Urinary System - El Camino College
advertisement

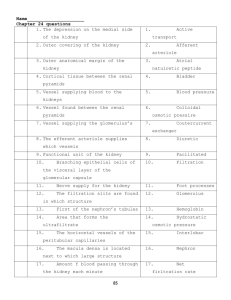
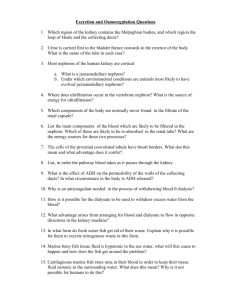
Urinary System Human Anatomy Chapter 23 • I. Kidneys • The kidneys perform the following functions: excretion of urea (from amino acid breakdown), uric acid (nucleic acid turnover), and creatine (from creatine phosphate breakdown). It also disposes of waste and excess ions, it regulates blood volume and its chemical make up, it affects blood pressure and red blood cell formation (erythropoetin- hormone to stimulate blood production). People can survive with just one kidney. • • A. Gross anatomy • 1. Location and external anatomy - The kidneys appear to be bean shape, both the left and right kidney lie against the posterior abdominal wall above the ilium and are protected by the lower two ribs. The renal hilus is the location where blood vessels and nerves enter the kidney. Superior to each kidney is the adrenal gland. •The kidneys are surrounded by the renal capsule (dense connective tissue), the adipose capsule (contains perirenal fat), and the most external membrane is renal fascia. There is some fat that lies close to the kidneys called pararenal fat, both fat layers cushion and support the kidneys. • 2. Internal gross anatomy- The following features can be seen with the naked eye in dissection. The most superficial region is the renal cortex which is lighter in color than the deeper region called the renal medulla. The renal medulla is divided into sections called renal pyramids, the renal columns (extensions of the cortex) lie in between the renal pyramids. The minor calices collect urine and merge into major calices which are branches that converge to form the renal pelvis (superior part of the ureter). The renal pelvis joins the ureter. Microscopic View of Renal Cortex (Shows nephron) Microscopic view of Renal Medulla • 3. Gross vasculature and nerve supply- The kidneys have a rich blood supply (see figure 23.3, 23.9, 23.10 for summary). The largest blood vessels are the renal arteries and veins. They eventually become segmental arteries, then lobar, then interlobar. They narrow more and become arcuate, they are called interlobular ateries again and finally reach the nephron as affarent and efferent arterioles. They then wrap around the nephron as pritubular capillaries and vasa recta. As this point they are veins and have the same names as the ateries: interlobular, arcuate, and renal vein. The renal plexus serves the nerves supply of the kidney carrying autonomic NS fibers. The sympathetic fibers control the diameters of the kidney arteries and influence uriniferous tubules. •3. Gross vasculature and nerve supply- The kidneys have a rich blood supply (see figure 23.9 for summary). The largest blood vessels are the renal arteries and veins. They eventually become segmental arteries, then lobar, then interlobar. They narrow more and become arcuate, they are called interlobular ateries again and finally reach teh nephron as affarent adn efferent arterioles. They then wrap aroudn the nephron as pritubular capillaries and vasa recta. As this point they are veins and have the amse as teh ateries: interlobular, arcuate, and renal vein. The renal plexus serves the nerves supply of the kidney carrying autonomic NS fibers. The sympathetic fibers control the diameters of the kidney arteries and influence uriniferous tubules. • • • B. Microscopic anatomy of the kidneys-This section examines the uriniferous tubules composed of the nephron and the collecting tubule. We will also look at urine production. 1. Mechanisms of urine productionurine production has three stages: • a. Filtration- blood filtrate enters the nephron, it resembles blood plasma and it is further processed to create urine. Note that normally NO blood cells or large proteins enter as part of filtrate. • b. Reabsorption- along the nephron beneficial molecules such as nutrients, water, and essential ions are reclaimed. These are returned into the blood. • c. Secretion- Undesired molecules are actively removed and passed along the tubules of the nephron on their way to become urine. • 2. The nephron- the filtering unit of the kidney contain various sections that perform different functions. • a. Nephron types- cortical nephrons are the most abundant type. Most of the nephron is located within the cortex and only a small portion of the loop of Henle enters into the medulla. About 15% of the nephrons are juxtamedullary nephrons because the Loop of Henle extends well into the renal medulla, these are used to produce highly concentrated urine. • b. Renal corpuscle- this is the site of filtration. The network of capillaries at this site is the glomerulus, it