File
advertisement

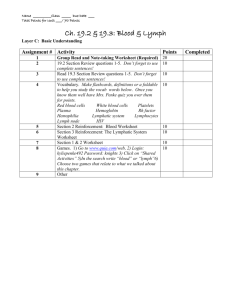
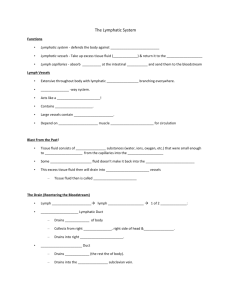
Semester 1 Final Exam St Guide KEY Chapter 14: Blood I. Blood and Blood Cells A. Introduction 2. Most blood cells form in red bone marrow. 3. Types of blood cells are red blood cells and white blood cells. 4. Cellular fragments of blood are platelets. 5. Formed elements of blood are the cells and platelets. B. Blood Volume and Composition B. Blood Volume and Composition 3. An average-size adult has 5 liters of blood. 4. Hematocrit is the percentage of blood cells in a blood sample. 5. A blood sample is usually 45 % cells and 55 % plasma. D. Characteristics of Red Blood Cells 1. Red blood cells are also called erythrocytes. 2. Red blood cells are biconcave in shape. 3. The biconcave shape of red blood cells allow them to have an increased surface area for the transport of gases. 4. Hemoglobin is an oxygen carrying protein in red blood cells. 6. Oxyhemoblobin is hemoglobin combined with oxygen. F. Red Blood Cell Production and Its Control 1. Erythropoiesis is red blood cell production. 2. Initially, red blood cell formation occurs in the yolk sac, liver and spleen. 3. After an infant is born, red blood cells are produced almost exclusively in the red bone marrow. 6. The average life span of a red blood cell is 120 days. 7. Erythropoietin controls red blood cell production and is released primarily from the kidneys. G. Dietary Factors Affecting Red Blood Cell Production 4. Iron is required for hemoglobin production. 5. Anemia is a reduction in the oxygen-carrying capacity of the blood. I. Types of White Blood Cells 1. White blood cells are also called leukocytes. 2. White blood cells function to protect against diseases. 4. Granulocytes have granules in their cytoplasm. 5. Examples of granulocytes are neutrophils, basophils, and eosinophils. 6. Agranuloctyes lack cytoplasmic granules. 7. Examples of agranuloctyes are monocytes and lymphocytes. 10. Neutrophils are the 1st to respond in an infection – they phagocytize bacteria, fungi, and some viruses. 11. Neutrophils account for about 54%-62% of white blood cells in a blood sample. 14. Eosinophils moderate allergic reactions. 15. Eosinophils make up 1%-3% of the total number of circulating white blood cells. 17. Basophils migrate to damaged tissues where they release histamine. 19. Histamine promotes inflammation. 20. Basophils usually account for less than 1% of leukocytes. 23. Monocytes can leave the blood stream to become macrophages. 24. Monocytes usually make up 3%-9% of white blood cells in a blood sample 26. The major types of lymphocytes are T cells and B cells. 27. T cells attack microorganisms, tumor cells, and transplanted cells. 28. B cells produce antibodies. 29. Lymphocytes account for about 25%-33% of the circulating white blood cells. J. Functions of White Blood Cells 1. Diapedesis is the movement of a WBC out of the blood stream into surrounding tissues. 6. Pus is an accumulation of bacteria, WBCs, and damaged cells. L. Blood Platelets 1. Platelets are also called thrombocytes. 2. Platelets arise from cells called megakaryocytes. 4. Platelets help repair damaged blood vessels by sticking to broken surfaces. III. Hemostasis A. Introduction 1. Hemostasis refers to the stoppage of bleeding. 2. Three actions that may prevent blood loss are blood vessel spasm, platelet plug formation, and blood coagulation. B. Blood Vessel Spasm 1. Vasospasm is smooth muscle contraction in the wall of a blood vessel. 2. Following vasospasm, blood loss lessens. C. Platelet Plug Formation 3. The function of the platelet plug is to prevent blood loss. D. Blood Coagulation a. Coagulation causes the formation of a blood clot. d. Prothrombin converts prothrombin to thrombin. e. The function of thrombin is to convert fibrinogen to fibrin. f. Once fibrin threads form, they stick to exposed surfaces of damaged blood vessels, creating a blood clot. g. A blood clot is composed of fibrin threads that have trapped blood cells and platelets. h. Blood clotting is enhanced by a positive feedback system. i. Normally blood clot formation is prevented by blood flow. IV. Blood Groups and Transfusions A. Antigens and Antibodies 1. Agglutination is the clumping of RBCs and is due to a reaction between RBC surface molecules called antigens and proteins called antibodies. 2. Avoiding the mixture of certain kinds of certain kinds of antibodies and antigens prevents adverse transfusion reactions. B. ABO Blood Group 1. The ABO blood group is based on the presence or absence of antigen A and antigen B on RBC membranes. 2. A person with only antigen A has type A blood. 3. A person with only antigen B has type B blood. 4. A person with both antigen A and antigen B has type AB blood. 5. A person with neither antigen A nor antigen B has type O blood. 6. A person with type A blood has antibody anti-B in their plasma. 7. A person with type B blood has antibody anti-A in their plasma. 8. A person with type AB blood has neither anti-A nor anti-B antibodies in their plasma. 9. A person with type O blood has both anti-A and anti-B antibodies in their plasma. 10. Antibodies anti-A and anti-B do not cross the placenta. 11. The major concern in blood transfusion procedures is that the cells in the donated blood not clump due to antibodies present in the recipient’s plasma. 12. A person with type AB blood is called a universal recipient because type AB lacks both anti-A and anti-B antibodies, so a person with this blood type can receive blood from any other blood type. 13. Type O blood is the universal donor because it lacks antigens A and B, so this blood type can be given to persons of all other blood types. 