Chapter 18: Blood
advertisement

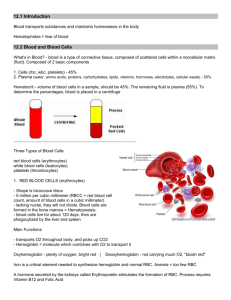
Chapter 18: Blood I. Functions and Properties Involved in respiration, nutrition, waste elimination, thermoregulation, immune defense, water and pH balance, and communication. 4-6L/ adult. Consists of plasma and formed elements (cells and platelets). Hematocrit separates RBCs from plasma, with buffy coat between. Normally, RBCs ~ 45%. Properties include: viscosity – 4.5 – 5.5X that of water; osmolarity regulates fluid and electrolyte balance based on osmosis. Colloid osmotic pressure especially crucial – created by proteins. When pathologically low, e.g. kwashiorkor (starvation), BP drops. II. Plasma With proteins removed = serum. (A) Proteins – for clotting, defense and transport. -1- albumins: smallest and most abundant. -2- globulins: alpha, beta and gamma. -3- fibrinogen: precursor of fibrin, for clotting. Most from liver; gamma globulins (antibodies) from plasma cells. (B) Nonprotein Nitrogenous Substances Amino acids and nitrogenous wastes, e.g. urea. (C) Nutrients: glucose, amino acids, fats, lipids, vitamins, minerals…. (D) Gases: O2, CO2, N2 (E) Electrolytes: Na+ most important. III. Blood Cell Formation = Hematopoiesis First from yolk sac, its stem cells migrate to marrow, spleen, liver, thymus. After infancy, myeloid hematopoiesis in red marrow (all formed elements) and lymphoid hematopoiesis in lymphoid tissues and elsewhere (only lymphocytes). 7 (A) RBC Production = erythropoiesis. 2.5 million cells/ second! Stimulated by hormone erythropoietin (EPO). Reticulocytes enter bloodstream, lose ER to mature into RBCs. RBC count maintained homeostatically. Stimulated by hypoxemia (low blood O2). Requires iron, which is selectively absorbed and transported. Also required: Vitamin B12, folic acid, Vitamin C and copper. (B) WBC Production = leukopoiesis. B progenitors; T progenitors; granulocyte-macrophage colony-forming units (for granulocytes & monocytes). These cells have receptors for CSFs (colony stimulating factors. (C) Platelet Production = thrombopoiesis. Stimulated by hormone thrombopoietin. Megakarycytes produced by DNA replication without cell divisions. Break into platelets. IV. Erythrocytes = Red Blood Cells (RBCs) (A) Form and Function Anucleate biconcave discs. Shape enhances surface area to volume ratio. Transport O2 and some CO2. Plasma membranes with glycoproteins and glycolipids which determine blood type. No organelles, depend upon anaerobic fermentation. Cytoplasm is 1/3 hemoglobin (Hb) which carries gases, enzyme carbonic anhydrase (which creates carbonic acid from water and CO2). (B) Hemoglobin 280 million molecules/ RBC! Each with four globin chains, two alpha & two beta, each has a heme (Fe) group to bind O2. CO2 binds to globin. Adult and fetal Hb (binds O2 more tightly). (C) Quantities clinically important. -1- hematocrit: 42-52% in men; 37-48% in women. -2- hemoglobin: 13-18 g/dL in men, 12-16 in women. -3- RBC count: 4.6-6.2 million/ microliter in men, 4.2-5.4 in women. Gender differences due to androgens, menstrual losses, relationship to body fat. (D) Death and Disposal RBC lifespan no more than 120 days. Membranes become fragile, many die in spleen (narrow channels). Hemolysis releases Hb. Globin provides amino acids, Fe recycled from heme, remainder creates bile pigments biliverdin, then bilirubin. Urobilinogen from bilirubin in small intestine (responsible for fecal brown). Urochrome from Hb for yellow urine. High blood bilirubin causes jaundice. 8 (E) RBC Disorders -1- polycythemia = elevated hematocrit. Increases blood viscicity and BP. Primary (polycythemia vera) due to cancer; secondary due to dehydration, hypoxemia (common in long-term smokers). -2- anemias (low hematocrit +/or Hb) result from three causes: a. inadequate hematopoiesis or Hb formation. Iron or vitamin deficiency, lack of intrinsic factor (pernicious anemia), old age, destruction of myeloid tissue (hypoplastic and aplastic anemias). b. hemorrhagic c. hemolytic: toxins, drugs, genetically malformed HB (thalassemia, Sickle Cell disease). V. Blood Types Based on antigens = agglutinogens on RBC surfaces. Recognized by antibodies = agglutinins, created in response to foreign agglutinogens. (A) ABO Group A and B gene alleles add sugars to glycolipids on membranes. Transfusion reaction: agglutination between agglutinins and foreign RBCs. Can be fatal. (B) Rh Group C, D, E exist but D most important clinically. Antibodies not present until sensitization in Rh- blood. HDN (hemolytic disease of the newborn) = erythroblastosis fetalis results from Rh antibodies passing placenta. Sensitization prevented with Rhogam injections. (C) Other groups – many. Rarely cause incompatibilities, used for paternity testing. VI. Leukocytes = White Blood Cells Classified, for convenience, based on appearance when stained. (A) Types -1- Granulocytes have obvious granules in cytoplasm: a. neutrophils- mostly phagocytic. b. eosinophils- fight parasitic worms. c. basophils: secrete histamine (inflammation) & heparin (blood thinner) 9 -2- Agranulocytes: a. lymphocytes: for immunity b. monocytes: become macrophages (B) Abnormal Counts Normal = 5,000-10,000 WBCs/ microliter -1- leukopenia = deficiency. Heavy metal poisoning, radiation sickness, some viral infections. -2- leukocytosis (excessive). Infection, allergy, dehydration. Differential count used for more useful diagnosis. -3- leukemias cause extreme leukocytosis. a. myeloid (granulocytes) vs. lymphoid. b. acute vs. chronic. VII. Hemostasis (A) Platelets: secrete procoagulents, vasoconstrictors, form plugs, dissolve old clots, phagocytize bacteria, attract WBCs, secrete growth factors to maintain vessel linings. (B) Vascular Spasm (C) Platelet Plug Formation Attraction to exposed collagen, release chemicals to establish positive feedback loop. (D) Coagulation Last resort, potentially dangerous, carefully regulated. Ends with fibrin mesh. Extrinsic mechanism initiated by damaged blood vessels, much faster. Intrinsic mechanism begins in blood. Leads to reaction cascade, requires Ca++, various factors (enzymes). Ultimately, prothrombin becomes thrombin, fibrinogen becomes fibrin. Involves another positive feedback loop. Platelets retract the clot, damaged blood vessel repaired. Dissolution = fibrinolysis, done with plasmin (another + feedback). Coagulation prevented by platelet repulsion, dilution, anticoagulants (antithrombin, heparin). (E) Disorders -1- hemophiliac: sex linked recessive, lack of clotting factors. Painful hematomas. -2- thrombosis: thrombus becomes embolus when traveling, embolism when lodged. 10