has afferent and efferent capillaries (no venuoles). These are surrounded by the glomerular capsule (Bowman’s capsule). The cells of the glomerular capsule are called podocytes. This site has fenestrations on the capillaries and filtration slits within podocytes, making it highly permeable. c. Tubular section-connecting to the renal corpuscle are the tubules responsible for reabsorption and secretion. First is the proximal convoluted tubule (cortical nephron) it is surrounded by peritubular capillaries. The proximal convoluted tubule goes into a long loop called the Loop of Henle. There is a descending and ascending limb. The ascending limb connects to the distal convoluted tubule which connects to the collecting tubules. Blood vessels in the Loop of Henle are called vasa recta, they are involved in concentrating urine. • 3. Collecting tubulesthese collect urine from several nephrons and run into the medulla where they merge with other collecting tubules to form papillary ducts that empty into minor calyces. When the body dehydrates the collecting tubules become more permeable and allow water to be reabsorbed, reducing urine volume and increasing its concentration. • . • 4. Juxtaglomerular apparatus- a structure that regulates blood pressure by releasing a hormone called rennin as a response to falling blood pressure. This causes an increase in blood solute concentration which leads to an increase blood volume and thus increased blood pressure. • 5. Interstitial connective tissue- layers of connective tissue that surround the uriniferous tubules and contain cells that release hormones to influence blood pressure and red blood cell production II. Ureters – Tubules that carry urine from the kidney to the bladder. A. Gross Anatomyabout 10 inches long, runs from the renal pelvis and reaches the bladder medially on its posterior wall. It enters at an oblique angle to prevent back flow. Forma two points of the trigone. B. Microscopic anatomy- this tube has three layers: mucosa, muscularis, and adventitia. Urine reaches the bladder through peristalsis. The muscle contractions seem to be guided by a reflex response. III. Urinary bladdera muscular sac that stores urine. It can collapse when empty and expand enough to enter into the abdominal cavity. In males it lies anterior to the rectum and in females it lies anterior to the uterus and vagina. It also has three layers: the mucosa, muscularis, and adventitia IV. Urethra- a thin tube that drains the urine out of the body from the bladder. It is short in females and long in males. In females the opening of the urethra lies posterior to the clitoris and anterior to the anus. The male urethra opens at the tip of the penis and carries both urine and semen. An involuntary sphincter muscle keeps the urethra closed when there is no urine, a voluntary sphincter constricts urine flow until the appropriate time to void. V. Micturition- Urination or voiding occurs when pressure in the bladder is increased either by bladder muscle and/or abdominal muscle contraction. This action is controlled by the brain, the parasympathetic neurons stimulate contraction of the muscle to induce voiding and the sympathetic branch stimulates the sphincter to prevent micturition. VI. Disorders of the urinary system • A. Urinary tract infections- these are more common in women than in men. In women they most often result from intercourse because it brings bacteria into the urethra and spermacides kill the natural living bacteria in the vagina. In men it can arise from long-term catheterization. The infection can spread from the bladder up the ureters and to the kidneys. The symptoms include frequent micturition accompanied by a burning sensation and fever. These infections are treated with antibiotics. • B. Renal Calculi- commonly known as kidney stones, they form when calcium, magnesium, or uric acid salt precipitate and accumulate. They cause pain when they obstruct a ureter. Kidney stones are caused by different factors but one of them is dehydration. Treatment includes ultrasonic shock wave therapy. • C. Cancer of Urinary Organs • 1. Bladder cancer- five times more common in men than in women, the cancer arises from the transitional epithelial cells of the mucosa. It can arise from exposure to tar in tobacco smoke, chemicals, and artificial sweetners. Blood in urine is a sign of bladder cancer. • 2. Kidney cancer- arises from epithelial cells of the uriniferous tubules or renal pelvis. It is more common in men than in women. Risk factors include obesity, high blood pressure, and a high protein diet. By the time it is detected the tumor has metastasized and since it is resistant to cancer treatment, the person only has months to live.