14. A person with Type A blood cannot receive Type B blood because antibodies in the recipient’s plasma would destroy the RBCs of the donor blood. C. Rh Blood Group 1. The Rh blood group was named after the Rhesus monkey. 2. Blood is said to be Rh positive when Rh antigens are present on RBCs. 3. Blood is said to be Rh negative when Rh antigens are not present on RBCs. 4. Anti-Rh antibodies form only in Rh-negative persons when the Rh negative person is exposed to Rh positive blood. 5. When an Rh-negative woman is pregnant with an Rh positive fetus, she will produce anti-Rh antibodies. Chapter 15: Cardiovascular System I. Introduction A. The cardiovascular system includes the heart and blood vessels. B. Without blood circulation, the tissues lack oxygen and nutrients and waste accumulates. II. Structure of the Heart A. Size and Location of the Heart 1. An average size of an adult heart is generally 14 cm long and 9 cm wide. 2. The heart is bounded laterally by the lungs, anteriorly by the sternum, and posteriorly by the vertebral column. 3. The base of the heart lies beneath the second rib. 4. The apex of the heart is at the level of fifth intercostal space. B. Coverings of the Heart 1. The pericardium is a covering that enclosed the heart and the proximal ends of the large blood vessels to which it attaches. 2. The fibrous pericardium is the outer fibrous layer of the pericardium. 3. The visceral pericardium is a serous membrane that is attached to the surface of the heart. 4. The parietal pericardium is a serous membrane that lines the fibrous layer of the pericardium. 5. The pericardial cavity is the space between the visceral pericardium and parietal pericardium. 6. Serous fluid reduces friction between the pericardial membranes as the heart moves. C. Wall of the Heart 1. The three layers of the heart wall are endocardium, myocardium, and pericardium. 2. The epicardium is composed of a serous membrane that consists of connective tissue covered by epithelium, and it includes blood capillaries, lymph capillaries, and nerve fibers. 3. The middle layer is the myocardium. 4. The myocardium is composed of cardiac muscle tissue. 5. The inner layer is the endocardium. 6. The endocardium consists of epithelium and connective tissue that contains mainly elastic and collagenous fibers. It also contains blood vessels and Purkinje fibers. 7. The endocardium of the heart is continuous with the inner lining of the blood vessels attached to the heart. D. Heart Chambers and Valves 1. The two upper chambers of the heart are the right atrium and the left atrium. 2. The two lower chambers of the heart are the right ventricle and the left ventricle. 3. Auricles are small, earlike projections of the atria. 4. The interatrial septum separates the right and left atrium. 5. The interventricular septum separates the right and left ventricles. 9. The right atrium receives blood from the superior and inferior vena cavae and the coronary sinus. 10. The tricuspid valve is located b/w the rt atrium and rt ventricle and prevents the back flow of blood into the rt atrium. 11. Chordae tendinae are fibrous strings and function to prevent cusps of A-V valves from swinging back into atria. 12. Papillary muscles are located in ventricular walls and contract when the ventricles contract. 13. The right ventricle receives blood from the right atrium. 14. The right ventricle pumps blood into the pulmonary trunk. 15. The pulmonary trunk divides into pulmonary arteries. 16. Pulmonary arteries deliver blood to the lungs. 17. The pulmonary valve is located between the rt. ventricle and pulmonary trunk and opens when the rt. ventricle contracts. 18. Pulmonary veins carry blood from the lungs to the left atrium. 19. Blood passes from the left atrium into the left ventricle. 20. The mitral valve is located b/w the l. atrium and l. ventricle and prevents the back flow of blood into the l. atrium. 21. The left ventricle pumps blood into the aorta. 22. The aortic valve is located between the left ventricle and aorta and opens when the left ventricle contracts. 23. The tricuspid and mitral valves are also called A-V valves because they are positioned between atria and ventricles. 24. The pulmonary and aortic valves are also called semilunar valves because of their structures. IV. Blood Vessels A. Introduction 1. Blood vessels form a closed circuit of tubes that carries blood from the heart to cells and back again. 2. Five types of blood vessels are arteries, arterioles, capillaries, venules, and vein. 3. Arteries conduct blood away from the heart and to arterioles. 4. Venules and veins conduct blood from capillaries and to the heart. 5. The capillaries are sites of exchange of substances between the blood and the body cells. B. Arteries and Arterioles 1. Arteries are strong, elastic vessels that are adapted for carrying the blood away from the heart under high pressure. 2. Arteries give rise to arterioles. 3. The three layers of the wall of an artery are the tunica interna, tunica media, and tunica externa. 4. The inner layer of an artery is called tunica interna and functions to provide a smooth surface for blood flow and prevents blood clotting. 5. The middle layer of an artery is called the tunica media and is composed of smooth muscle fibers. 6. The outer layer is the tunica externa and consists of connective tissues with collagenous and elastic fibers. 