Fall OMS I exam 1 2014 CLIs
advertisement

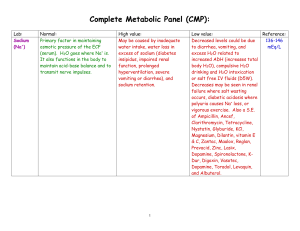
Common learninG ISSUES PBL TEST 1 2014 Carbon Dixoide (CO2) • Normally 23-30 mmol/L • CO2 excreted into blood as bicarbonate-> NOT THE SAME THING AS PCO2 • Regulated by the kidneys; rough guide for acid-base studies • Increased: COPD, severe vomiting, primary cause of metabolic alkalosis; kidney compensation in respiratory acidosis • Decreased: Starvation, diabetic ketoacidosis, diarrhea, dehydration; primary cause of metabolic acidosis and a response to respiratory alkalosis, loop diuretics, BMP vs. CMP • BMP/Chem-7: • • • • • • • Sodium Chloride Potassium CO2/Bicarbonate BUN Creatinine Glucose • CMP/Chem-12: • Same as BMP plus: • • • • • AST ALT Albumin Bilirubin Alkaline Phosphatase Chloride (Cl) • Normally 98-106mEq/L • Major extracellular anion; follows Na to maintain electroneutrality • Increased: Diarrhea, hyperalimentation • Decreased: Vomiting, renal disease, diabetic ketoacidosis • Normally Cl values will not change by themselves; will accompany shifts in either HCO3 or Na creatinine • In chronically unstable patients acute changes in renal function can make real time evaluation of GFR difficult • Cystatin C may be used for chronic kidney disease • Clearance: amount of filtrate made • Amount of blood to be filtered and ability of glomeruli to filter Creatinine • Normally <1.1 mg/dl • Measures blood flow through kidneys (used to approximate GFR) • Increased: Renal failure, false positive seen in diabetic ketoacidosis • Decreased: Muscle wasting, (MINIMAL effect from liver disease) creatinine • Catabolic product of creatine phsophate used in skeletal muscle contraction, depends on muscle mass • Excreted by kidneys and is directely proportional to renal excretory function; serum levels should be constant • Used to diagnose impaired renal function • Unlike BUN it is minimally affected by hepatic function • Approximation of GFR • Suggest chronic disease Glucose • Normally 80-140 mg/dl • Slight increase normal with aging • Increased: DM, Cushing’s syndrome, pancreatitis, thiazide diuretics, stress, steroids • Decreased: Liver disease, insulin overdose, malnutrition, sepsis, endocrine tumors, renal failure • HIGHLY dependent on time of day, if pt was fasting, etc. HbA1c is a better determinant of long-term glycemic controls. Potassium (K) • • • • Normally 3.5-5 mEq/L Major intracellular cation Hemolysis may falsely elevate level Increased: Renal failure, Addison’s disease, dehydration, ACE inhibitors, Spironolactone • Decreased: Diuretics, NG suctioning, vomiting, diarrhea, metabolic alkalosis Sodium (Na) • Normally 136-145 mmol/l • Major cation in extracellular space (was a question last year); major determinant of extracellular osmolarity • Increased: Diabetes inspidius, exessive sweating, Cushing’s syndrome, burns • Decreased: Excess body water/excess intake (CHF, renal failure, small cell lung cancer, brain disorders), hypothyroidism, vomiting, diarrhea, pancreatitis, SIADH • Regulated by aldosterone; increased levels will stimulate ANP (Atrial naturietic factor is stimulated by +Na), ADH (antidiuretic hormone, increased levels will decrease levels of Na) BUN • Shock, dehydration, congestive heart failure, excessive protein catabolism • GI bleeding • If kidney disease is unilateral and other kidney can take on role then BUN won’t be affected • Ureteral and urethral obstruction • Liver disease decreased BUN (urea cycle takes place in the liver) • Can be normal if there is liver and kidney disease BUN • • • • 10-20 mg/dL adult Child and infant 5-18 mg/dL Newborn 3-12 mg/dL Rough and indirect measurement of renal function and GFR also a measure of liver function • Amount of urea nitrogen in the blood • Urea is an end product of protein metabolism and digestion • Elevated bun or azotemia BUN (BLOOD Urea Nitrogen) • • • • • • Normally 10-20 mg/dl (adults) Indirect measure of GFR and liver function Increased: Renal failure, CHF, aminoglycosides Decreased: Starvation, liver failure BUN:Creatinine >20 suggests dehydration BUN:Creatinine >30 suggests GI bleed HEMATOCRIT • Decreased levels: anemia (reduced number of RBCs), elevated white counts, pregnancy, cirrhosis, hemolytic anemia (destruction of RBCs), iron/dietary deficiency, bone marrow failure. Renal failure kidney makes EPO, collagen vascular disease, anemia • Increased levels:, erythrocytosis, polycythemia, dehydration, macrocytic