MUSCLE CONTROL Voluntary – muscles under conscious control of Somatic Division of nervous system Involuntary – muscles you cannot control; under Autonomic Division of nervous system Ex.; arms, legs Ex.; heart, muscles of digestive tract Both – voluntary and involuntary Ex.; breathing, eyelids THREE TYPES OF MUSCLE TISSUE differ in microscopic anatomy, location & control by nervous & endocrine systems 1. skeletal muscle – attached to bone Striated – alternating dark and light bands Primary function - to produce movement Voluntary control (some are involuntary, like the diaphragm and muscles of posture) 2. cardiac muscle – found in the heart Function - to pump blood through the heart and blood vessels Striated Involuntary control Autorhythmicity – built in rhythm of the heart; can be affected by hormones and neurotransmitters (speed up or slow it down) Intercalated disc – thickened areas where one muscle fiber connects to another 3. smooth muscle – also called visceral Found in the walls of internal organs and blood vessels Nonstriated (smooth) Involuntary control Function by contracting and relaxing to move substances through the body (ex.; food through the digestive tract, urine through urinary system) FUNCTIONS OF MUSCLE 1. movement 2. posture - result of sustained muscle contractions 3. heat production - when muscle contracts, it produces heat which is used to maintain normal body temp. 4. moves substances within the body (food, waste, blood) 5. regulates organ volume: sphincters (rings of smooth muscle) that close the outlets of hollow organs CHARACTERISTICS OF SKELETAL MUSCLE 1. excitability – ability to receive & respond to stimuli by producing electrical signals called muscle action potentials Muscles respond to a stimulus from the nervous system Stimuli could be autorhythmic or chemical 2. contractility – the ability to shorten or contract Two types of muscle contraction: A. Isometric contraction –muscle tension is increased, but no movement is produced B. Isotonic contraction – muscle maintains the same tension, movement between two parts 3. extensibility - the ability of a muscle to stretch without being damaged Ex., stomach filling with food 4. elasticity – the ability of muscle to return to its original length and shape after contraction STRUCTURE OF SKELETAL MUSCLE STRUCTURE OF SKELETAL MUSCLE Each muscle is a separate organ containing - muscle cells called fibers - connective tissue called fascia - blood vessels - nerves musclefasciclefibermyofibrilfilament Fascia – sheet of fibrous connective tissue that surrounds and protects muscles Superficial fascia – separates muscle from skin -stores adipose (fat) tissue, which stores triglycerides & provides insulation to guard against heat loss Deep fascia – dense (three layers), irregular connective tissue that holds muscle with similar function together -contains nerves, blood vessels, lymphatic vessels - allows free movement of muscles - protects & strengthens muscle THREE LAYERS OF DEEP FASCIA 1. Epimysium - outermost layer of connective tissue that covers the entire muscle 2. Perimysium – connective tissue that surrounds groups of 10-100 or more muscle fibers These fibers grouped into bundles are called fascicles 3. Endomysium – innermost layer of connective tissue around each muscle fiber All three of these combine to form Tendons – connective tissue cords that attach muscle to periosteum of bone MUSCLE FIBERS Muscle fibers arise from myoblasts (stem cells) that fuse during embryonic development Once fusion has occurred, fibers cannot undergo cell division…so we are born with a set number of fibers A few myoblasts remain as satellite cells, which fuse with other fibers to repair damaged fibers A typical muscle fiber is ~ 100mm in length STRUCTURE OF MUSCLE FIBERS Covered in sarcolemma – cell membrane Contains multiple nuclei (fused myoblasts) Contains sarcoplasm – cytoplasm contains glycogen, which can be split into glucose that’s used in ATP synthesis Contains myoglobin, which is the oxygen binding protein needed for ATP production in mitochondria Fibers divide into myofibrils MYOFIBRILS - contractile unit of skeletal muscle - extend entire length of muscle