10. Vasoconstriction is the contraction of smooth muscle cells in blood vessel walls. 11. Vasodilation is the relaxation of smooth muscle cells in the walls of blood vessels and occurs when the blood vessel diameter increases. 12.Changes in the diameters of arteries and arterioles greatly influence blood flow and pressure. C. Capillaries 1. Introduction a. The smallest diameter blood vessels are capillaries. b. Capillaries connect arterioles to venules. c. The wall of a capillary consists of endothelium. 2. Capillary Permeability a. The most permeable capillaries are located in the liver, spleen, and red bone marrow. b. Protective and tight capillaries are located in the brain. 5. Exchanges in the Capillaries a. The vital function of exchanging gases, nutrients, and metabolic by-products between the blood and the tissue fluid surrounding body cells occurs in the capillaries. b. Biochemicals move through capillary walls by diffusion, filtration, and osmosis. c. Diffusion is the most important means of transfer. d. Oxygen and nutrients diffuse out of the capillary walls into surrounding cells because they are in a lower concentration in surrounding cells. e. Carbon dioxide and other wastes diffuse into the capillary blood because they are in a lower concentration in the capillary blood. Chapter 19: Respiratory System I. Introduction D. Ventilation is the movement of air in and out of the lungs. E. External respiration is the exchange of gases between the air in the lungs and the blood F. Internal respiration is the exchange of gases between the blood and the body cells. III. Organs of the Respiratory System A. Introduction 1. The upper respiratory tract includes nose, nasal cavity, sinuses, and pharynx. 2. The lower respiratory tract includes larynx, trachea, bronchial tree, and lungs. B. Nose 2. Nostrils are openings through which air can enter and leave the nasal cavity. 3. Internal hairs of nostrils prevent entry of large particles carried in air. C. Nasal Cavity 1. The nasal cavity is a hollow space behind the nose. 2. The nasal septum is a structure that divides the nasal cavity into left and right halves. 4. Nasal conchae are located on the lateral walls of the nasal cavity 5. Nasal conchae function to support the mucous membranes and to increase the surface area of the nasal cavity. 6. The lining of the upper portion of the nasal cavity contains olfactory receptors. 7. Most of the nasal cavity conducts air to and from the nasopharynx. 9. The functions of the mucous membrane are to warm and moisten the air, and trap small particles entering the nasal cavity. 10. Cilia of the nasal cavity function to move mucous and any entrapped particles toward the pharynx. D. Sinuses 1. Sinuses are air-filled spaces located within skull bones. 3. The functions of sinuses are to reduce the weight of the skull and to resonate the voice. E. Pharynx 1. The pharynx is located posterior to the oral cavity and between the nasal cavity and the larynx. 2. Functions of the pharynx are to move food into the esophagus, to move air into the larynx. F. Larynx 1. The larynx is an enlargement in the airway superior to the trachea and inferior to the pharynx. 2. The functions of the larynx are to move air into the trachea, prevent foreign objects from entering the trachea, and to house vocal cords. 3. The larynx is composed of a framework of muscles and cartilages bound by elastic tissue. 4. The cartilages of the larynx are thyroid, cricoid, and epiglottic. 5. The thyroid cartilage is located just superior to the thyroid gland. 6. The cricoid cartilage is located inferior to the thyroid cartilage. 7. The epiglottic cartilage is located attached to the upper border of the thyroid cartilage. 8. The epiglottis is flaplike structure supported by the epiglottic cartilage. 9. The functions of the epiglottis are to prevent foods and liquids from entering the air passages and to allow air to pass into the trachea. 14. False vocal cords are composed of muscle tissue and connective tissue with a covering of mucous membrane. 15. The function of the false vocal cords is to help close the larynx during swallowing. 16. The true vocal cords are composed of muscle and elastic fibers. 17. The functions of the true vocal cords are to produce sounds of speech. 18. A higher pitch of the voice is produced by increasing tension on true vocal cords and a lower pitch is produced by decreasing the tension on the cords. 20. The glottis is the opening between vocal cords. G. Trachea 1. The trachea is located anterior to the esophagus in the thoracic cavity. 2. The trachea splits into right and left bronchi. 3. The inner wall of the trachea is lined with a ciliated mucous membrane that contains many goblet cells. 4. The mucous membrane of the trachea functions to filter incoming air and to move entrapped particles upward into the pharynx where the mucous can be swallowed. 5. The wall of the trachea is composed of C shaped pieces of hyaline cartilage, smooth muscle, and connective tissues. 6. The cartilaginous rings of the trachea prevent the trachea from collapsing and blocking the airway. 7. The soft tissues that complete the rings in the back of the trachea allow the esophagus to expand as food moves through it. 8. A blocked trachea causes asphyxiation. 