anemias,living at altitude, congenital heart diseases (response to hypoxia), COPD • Values NOT reliable immediately after hemorrhage-a question last year; percentage of total blood volume taken up by RBCs hasn’t changed. The value will only decrease after fluid repletion • Know figure 2-17, it was on last year’s exam • Indications for transfusions (normally 24%)vary with age Hematocrit • Normal Values: Male 42-52% (.42-.52) Female 37-47% (.37-.47); Critical <15% or >60% • Indirect measurement of RBC number and volume; regularly measured in a CBC • Percentage of total blood volume made by RBCs; ratio of the height of the RBC column after centrifugation compared to total height of column • Approximately 3* Hgbn values under normal circumstances • Women have lower values than men; also decreases with age HEMOGLOBIN • Measure of total amount of Hgb in peripheral blood-oxygen carrying capacity of blood • Women and elderly-decreased values • Changes in plasma volume accurately reflected by Hgb concentration (overhydration will increase, dehydration will increase) • Slight diurnal variation in Hgb levels (highest in the morning) • Causes of high hgb: smoking, altitude • Decreased levels (hypochromic): anemia (reduced number of RBCs), elevated white counts, pregnancy, cirrhosis, hemolytic anemia (destruction of RBCs), iron/dietary deficiency, bone marrow failure. Renal failure kidney makes EPO, collagen vascular disease, anemia • Increased levels (hyperchromic):, erythrocytosis, Platelet count • Platelet count • Number of platelets formed in bone marrow of megakaryocytes • Adult/child 150,000-400,000 • Newborn/ premature infant: 100,000-300,000 • Infant 200,000-475,000 • Counts <100,000= Thrombocytopenia; >400,000=thrombocytosis; >1 million= thrombocythemia • • Even pts with elevated blood platelet counts experience bleeding, because functions like aggregation may be abnormal Thrombocytopenia causes spontaneous bleeding, causing petechiae (small bruising) and echymoses (large bruises) • Survival in blood is 7-9 days Platelet count • Causes of thrombocytopenia: reduced production (bone marrow failure, tumor); sequestration of platelets (hypersplenism), accelerated destruction of platelets (antibodies, infections, drugs), disseminated intravascular coagulation, hemorrhage,dilutional, thrombotic thrombocytopenias like HELLP (eclampsia= hemolysis, elevated liver enzymes, low platelet count).pernicious anemia (B12 is necessary for platelet production) • Causes of thrombocytosis: malignancys (leukemia, lymphoma, solid tumors of the colon); polycythemia vera; postsplenectomy (it’s the spleen’s job to destroy old “senescent” RBCS), rheumatoid arthritis, iron deficiency anemia RBC Count/erythrocyte count • • • • Normal findings: Adult male: 4.7-6.1; Adult female 4.2-5.4 Number of cicularing RBCS in 1 mm3 peripheral venous blood Production is stimulated by erythropoeiten Abnormal or old RBCs destroyed by the spleen; intravascular injury like atherosclerotic plaques shortens the RBC life • Overly active spleen will also destroy RBCs • Anemia= 10% less than normal values CBC • • • • • • • • Measures RBC Hemoglobin Hematocrit RBC Indices WBC count Blood smear Platelet count Mean platelet volume CBC • Mean corpuscular volume ( MCV) • • • • Average volume or size of a single RBC Divide hematocrit by total RBC count (Hct*10%/RBC) Large “macrocytic”: folic acid or B12 deficiency Small “microcytic”: iron deficient anemia or thalassemia • RBC • # circulating RBC • Normal life span 120 days • Lysed and extracted from circulation by spleen CBC • Mean corpuscular hemoglobin • Measure of average weight of hemoglobin within RBC • Hgbn*10/RBC • Mean corpuscular hemoglobin concentration (MCHC) • Average concentration or % of hemoglobin within RBC (Hgbn*100/Hct) • RBC distribution width • Indicates variation of size of RBC • Important in classifying anemias CBC • Blood smear • Information concerning drugs and diseases that affect RBCs and WBCs • Examines RBC, platelet, and WBC • White count • Neutrophils, basophils, eosinophils, monocytes, lymphocytes White Blood Count • Normally 5,000-10,000 • Differential provides more clues to cause than overall count does • Increased: Infection, inflammation, leukemia, trauma, stress • Decreased: Bone marrow failure, vitamin B12 deficiency Cause of Increased Differentials • • • • Basophils: Leukemia, s/p spleenectomy Eosnophils: Allergies, asthma, parasites