25. Reproduction II - campus
advertisement
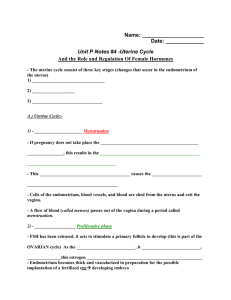
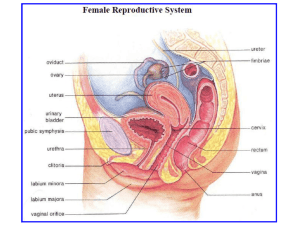
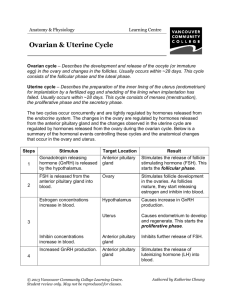
D’YOUVILLE COLLEGE BIOLOGY 108/508 - HUMAN ANATOMY & PHYSIOLOGY II LECTURE # 25 REPRODUCTIVE SYSTEM FEMALE 1. Anatomy of Female Reproductive Tract (fig. 27 - 10): a. Ovaries (fig. 27 - 11): primary sex organs in pelvis; produce ova; secrete sex hormones • primordial germ cells form follicles (primary oocyte + granulosa cells) • granulosa cells nourish ovum & produce estrogens, progestins b. Uterus (fig. 27 - 12): • body, fundus, cervix, wall: perimetrium, myometrium, endometrium (fig. 27 - 13) c. Uterine Tubes: terminate near ovaries with fimbriae; ciliated lining d. Vagina (Birth Canal): inferior to uterus, lined with mucosa • vaginal orifice may be partially closed by the hymen in virgins e. Vulva: labia majora and labia minora enclose vestibule containing clitoris (homologue of penis), opening of urethra and vaginal orifice; fleshy pad of fat (mons pubis) located in front of vestibule at anterior ends of labia (fig. 27 - 14) 2. Mammary Glands (fig. 27 - 15): • modified sweat glands serving to produce milk to nourish newborn • glandular units (alveoli) empty into lactiferous ducts that communicate with openings in the external nipple (surrounded by areola) 3. Physiology of Female Reproduction: a. Hormonal Relationships (figs. 27 - 19 & 27 - 20): • Gonadotropin Releasing Hormones: regulate pituitary gonadotropins: • Follicle Stimulating Hormone (FSH): for follicle growth in ovary • Luteinizing Hormone (LH): for follicle maturation, estrogen secretion • LH surge (near mid cycle) causes ovulation; LH stimulates follicular residue to form corpus luteum which secretes progesterone and some estrogens; LH maintains corpus luteum • Estrogens: proliferation of mammary glands and glands of endometrium; enlargement of pelvic dimensions, development of secondary sex characteristics (female distribution of body fat, rapid but shortened growth in early puberty, development of pubic and axillary hair) • Progesterone: promotes secretion by mammary gland & endometrium b. Ovarian Cycle (figs. 27 - 17 & 27 - 18): i. Follicular Phase (Preovulatory Phase): (approx. first 14 days) follicles enlarge, become vesicular with primary oocyte completing first meiosis ---> mature (Graafian) follicle (ready for ovulation); mostly directed by FSH from anterior pituitary with help of LH Bio 108/508 lec. 25 - p. 2 ii. Luteal Phase (Post ovulatory Phase): LH surge triggers ovulation and development of corpus luteum; progesterone level rises and produces a progressively strengthening negative feedback on anterior pituitary inhibiting further output of gonadotropins Bio 108/508 lec. 25 - p. 3 c. Uterine Cycle (fig. 27 - 20): i. Proliferative Phase: estrogens promote thickening of endometrium (rich blood supply, extensive glandular development) ii. Secretory Phase: progesterone from corpus luteum promotes glandular secretion, preparation of endometrium for implantation iii. Menstrual Phase: in absence of implantation, negative feedback on anterior pituitary causes deterioration of ovarian corpus luteum and resulting decline in progesterone leads to sloughing off of endometrium constituting the menstrual discharge (4 - 5 days) d. Regulation of Non-pregnant Reproductive Cycle: • following menses, pituitary FSH and LH rise, initiating next follicular phase of ovary • estrogens from maturing follicles promote proliferative phase of uterine endometrium • rising estrogen levels cause positive feedback upon anterior pituitary causing gonadotropin surges (especially LH); ovulation ensues • corpus luteum formation in ovary marks beginning of luteal phase with progesterone dominating hormonal picture • progesterone promotes secretory phase of uterine endometrium and negative feedback inhibition of AP gonadotropins • corpus luteum regresses (lack of LH support); endometrium deteriorates with lack of progesterone support; menses begins