9. A tracheostomy is the production of a temporary hole in the trachea. H. Bronchial Tree 1. Introduction a. The bronchial tree consists of branched airways leading from the trachea to the microscopic air sacs in the lungs. b. Primary bronchi are the first branches of the trachea. c. The carina is ridge of cartilage that separates the primary bronchi. d. Each bronchus, accompanied by blood vessels and nerves, enters its respective lung. 2. Branches of the Bronchial Tree a. Primary bronchi branch into secondary bronchi. b. Secondary bronchi branch into tertiary bronchi. c. Tertiary bronchi branch into terminal bronchioles. f. Terminal bronchioles branch into alveolar ducts. h. Alveolar ducts give rise to alveoli j. Alveoli are thin-walled, microscopic air sacs that open to an alveolar sac. I. Lungs 1. The lungs are cone shaped and located the thoracic cavity. 4. Visceral pleura are serous membranes attached to the surfaces of the lungs. 5. Parietal pleura is a serous membrane that lines the thoracic cavity. 6. The pleural cavity is the potential space between the visceral pleura and parietal pleura. 7. The functions of serous fluid are to lubricate serous membranes and reduce friction during lung movements. 8. The lobes of the right lung are superior, middle, and inferior. 9. The lobes of the left lung are superior and inferior. IV. Breathing Mechanism A. Introduction 1. Breathing or ventilation is the movement of air from outside the body into the bronchial tree and alveoli, followed by a reversal of this air movement. 2. Inspiration is inhalation. 3. Expiration is exhalation. B. Inspiration 1. The force that moves air into the lungs is atmospheric pressure. 2. If the pressure inside the lungs and alveoli decreases, outside air will flow into the airways. 3. The diaphragm is located just inferior to the lungs and is composed of skeletal muscle. 4. The nerves that stimulate the diaphragm are the phrenic nerves. 5. When the diaphragm contracts it moves inferiorly and the thoracic cavity enlarges. 6. When the thoracic cavity enlarges, the intra-alveolar pressure decreases. 7. When intra-alveolar pressure falls, air is moved into the airways. 8. The action of ext. intercostals muscles is to raise the ribs and the sternum, which inc. the size of the thoracic cavity. 9. When intercostals muscles move the thoracic wall upward and outward, the parietal pleura and visceral pleura move. 10. Movement of the parietal and visceral pleura upward and outward expands the lungs in all directions. 11. Surface tension is the attraction of certain molecule to each other. 12. Surfactant is located in alveolar spaces and functions to reduce the alveoli’s tendency to collapse. 13. If a person takes a deeper than normal breath, the diaphragm and ext. intercostals muscles contract to a greater extent. 14. Other muscles that can be used to enlarge the thoracic cavity are the pectoralis minors and sternocleidomastoids. C. Expiration 1. The forces responsible for normal expiration come from elactic recoil of lung tissues and from surface tension. 2. As the diaphragm and external intercostals muscles relax, the elastic tissues cause the lungs to recoil. 3. Air is forced out of respiratory passageways because intra-alveolar pressure rises above atmospheric pressure. 4. Muscles that aid in a more forceful exhalation than normal are internal intercostal muscles and abdominal wall muscles. D. Respiratory Volumes and Capacities 1. Spirometry is the measure of air volumes. 2. A respiratory cycle is one inspiration plus the following expiration. 3. Tidal volume is the amount of air that enters of leaves during a respiratory cycle. 4. Inspiratory reserve volume is the additional quantity of air after the resting tidal volume that can enter the lungs. 5. Expiratory reserve volume is the additional quantity of air that can exit the lungs after a resting tidal volume. 6. Residual volume is the amount of air that remains in the lungs after a forceful expiration. 7. Vital capacity is maximum amount of air that can be exhaled after taking the deepest breath possible. 8. Inspiratory capacity is maximum volume of air that can be inhaled following exhalation of tidal volume. 9. Functional residual capacity is volume of air that remains in the lungs following exhalation of tidal volume. 10. Total lung capacity is total volume of air that the lungs can hold. 14. A spirometer measures respiratory air volumes. 15. Respiratory volumes and capacities are used to evaluate the course of respiratory illnesses. V. Control of Breathing A. Respiratory Center 1. The respiratory center is composed of groups of neurons in the brainstem which controls breathing. 2. The functions of the respiratory center are to cause inhalation and exhalation, and to adjust the rate and depth of breathing. 3. The components for the respiratory center are located widely scattered throughout the pons and medulla oblongata. 4. The medullary rhythmicity area includes two groups of neurons that extend throughout the medulla oblongata. 5. The dorsal respiratory group is responsible for the basic rhythm of breathing. 6. The functions of the ventral respiratory center are to generate impulses for more forceful breathing movements. 7. The functions of the pneumotaxic area are to regulate the duration of inspiratory bursts originating from the dorsal group. This area basically controls the rate of breathing. VIII. Gas Transport A. Introduction 1. The blood transports oxygen and carbon dioxide between the lungs and the body cells. 2. As oxygen and carbon dioxide enter blood, they dissolve in plasma or combine chemically with other atoms or molecules. B. Oxygen Transport 1. Almost all the oxygen carried in blood is bound to hemoglobin. 2. A small amount of oxygen is carried in blood dissolved in plasma. 