The Menstrual Cycle & Pregnancy
advertisement

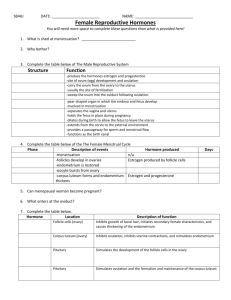
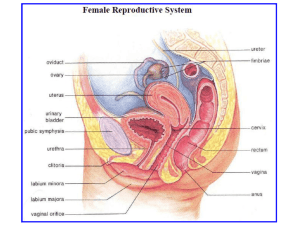
The Menstrual Cycle & Pregnancy HONORS ANATOMY & PHYSIOLOGY THE REPRODUCTIVE SYSTEM PART 3 Female Reproductive Cycle 2 parts: Ovarian Cycle 1. 1. series of events in ovaries occurring during & after maturation of oocyte 2. Uterine (Endometrial) Cycle 1. 2. concurrent with ovarian cycle series of changes in endometrium to repare it for implantation of fertilized egg Hormonal Regulation Hypothalamus secretes GnRH (gonadotropin- releasing hormone) that controls both the ovarian & uterine cycles GnRH stimulates release of FSH & LH from anterior pituitary Effects on Ovaries FSH initiates follicle growth stimulates: follicles to release E granulosa cells to turn androgens E LH stimulates : further development of follicles release of E from follicles release of androgens from theca cells @ midcycle LH surge triggers ovulation corpus luteum E, P, relaxin, inhibin Estrogens 3 of 6 different estrogens are present in significant amts: 1. ß estradiol 2. Estrone 3. Estrial most abundant in non-pregnant female made from cholesterol in ovaries Functions of Estrogens promote development &maintenance of female reproductive structures, 2◦ sex characteristics 2. increase protein anabolism working synergistically with hGH 3. lowers cholesterol (1 reason females <50 yo have lower risk of CAD) 4. moderate levels inhibit release of GnRH, FSH, LH (negative feedback loop) 1. Progesterone secreted by corpus luteum with E prepares endometrium for implantation & breasts for lactation Relaxin produced by corpus luteum inhibits contractions of myometrium during pregnancy, placenta secretes more relaxin…@ end of pregnancy it increases flexibility of pubic symphysis & may help dilate cx Inhibin secreted by granulosa cells of growing follicles & by corpus luteum after ovulation action: inhibits secretion of FSH & to lesser extent LH Hormones of the Menstrual Cycle Phases of the Menstrual Cycle Menstrual Phase 2. Preovulatory Phase 1. in ovaries called follicular phase in uterus: proliferative phase 3. Ovulation 4. Postovulatory Phase in ovaries called luteal phase in uterus: secretory phase Menstrual Phase aka menstruation, menses ~1st 5 d of cycle (d 1 of flow = day 1 of cycle) Ovaries: FSH causes several primordial follicles to develop 1◦ follicles 2◦ follicles Uterus: declining E & P levels prostaglandins constriction of uterine spiral arterioles O deprived tissue death & shedding 50 – 150 mL of blood, tissue fluid, mucus, epithelial cells (entire stratum functionalis sloughs off) Preovulatory Phase time between end of menses ovulation most variable length in time (reason cycles vary in length) Ovaries: follicles secrete E & inhibin d 16 one 2◦ follicle in 1 of the 2 ovaries becomes the dominant follicle (secretes more E & inhibin decreases FSH) dominant follicle (Graafian) enlarges until ovulation:~2cm Preovulatory Phase (Proliferative) Uterus: E stimulates repair of endometrium producing new stratum functionalis new endometrial glands form endometrium thickens from ~4 to 10 mm Ovulation d 14 in 28 d cycle 2◦ oocyte surrounded by zona pellucida & corona radiata higher levels of E @ end of preovulatory phase have + effect on cells that secrete LH & GnRH: their increase leads to ovulation OTC test for LH surge used to predict ovulation Mittleschmerz pain noted @ time of ovulation caused by small amt of blood that leaks into pelvic cavity from ruptured follicle Postovulatory Phase (Luteal) time between ovulation & onset of next menses Most constant part of cycle = 14 days (d15 – 28) Ovary: under influence of LH, granulosa cells transformed corpus luteum cellswhich secrete E, P, relaxin, inhibin if oocyte not fertilized: corpus luteum lasts 2 wks corpus albicans + fertilization: corpus luteum persists until “rescued” by hCG (human chorionic gonadotropin) which is made by chorion of embryo @ ~ 8d after fertilization Postovulatory Phase (Secretory) Uterus: P & E made by corpus luteum promote: growth & coiling of endometrial glands vascularization of superficial endometrium thickening of endometrium (12 – 18 mm) these changes peak 1 wk after ovulation if no fertilization levels of P & E decline which eventually causes menstruation Homeostatic Imbalances Dysmenorrhea painful menses Amenorrhea absence of menses #1 reason = pregnancy Endometriosis disorder in which endometrium grows outside uterus +/- painful can cause infertility due to scarring Embryonic Period Fertilization: Nuclei from sperm merges with nuclei from 2◦ oocyte forming a diploid nucleus Fallopian tube normal site of fertilization w/in 12 -24 hrs after ovulation sperm can remain viable up to 48 hrs after deposition in vagina Fertilization sperm must penetrate 2 layers: corona radiata 1. granulosa cells that surround 2◦ oocyte 2. zona pellucida clear glycoprotein layer