Motor systems(W).
advertisement

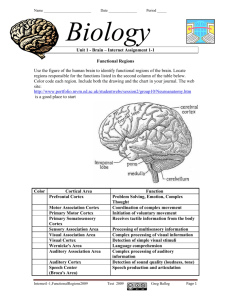
Introduction to Biological Psychology Central Control of Movement Classification of movement 1 – Simple reflex - stretch reflex, knee jerk - mediated at the level of the spinal cord 2 – Posture and postural change - standing, balancing 3 – Locomotion - walking, running 4 – Sensory orientation - head turning, eye fixation 5 – Species specific action patterns - ingestion, courtship, escape/defence, grooming, gestures 6 – Acquired skills - speech dressing, painting, driving, sports, etc Control of movement Motor output comes from the motor cortex Projects through pyramidal tracts to spinal cord, where it synapses with peripheral motor neurones Other pathways run parallel from cortex, basal ganglia and cerebellum via brainstem and spinal cord - these run outside the pyramidal tract and are called the extrapyramidal system Motor control systems in the cortex Primary motor cortex – source of pyramidal tract neurones Supplementary motor cortex - conception and initiation of movement. - lesions cause deficits in voluntary movement or speech Premotor cortex - important in motor coordination. - lesions cause impairments in stability of stance, gait and hand coordination From: Biopsychology, JPJ Pinel Primary motor cortex From: Biopsychology, JPJ Pinel Motor control systems outside the cortex Cerebellum -controls neural ‘programs’ for the executionl of skilled movements Basal ganglia - a group of subcortical forebrain nuclei (caudate nucleus, putamen (= striatum), globus palludus, subthalamic nucleus) - modulate patterns of motor activity Organisation of the motor system Visual cortex Cerebellum Somatosensory cortex Prefrontal cortex Supplementary motor cortex Premotor cortex Motor nuclei of the thalamus Basal ganglia Brainstem Extrapyramidal Motor pathways Primary motor cortex Pyramidal tract Spinal motor pathways Pyramidal tract - control most of our fine movements Tectospinal tract - coordinating head and eye movements as part of the optic reflexes Vestibulospinal tract - influences postural muscles Reticulospinal tract - projects from the reticular formation - inhibition or facilitation of movement From : The Central Nervous System, P. Brodal Spinal reflexes • Mediated at the level of the spinal cord • Do not require any cortical input e.g. Knee jerk reflex • Tapping the knee tendon stimulated tendon stretch receptors • Sensory neurone synapses directly to motor neurone • Muscle contracts to cause limb extension From: Biopsychology, JPJ Pinel Neurological diseases of the motor system Dysfunctions of the Motor System • Paralysis • Apraxia • Decomposition of movement • Parkinson’s disease • Huntington’s disease • Duchenne’s muscular dystrophy • Myesthenia gravis Diseases of peripheral rather than central origin: more information is available on the web slides Paralysis Damage to motor neurones • viral (e.g. poliomyelinitis – leads to destruction of spinal motorneurones) • toxins and/or hereditary (e.g. amyotrophic lateral sclerosis – degeneration of motoneurones in the brainstem and spinal cord) • injury • severing of spinal cord – permanent • bruising or compression of spinal cord – transient Damage to primary motor cortex • paralysis or partial paralysis of voluntary movement on one side of the body (contralateral to damage) • extent of paralysis depends on extent of damage • often accompanied by spasticity and abnormal reflexes Apraxia Inability to carry out movements in response to commands • no paralysis • no loss of comprehension • no loss of motivation May be due to disconnection of primary motor cortex from supplementary motor areas and motor association cortex From: Biopsychology, JPJ Pinel Decomposition of movement Inability to perform “motor patterns” (e.g. walking) • motor patterns are broken up into individual segments instead of being executed smoothly • movements require thought for execution, rather than being “automatic” Due to cerebellar damage Influence of the cerebellum Visual cortex Cerebellum Somatosensory cortex Prefrontal cortex Supplementary motor cortex Premotor cortex Motor nuclei of the thalamus Basal ganglia Brainstem Extrapyramidal tract Primary motor cortex Pyramidal tract Symptoms of Parkinson’s Disease • Resting tremor in limbs – disappears on movement or during sleep • Muscle rigidity – resistance to passive movement: jerky (cogwheel) movement • Akinesia – general paucity of involuntary movement • Stooped posture • Shuffling gait • Excessive sweating and salivation • Micrographia • Altered cognitive function, depression and/or dementia • Deficits in movement controlled by extra-pyramidal motor pathways Neuropathology of Parkinson’s disease • nigro-striatal pathway degeneration • leading to a depletion of striatal dopamine • some degeneration of other dopamine pathways too Dopamine Glutamate X Striatum GABA Treatment of Parkinson’s disease • prior to 1960s there were no effective treatments • realisation of dopamine’s involvement led to use of drugs which increase brain dopamine • dopamine itself cannot cross from the blood to the brain • use precursor, L-DOPA, which enters the brain and is converted there into dopamine • can cause severe side effects (dyskinetic movements, psychotisism) • surgical interventions and neural transplantation are under investigation as alternative therapies Huntington’s disease • Progressive disease causing involuntary muscle jerks • Ultimately affect the whole body • Also intellectual deterioration, depression and occasionally psychotisism • Onset of symptoms usually at 30 to 45 years • Genetically determined (single dominant gene) • Causes degeneration of the output neurones from the striatum, reducing inhibitory modulation of motor function Dopamine Glutamate Striatum X GABA Treatment of Huntington’s disease • no effective treatment • GABA replacement or dopamine antagonists provide some relief • no means of halting the progression of the disease Influence of the basal ganglia Visual cortex Cerebellum Somatosensory cortex Prefrontal cortex Supplementary motor cortex Premotor cortex Motor nuclei of the thalamus Basal ganglia Brainstem Extrapyramidal tract Primary motor cortex Pyramidal tract Additional slides • Muscular dystrophy • Myesthenia gravis Muscular dystrophy A group of diseases characterised by a generalised wasting of muscles Appears to involve biochemical abnormalities leading to structural changes in muscle cells Duchenne’s muscular dystrophy • wasting of muscles caused by a single gene on the x-chromasome (effects only males) • the gene is responsible for the protein product, dystrophin, which may be involved in regulating intracellular calcium • onset of symptoms around 6years old, with death resulting within about 10 years • may respond to gene therapy X-Linkage in Duchenne’s muscular dystrophy • The gene responsible is recessive • Therefore for a female to be affected they would have to have two copies of the DMD gene, one derived from each parent • If a female has one DMD gene (i.e. heterozygous) she would be a carrier, but would not express the disease • For a male to be affected they only need one copy of the DMD gene, which must come from his mother • Since affected individuals die before reaching reproductive age, it is impossible for a male to pass on the DMD gene • Therefore it is impossible for a female to be homozygous for the DMD gene • Therefore a female cannot express the disease. Myesthenia gravis • profound weakening of sketetal muscles • due to reduced numbers of acetylcholine receptors at the neuromuscular junction (c.f. snake venom toxins such as bungarotoxin) • this leads to reduced transmission of neuronal signals activating muscles • caused by autoimmune destruction of the neuromuscular junction • removal of the thymus gland (where immune cells are made) has some beneficial effects