3. Hemoglobin consists of two types of components called heme and globin. 4. Each heme group contains an atom of iron. 5. Oxyhemoglobin is the combination of oxygen and hemoglobin. 7. Factors that promote the release of oxygen from hemoglobin are a decrease in the partial pressure of oxygen, increasing blood concentrations of carbon dioxide, acidity, and increased temperatures. C. Carbon Dioxide Transport 1. Blood flowing through capillaries gain carbon dioxide because the tissues have a high partial pressure of carbon dioxide. 2. Carbon dioxide is transported to lungs in one of the following three forms: bound to hemoglobin, dissolved in plasma, or as bicarbonate ions. 3. Carbaminohemoglobin is the combination of carbon dioxide and hemoglobin. 5. The most important carbon dioxide transport mechanism involves the formation of bicarbonate ions. 6. Carbon dioxide forms carbonic acid when it reacts with water. 7. Carbonic anhydrase is an enzyme that speeds up the reaction between carbon dioxide and water and is located inside red blood cells. 8. Carbonic acid dissociates into hydrogen ions and bicarbonate ions. Chapter 16: Lymphatic System and Immunity I. Introduction A. The lymphatic system is closely associated with the cardiovascular system because it includes a network of vessels that assist in circulating body fluids. B. Lymphatic vessels transport excess fluid away from interstitial spaces and return it to the bloodstream. C. Lacteals are lymphatic capillaries in the lining of the small intestine and function to transport fats to the venous system. D. The organs of the lymphatic system also defend the body against infection by disease-causing agents. II. Lymphatic Pathways A. Lymphatic Capillaries 1. Lymphatic capillaries are microscopic, closed-ended tubes that extend into interstitial spaces. 2. The walls of lymphatic capillaries are similar to blood capillaries. 3. The thin walls of capillaries make it possible for tissue fluid from interstitial space to enter the lymphatic capillaries. 4. Lymph is fluid inside a lymphatic capillary. B. Lymphatic Vessels 1. The walls of lymphatic vessels are similar to those of veins. 2. Lymphatic vessels have valves that prevent backflow of lymph. 3. Larger lymphatic vessels lead to lymph nodes. 4. After leaving nodes, lymphatic vessels merge together to form lymphatic trunks. C. Lymphatic Trunks and Collecting Ducts 1. Lymphatic trunks drain lymph from lymphatic vessels and are named for the regions they serve. 2. Examples of lymphatic trunks are lumbar, intestinal, intercostal, bronchomediastinal, subclavian, and jugular trunks. 3. Lymphatic trunks join one of two collecting ducts. 4. The two collecting ducts are the thoracic duct and right lymphatic duct. 5. The thoracic duct is located along side the aorta in the abdominal and thoracic cavity and empties into the left subclavian vein. 6. The thoracic duct drains lymph from the intestinal, lumbar, and intercostal trunks, as well as from the left subclavian, left jugular, and left bronchomediastinal trunks. 7. The right lymphatic duct is located on the right side of the thorax and empties into the right subclavian vein. 8. The right lymphatic duct drains right jugular, right subclavian, and right bronchomediastinal trunks. 9. After leaving the two collecting ducts, lymph enters the venous system and becomes part of the plasma. III. Tissue Fluid and Lymph A. Introduction 1. Lymph is tissue fluid that has entered a lymphatic capillary. 2. Lymph formation depends on tissue fluid formation. B. Tissue Fluid Formation 1. Capillary blood pressure filters water and small molecules from plasma and the resulting fluid consists of water, nutrients, gases, and hormones (a similar composition to plasma). 2. Water is drawn back into capillaries because of plasma colloid osmotic pressure. C. Lymph Formation 1. Filtration from the plasma normally exceeds reabsorption, leading to the formation of tissue fluid. 2. Tissue fluid moves into lymphatic capillaries because of interstitial fluid hydrostatic pressure. 3. Lymph formation prevents edema. D. Lymph Function 1. Lymphatic vessels in the small intestine play a major role in the absorption of dietary fats. 2. Lymph returns very small proteins that the blood capillaries filtered to the bloodstream. 3. Lymph transports foreign particles to lymph nodes. 4. Lymphatic capillaries can receive proteins and foreign particles that blood capillaries cannot because the epithelial cells that form the walls of lymphatic vessels overlap each other but are not attached. 5. The lumen of a lymphatic capillary remains open because their epithelial cells are attached to surrounding connective tissue cells by protein filaments. IV. Lymph Movement A. Introduction 1. The hydrostatic pressure of tissue fluid drives lymph into lymphatic capillaries. 2. Muscular activity largely influences movement of lymph through lymphatic vessels. B. Lymph Flow 1. Lymph is under relatively low hydrostatic pressure. 2. Contracting skeletal muscles compress lymphatic vessels. 3. Lymph does not flow back because of valves. 4. Breathing aids lymph circulation by creating a relatively low pressure in the thorax and a relatively high pressure in the abdomen during inhalation. C. Obstruction of Lymph Movement 1. Conditions that interfere with lymph movement causes fluid to accumulate within interstitial spaces. 2. The continuous movement of lymph from interstitial spaces into blood capillaries and lymphatic capillaries stabilizes the volume of fluid in interstitial spaces. V. Lymph Nodes A. Introduction 1. Lymph nodes are located along lymphatic pathways. 