between corona radiata & oocyte’s plasma membrane Fertilization ZP3: 1 of glycoproteins acts as sperm receptor acrosomal reaction: occurs when ZP3 binds to specific membrane protein on sperm head plasma membrane release of contents of acrosome Acrosomal Reaction acrosomal enzymes digest a path thru zona pellucida lashing flagella of sperm pushes it forward several sperm bind to ZP3 molecules but only 1st sperm to penetrate zona pellucida & reach plasma membrane of oocyte “wins” once diploid nucleus formed its called a zygote Cleavage of the Zygote rapid M phase but no growth 1st division begins ~24 hrs after fertilization taking 6 hrs to complete, following divisions take less time ~2 d after fertilization = 4 cells ~ 3 d after = 16 cells cells get progressively smaller, & are called blastomeres morula (mulberry) solid sphere of cells, still surrounded by zona pellucida & still about size of original zygote Blastocyst Formation ~ end of 4th d: # of cells in morula increase as it is still moving thru fallopian tube enter uterine cavity on d 4-5 glycoprotein secretions fromendometrial glands enter morula providing nourishment @ ~ 32 cell size, fluid enters morula & collects between blastomeres forming fluid-filled cavity = blastocyst cavity (up to ~100 cells) & now called a blastocyst or blastula (still ~ same size as original zygote) Blastocyst Forms Layers 2 distinct structures form: Inner cell mass 1. eventually becomes embryo 2. Trophoblast ultimately forms fetal portion of placenta 5th d: blastocyst digests hole thru zona pellucida & squeezes out Implantation attachment of blastocyst to endometrium after implantation endometrium becomes modified & is called decidua Trophoblast develops into 2 layers (both part of chorion): Syncytiotrophoblast 2. Cytotrophoblast 1. hCG is Produced hCG: human chorionic gonadotropin Produced by trophoblast starting on d 6 hCG causes endometrium to grow & proliferate hCGprevents the menstrual cycle from occuring reason female misses her menses when she is pregnant Inner Cell Mass differentiates into a bilaminar disc Hypoblast 2. Epiblast 1. Amnion thin protective membrane develops from cytotrophoblast Gastrulation @ end of cleavage stage, cells making up the blastula move surface proteins help cells recognize each other & help sort cells 3 layers of gastrula formed: called the 3 germ layers Endoderm Mesoderm Ectoderm Extraembryonic Membranes develop from the germ layers but are NOT part of the embryo (lost at birth) lie outside embryo & provide protection & nourishment 4 components: 1. chorion 2. amnion 3. allantois 4. yolk sac Placentation formation of the placenta site of exchange of nutrients & wastes between the mother & fetus also functions as protective barrier & produces several hormones to maintain pregnancy (hCG) Week 2 implantation continues until complete emersion into endometrium Weeks 3 - 4 development of nervous system & cardiovascular system evident Weeks 5 - 8 embryo will develop all structure that an adult has by end of week 8 Embryo/ Fetus Embryonic Period Fetal Period 1st thru 8th wk begins @ 9th wk & goes characterized by until birth @ 38 wks (from fertilization) characterized by growth & development of structures formed in embryonic period development of structures (organs) Maternal Changes in Pregnancy uterus nearly fills abdominal cavity GI tract compressed may cause heartburn, constipation pressure on bladder causes frequency & urgency compression of inferior vena cava may cause varicose veins, &/or edema in legs compression on renal vessels may cause elevated BP (renal hypertension) Maternal Hormone Changes During Pregnancy pregnancy maintained by hCG, E, & P relaxin increases flexibility of pubic symphysis hCS (human chorionic somatomammotropin) contributes to: breast development protein anabolism catabolism of glucose & fatty acids Labor process by which fetus is expelled from uterus true labor involves dilation & thinning of cx false labor may have painful contractions but there are no cervical changes Positive Feedback Loop Adjustments Infant Makes at Birth Infant’s respiratory & cardiovascular systems undergo changes to enable them to become selfsupporting Maternal Breast Changes hormonal changes, increased blood flow, & changes in breast tissue cause breast to feel heavy, swollen, or sore breast tenderness commonly starts w/in 4 wks areolas enlarge & darken Colostrum the yellowish1st milk your baby gets may leak out any time after 3rd mo contains Ig A antibodies, protein, fatsoluble vitamins, minerals replaced by milk after 2 – 4 days baby nursing Breastfeeding is Best Lactation Hormones Prolactin made in anterior pituitary release controlled by dopamine action: activates mammary glands to make milk several minutes of baby nursing stimulates release Oxytocin made in hypothalamus & stored in posterior pituitary baby nursing stimulates its release action: milk let down