Lymphocytes (B cells/T cells): Viral infections, leukemia Monocytes: Bacterial infections, protozoan infections, ulcerative colitis • Neutophils: Bacterial infection, noninfectious tissue damage, metabolic disorders ALPHA-FETOPROTEIN • NORMAL FINDINGS < 40 ng/mL • Child < 30 ng/mL • Ranges vary by week of gestation normally detected at 10 weeks • Peak levels at 16-18 weeks • DECREASED LEVELS: • TRISOMY 21 • FETAL WASTAGE • INCREASED LEVELS: • • • • • NTD, ABDOMINAL WALL DEFECTS MULTIPLE FETUSES THREATENED ABORTION FETAL DISTRESS OF CONGENITAL ANOMALIES FETAL DEATH ALPHA FETOPROTEIN • • • USED AS A SCREENING MARKER INDICATING INCREASED RISK FOR BIRTH DEFECTS (NEURAL TUBE, BODY WALL, AND CHROMOSOMAL) PRODUCED BY FETAL LIVER AND YOLK SAC IF THERE IS A BODY WALL DEFECT THE AFP WILL LEAK INTO AMNIOTIC FLUID AND IS PICKED UP BY MATERNAL SERUM ALSO ASSOCIATED WITH TUMOR MARKERS, HEPATOMA, TERATOMA, HODGKINS, LYMPHOMA, AND RENAL CELL CARCINOMA karotype • Study an individual’s chromosome makeup to determine chromosomal defects associated with disease or risk for developing disease • Congenital or acquired because of duplication, deletion, translocation, reciprocation, or genetic rearrangement • Indicated with family hx of disease or advanced maternal age • Performed by a banding technique, pairing similar chromosomes based on size (arranged largest to smallest), location of centromere, banding patterns • Congenital anomalies, growth and mental retardation, infertility, delayed puberty, hypogonadism, amenorrhea, ambiguous genitalia, CML, neoplasm recurrent miscarriage, turner, klinefelter, downs hCG • <5 for non-pregnant people, used to diagnose pregnancy, increases throughout pregnancy, can be detected as early as 10 days post conception • Secreted by placental trophoblast • Immunologic test: high risk of false positive • Beta subunit characteristic of hCG • Radioimmunoassay: blood test for beta • Radioreceptor assay performed in one hour reliable • Ectopic pregnangy, hydatiform mole, and choriocarcinoma can produce • Liver cancer cells as well amniocentesis • Performed on women whose pregnancies are high risk (diabetic, obese, older); usually at 24-25 weeks (earliest possible is 12-14 weeks) • Indicate fetal maturity, distress, risk for RDS, genetic and chromosomal abnormalities, sex, NTD • Lung maturity (lecithin and sphingomyelin ratio) lecithin is a major constituent of surfactant 2:1 indicates maturity; at 35 weeks rapidly increases amnio • Phosphatidyglycerol (PG) small component of surfactant, produced by mature lung alveolar cells appear at 35 weeks • Lamellar body count: produce by type II pneumocytes, represent the storage of surfactant • Microviscosity: aggregates dependent on L/S ratio and degree of saturation of fatty acid side chains, high early decreases later amnio • Rh isoimmunization: assess levels of bilirubin in amniotic fluid, indicates severity of hemolytic anermia in Rh-sensitized pregnancy higher bilirubin, lower fetal hemoglobin, early delivery or blood transfusion may be indicated • Anatomic abnormalities: increased AFP neural crest abnormality • Fetal distress: pale, straw colored fluid tinged with green, yellow indicates blood incompatibility, yellow-brown may be intrauterine death red is blood contamination Gravida-para • Gravida = total number of pregnancies • Para = or outcomes of pregnancies • Often after you will see notations F (full-term), P (premature), A (abortion), L (living child) Twin pregnancies= 1 pregnancy. So a woman who has had one set of twins= G1P2 apgar • Key assessment of newborn immediately after birth 5 components take at 1 and 5 minutes after birth based on 0,1, or 2, total score is 0-10, five minute score of 8+ move on to full exam • 1 minute score 8-10 normal, 5-7 some nervous system depression 0-4 severe depression requiring immediate resuscitation • 5 minute score 8-10 normal, 0-7 high risk for subsequent central nervous system and other organ dysfunction APGAR Clinical sign 0 1 2 Heart rate absent <100 >100 Respiratory effort Absent Slow and irregular Good, strong Muscle tone Flaccid Some flexion of arms and legs Active movement Reflex irritability No response Grimace Crying vigorously, sneeze or cough color Blue/pale Pink body, blue extremities Pink all over



![Common learning issues [Fall OMS I exam 1 2012].](http://s3.studylib.net/store/data/009436655_1-8a428dfd19e37e03ac0238fcf3b28e2d-300x300.png)