2. Lymph nodes contain lymphocytes and macrophages which fight invading microorganisms. B. Structure of a Lymph Node 1. The hilum of a lymph node is the indented region. 2. Afferent lymphatic vessels are those that carry lymph to a node. 3. Efferent lymphatic vessels are those that carry lymph away from a node. 4. Lymph nodules are divisions of a lymph node. 5. Germinal centers contain dense masses of actively dividing lymphocytes and macrophages. 6. Tonsils are composed of partially encapsulated lymph nodules. 7. Peyer’s patches are located in the mucosal lining of the distal portion of the small intestine and are composed of M cells, macrophages, and lymphocytes. 8. Lymph sinuses are a network of chambers and channels through which lymph circulates. C. Locations of Lymph Nodes 1. Lymph nodes generally occur in groups or chains along the paths of larger lymphatic vessels but are absent in the central nervous systems. 2. Major locations of lymph nodes are cervical region, axillary region, inguinal region, pelvic cavity, abdominal cavity, thoracic cavity, and supratrochlear region. 3. Lymph nodes of the cervical region are associated with lymphatic vessels that drain the skin of the scalp and fact, as well as tissues of the nasal cavity and pharynx. 4. Lymph nodes of the axillary region are associated with lymphatic vessels that drain the upper limbs, wall of the thorax, mammary glands, and upper abdominal wall. 5. Lymph nodes of the inguinal region are associated with lymphatic vessels that receive lymph from the lower limbs, external genitalia, and lower abdominal wall. 6. Lymph nodes of the pelvic cavity are associated with lymphatic vessels that drain the pelvic viscera. 7. Lymph nodes of the abdominal cavity are associated with lymphatic vessels that drain the abdominal viscera. 8. Lymph nodes of the thoracic cavity are associated with lymphatic vessels that drain thoracic viscera and the internal wall of the thorax. 9. Lymph nodes of the supratrochlear region are associated with lymphatic vessels that drain the elbow region. D. Functions of Lymph Nodes 1. The two primary functions of lymph nodes are to filter potentially harmful particles from lymph and to monitor body fluids. 2. Along with the red bone marrow, lymph nodes are centers for lymphocyte production. 3. Lymphocytes attack viruses, bacteria, and other parasitic cells. 4. The functions of macrophages are to engulf and destroy foreign substances, damaged cells, and cellular debris. VII. Thymus and Spleen A. Thymus 1. The thymus is composed of lymphocytes and connective tissues and is located in the mediastinum . 2. After puberty, the thymus begins to shrink. 3. Most cells of the thymus gland are thymocytes. 4. The hormones secreted by the thymus gland are called thymosins. 5. Thymosins function to stimulate maturation of T lymphocytes. B. Spleen 1. The largest lymphatic organ is the spleen. 2. The spleen is located in the upper left portion of the abdominal cavity. 3. The spleen resembles a large lymph node. 4. White pulp contains many lymphocytes. 5. Red pulp contains red blood cells, lymphocytes, and macrophages. 6. The functions of the spleen are to remove foreign particles, damaged red blood cells, and cellular debris from the blood. VIII. Body Defenses Against Infection A. A pathogen is disease-causing agents. B. An infection is the presence of pathogens. C. Examples of pathogens are bacteria, viruses, and fungi. D. Innate defenses are general defenses and protect against many types of pathogens and include species resistance, mechanical barriers, enzyme actions, interferon, fever, natural killer cells, inflammation, and phagocytosis. E. Adaptive defenses are very precise defense mechanisms and are carried out by lymphocytes. IX. Innate Defenses A. Species Resistance 1. Species resistance refers to the fact that a given kind of organism or species develops diseases that are unique to it. 2. A species may be resistant to diseases that affect other species because its tissues somehow fail to provide the temperature of chemical environment that a particular pathogen requires. B. Mechanical Barriers 1. Mechanical barriers prevent the entrance of some infectious agents. 2. Examples of mechanical barriers are skin, mucous membranes, and hair. 3. The first line of defense is a mechanical barrier. 4. The second line of defense is a collection of the other nonspecific defenses. C. Chemical Barriers 1. Chemical barriers are body fluids containing enzymes or antimicrobial substances. 2. Examples of chemical barriers are gastric juice, interferons, defensins, and collectins. 3. Interferon is produced by lymphocytes and fibroblasts and its functions include stimulation of phagocytosis, and to prevent viral infections. 4. Defensins are produced by white blood cells, and certain epithelial cells. 5. The functions of defensins are to make holes in bacterial cells walls and to destroy certain pathogens. 6. Collectins are proteins and their functions include protecting the body against viruses, bacteria, and yeasts. D. Fever 1. A fever begins when a viral or bacterial infection stimulates lymphocytes to produce interleukin-1. 2. The functions of fever are to increase phagocytosis and to prevent bacteria and other pathogens from obtaining iron. E. Natural Killer Cells 1. Natural killer cells are a small population of lymphocytes. 2. Functions of natural killer cells are to protect the body against cancer and viruses. 