fiber - make muscles fiber look striated - can increase or decrease in number sarcoplasmic reticulum –encircles each myofibril - in relaxed muscle fibers, it stores calcium - release of calcium triggers muscle contraction T-tubules - connect myofibrils to sarcolemma - receive nerve impulses - allows action potential to quickly spread thoughout the fiber MUSCLE PROTEINS Myofibrils - built from 3 different types of proteins 1. contractile proteins – generate force during contraction Actin – thin filaments Myosin – thick filaments; converts chemical energy of ATP into mechanical energy of motion 2. regulatory proteins - turn contraction on and off Troponin Tropomyosin 3. structural proteins - give myofibril extensibility and elasticity Myofibrils divide into filaments FILAMENTS Filaments - arranged in sarcomeres Sarcomere -structural unit of myofibril Thick filaments – contain myosin Thin filaments – contain actin -thick and thin filaments overlap each other, which shows up as striations Z discs – separates one sarcomere from the next M line - middle of sarcomere A Band – dark middle part of sarcomere made up of thick filaments (myosin) and part of thin (actin) I band – lighter area made up of thin filament only (actin) THICK FILAMENT Myosin – acts as a motor protein (push or pulls what’s attached to it to achieve movement ~300 molecules of myosin make up a single thick filament THIN FILAMENT Actin – individual actin molecules join to form an actin filament that’s twisted into a helix Contain myosin-binding sites – where myosin heads can attach Tropomyosin – covers the myosin binding sites on actin in relaxed muscles Troponin – holds tropomyosin in place MUSCLE CONTRACTION Sliding Filament Mechanism thick and thin filaments slide past each other during contraction, shortening the muscle - when contraction occurs, myosin binds to actin, pulling it towards the M line - Sarcomere shortens – thick and thin DO NOT shorten…they slide past each other to overlap - Sarcomere shortens, fiber shortens, muscle shortens (contracts) STEPS IN MUSCLE CONTRACTION 1. stimulus received from nervous system 2. action potential spreads through Ttubules 3. sarcoplasmic reticulum releases calcium 4. calcium causes troponin to change shape 5. troponin pulls on tropomyosin uncovering myosin binding site on actin 6. myosin attaches to actin and pulls on it 7. thick and thin filaments slide past each other 8. when action potential stops, calcium is pumped back into the sarcoplasmic reticulum High calcium levels in sarcoplasm starts contraction Low calcium levels in sarcoplasm ends contraction *****ATP POWERS THE ENTIRE PROCESS***** CLINICAL APPLICATION- RIGOR MORTIS After death, calcium leaks out of sarcoplasmic reticulum Myosin binds to actin No ATP synthesis so muscles stay contracted Begins ~3-4 hours after death, peaks at 12 hours and stops at 24 hours when tissues begin to breakdown NERVE AND BLOOD SUPPLY WITHIN MUSCLES Motor neurons - nerves that stimulate muscles to contract -requires a lot of energy (ATP) & produces lots of waste…so there are lots of capillaries in the endomysium Motor unit – a motor neuron and the skeletal muscles it stimulates Synapse – meeting place where a muscle and a nerve communicate with each other Synaptic cleft – a small gap that exists between the neuron and the muscle fiber at the synapsis Neurotransmitter – a chemical that allows nerves and muscles to communicate across that gap Acetylcholine (ACH) – the neurotransmitter for skeletal muscle contraction NEUROMUSCULAR JUNCTION Neuromuscular junction – a synapse between a motor neuron and a skeletal muscle Each motor neuron has an axon that divides into several axon terminals At the end of each axon terminal are little sacs called synaptic vessicles that contain acetylcholine The motor end plate is the region of sarcolemma adjacent to the synaptic vessicles. It contains acetylcholine receptors (30-40 million receptors/end plate) When acetylcholine binds to the receptor on the muscle, it causes sodium (Na+) to go into the muscle cell…contraction occurs Acetylcholinesterase – enzyme that breaks down acetylcholine with no acetylcholine, the action potential is ended.