3. Perforins are cytolytic substances secreted by natural killer cells. F. Inflammation 1. Inflammation produces redness, swelling, heat and pain. 2. Redness of inflammation is the result of dilated blood vessels. 3. Swelling of inflammation is the result of increases capillary permeability. 4. Heat of inflammation is the result of the entry of blood from deeper body parts. 5. Pain of inflammation is the result of stimulation of pain receptors. 6. Cells that commonly migrate to areas of inflammation are neutrophils and monocytes. 7. Pus is the result of an accumulation of white blood cells, bacterial cells, and cellular debris. 8. The functions of inflammation are to prevent the spread of infection, to clear infection, and to promote healing of damaged tissues. G. Phagocytosis 1. Phagocytosis removes foreign particles. 2. Examples of phagocytic cells are neutrophils, monocytes, and macrophages. 3. The mononuclear phagocytic system is monocytes, macrophages, and neutrophils that are spread throughout the body. X. Adaptive Defenses or Immunity A. Introduction 1. Immunity is resistance to particular pathogens or to their toxins or metabolic by-products. 2. An immune response is based on the ability to distinguish molecules that are part of the body from those that are foreign. 3. Antigens are molecules that can elicit an immune response. 4. Lymphocytes and macrophages carry out immune responses. B. Antigens 1. Receptors on lymphocyte surfaces enable cells to recognize foreign antigens. 2. Antigens may be proteins, polysaccharides, glycoproteins, or glycolipids. 3. The antigens most effective in eliciting an immune response is large and complex, with few repeating parts. 4. A hapten is a small molecule that must bind to a larger molecule to elicit an immune response. 5. Examples of haptens are chemicals found in drugs, household cleaners, dust, and skins of certain animals. C. Lymphocyte Origins 1. T cells are derived from red bone marrow and the thymus gland. 2. B cells are derived from red bone marrow. 3. The blood distributes B cells. 4. B cells and T cells are abundant in lymph nodes, the spleen, bone marrow, and the intestinal lining. D. Lymphocyte Functions 1. The cellular immune response is cell-to-cell contact between a T cell and antigen cell. 2. Cytokines are produces by T cells. 3. Examples of cytokines are interleukins, colony-stimulating factors, interferons, and tumor necrosis factors. 4. Functions of cytokines are to stimulate the production of lymphocytes, block viral replication, stimulate phagocytosis, stimulate production of antibodies, and to stop growth of tumor cells. 5. T cells may also secrete toxins that kill antigen-bearing cells, growth-inhibiting factors that prevent target cell growth, or interferon that prevent viral and tumor cell proliferation. 6. B cells differentiate into plasma cells. 7. Plasma cells produce antibodies. 8. The humoral immune response is the immune response that is mediated by antibodies. 9. A clone is a cell that is identical to the cell from which it was derived. 10. Different varieties of T cells and B cells have a particular type of antigen receptor on their cell membranes that can respond only to a specific antigen. E. T Cells and the Cellular Immune Response 1. A lymphocyte must be activated before it can respond to an antigen. 2. T cell activation requires the presence of processed fragments of antigen attached to the surface of another kind of cell. 3. Antigen-presenting cells are macrophages, B cells, and other cell types. 4. T cell activation begins when a macrophage phagocytizes a bacterium and moves the antigens of the bacterium to its membrane. 5. The major histocompatibility complex is a complex of proteins found on the surface of antigen-presenting cells. 6. MHC antigens help T cells recognize an antigen as foreign. 7. Class I MHC antigens are located on cell membranes of all cells except red blood cells. 8. Class II MHC antigens are located on cell membranes of antigen-presenting cells, thymus cells, and activated T cells. 9. The functions of helper T cells are to stimulate B cells to produce antigens and to secrete cytokines. 10. The functions of cytotoxic T cells are to eliminate viral infected cells and tumor cells. 11. The functions of memory T cells are to respond to an antigen during a future exposure and to differentiate immediately into cytotoxic T cells. F. B Cells and the Humoral Immune Response 1. Introduction a. B cells may become activated when an antigen binds to its membrane-bound receptor. b. Upon activation, B cells divide repeatedly. c. T cells help B cells by releasing cytokines that stimulate B cell proliferation and antibody production. d. The functions of memory B cells are to respond rapidly to subsequent exposures to a specific antigen. e. The functions of plasma cells are to secrete antibodies. f. An immune response may include several types of antibodies manufactured against a single microbe because pathogens often have different antigens on their surfaces. g. A polyclonal response is the production of several different antibodies against one pathogen. 2. Antibody Molecules a. Antibodies are soluble, globular proteins b. Each antibody is composed of four chains of amino acids that are linked together. c. The light chains are identical and contain about half the number of amino acids as the heavy chains. d. The heavy chains are identical and contain twice as many amino acids as the light chains. e. The five major types of antibodies are distinguished by a particular kind of heavy chain. f. The variable region is the part of the antibody that contains variable regions of amino acids. g. Variable regions are specialized to react to the shape of a specific antigen molecule. h. Antigen-binding sites are specialized ends of antibodies that bind to antigens. i. Idiotypes are the particular parts of antigen-binding sites that actually bind to antigens. j. Constant regions are the parts of an antibody other than their variable regions. 3. Types of Immunoglobulins a. The five major types of immunoglobulins are IgG, IgA, IgM, IgD, and IgE. b. The three types of immunoglobulins that make up the bulk of circulating antibodies are IgG, IgA, and IgM. c. IgG is found in tissue fluid and plasma. d. The functions of IgG are to defend against bacterial, viruses, and toxins; it also activates complement. e. IgA is found in exocrine gland secretions. f. The functions of IgA are to defend against bacteria and viruses. g. IgM is found in plasma. h. The functions of IgM are to react with antigens occurring on red blood cells and to activate complement. i. IgD is found in the cell membranes of B cells. j. The functions of IgD are to act as receptors for B cells. k. IgE is located in exocrine gland secretions. l. The functions of IgE are to promote inflammation and allergic reactions. 4. Antibody Actions a. The three ways antibodies react to antigens are to directly attack antigens, activate a set of enzymes that attack antigens, or stimulate localized changes that help prevent the spread of the antigens. b. In a direct attack, antibodies combine with antigens and cause them to clump. c. Phagocytic cells can engulf antigens more readily when they have clumped together. d. Antibodies can also cover the toxic portions of antigens and neutralize their effects. e. Complement is a group of proteins in plasma and other body fluids. f. Complement is activated by the binding of certain antibodies to antigens. g. Functions of complement are opsonization, chemotaxis, cell lysis, and inflammation. h. IgE antibodies are usually attached to membranes of mast cells. i. Mast cells release their biochemicals when antigens combine to antibodies on their surfaces. G. Immune Responses 1. The primary immune response occurs when a person is first exposed to an antigen. 2. Following a primary immune response, some B cells produce memory cells. 3. The secondary immune response occurs when a person is later exposed to an antigen and memory cells are activated. H. Practical Classification of Immunity 1. Naturally acquired active immunity develops when a person is naturally exposed to an antigen. 2. Artificially acquired active immunity develops when a person is given a vaccine. 3. A vaccine is an injection of a dead or weakened antigen that promotes an immune response. 4. Artificially acquired passive immunity occurs when a person is injected with antibodies or anti-toxins. 5. Naturally acquired passive immunity occurs when antibodies are passed across the placenta or through mother’s milk. I. Allergic Reactions 1. An allergic reaction is an immune response against a nonharmful substance. 2. Allergens are substances that trigger allergic reactions. 3. An immediate-reaction allergy occurs when an allergens bind to IgE antibodies and allergy mediators are released from mast cells and basophils. 4. Anaphylactic shock is a severe form of immediate-reaction allergy that may lead to death. 5. Antibody-dependent cytotoxic reactions occur when an antigen binds a specific cell, simulating phagocytosis and complement-mediated lysis of the antigen. 6. Immune complex reactions occur when antigen-antibody complexes cannot be cleared from the body. 7. Autoimmunity refers to the loss of the ability to tolerate self-antigens. 8. A delayed-reaction allergy occurs when a person is repeatedly exposed to an allergen and the allergic reaction occurs about 48 hours after exposure to the antigen. J. Transplantation and Tissue Rejection 1. Transplanted tissues and organs include corneas, kidneys, lungs, pancreases, bone marrow, skin, livers, and hearts. 2. A tissue rejection reaction is the destruction of transplanted tissue by the recipient’s immune system. 3. Tissues are rejected because the cell surface molecules (MHC antigens) of the donor tissue are recognized as foreign by the recipient. 4. Isografts are grafts from an identical twin. 5. Autografts are grafts from one’s self. 6. Allografts are grafts from another person. 7. Xenografts are grafts from a different species. 8. Immunosuppressive drugs are used to reduce rejection of transplanted tissues. K. Autoimmunity 1. Autoantibodies are antibodies that cannot distinguish self from nonself. 2. Reasons people develop autoimmunities are viruses may incorporate some self proteins into its coating and the body then recognizes the self proteins as foreign in all cells, T cells may never learn to differentiate between self and nonself cells, or some antigens may resemble self antigens. 3. Scleroderma is a condition caused by autoimmunity that produces fatigue, swollen joints, stiff fingers, hardened blood vessels, and a mask like face. XI. Life-Span Changes A. The immune system begins to decline early in life. B. By age 70, the thymus is one-tenth of its original size. C. Elderly people have a higher risk of developing cancer and infections because the strength of their immune systems has declined. D. AIDS is more difficult to diagnose in older people because physicians do not initially suspect the condition. E. Elderly people may not be candidates for certain medical treatments because of their declining immune systems.