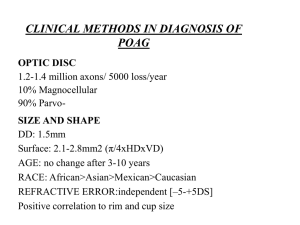
View PowerPoint Presentation. - Vision Research Coordinating Center
advertisement
Baseline topographic optic disc measurements are
associated with the development of POAG:
The CSLO Ancillary Study to the OHTS
Linda M Zangwill
Robert N Weinreb
Julie Beiser
Chuck C Berry
George A Cioffi
Anne L Coleman
Gary Trick
Jeffrey M Liebmann
James D. Brandt
Jody R Pitz-Seymour
Keri A Dirkes
Suzanne Vega
Michael A Kass
Mae O Gordon
and the OHTS CSLO Ancillary Study Group
Grant Support
NEI EY11158
NEI EY09341 and EY09307
and the National Center on
Minority Health and Health
Disparities,
Merck Research Laboratories
Unrestricted grants from
Research to Prevent Blindness
Financial Disclosures
Linda M Zangwill: (F) Heidelberg Engineering, Carl Zeiss Meditec
Robert N Weinreb: (F) Heidelberg Engineering, Carl Zeiss Meditec
Julie Beiser:
None
Chuck C Berry:
None
George A Cioffi:
None
Anne L Coleman: None
Gary Trick:
(C,R) Heidelberg Engineering
Jeffrey M Liebmann: (F,C) Heidelberg Engineering
James D. Brandt: None
Jody R Pitz-Seymour: None
Keri A Dirkes:
None
Suzanne Vega:
None
Michael A Kass:
None
Mae O Gordon:
None
CSLO Ancillary Study to the OHTS
Objectives:
• To determine the effectiveness of HRT to objectively and
quantitatively detect glaucomatous changes of the optic
disc in ocular hypertensive patients
• To describe racial differences in optic disc topography in
ocular hypertensive patients
• To assess the effect of ocular hypotensive treatment on
optic disc topography
• To determine whether optic disk topographic
measurements are an accurate predictor of glaucoma
CSLO Ancillary Study to the OHTS
Objectives:
• To determine the effectiveness of HRT to objectively and
quantitatively detect glaucomatous changes of the optic
disc in ocular hypertensive patients
• To describe racial differences in optic disc topography in
ocular hypertensive patients
• To assess the effect of ocular hypotensive treatment on
optic disc topography
• To determine whether optic disk topographic
measurements are an accurate predictor of glaucoma
CSLO Ancillary Study:
7of the 22 OHTS Study Centers Participating
•
Devers Eye Institute
– PI: Jack A. Cioffi, MD
– Coordinator: Kathryn Sherman
•
Scheie Eye Institute, U. of Pennsylvania
– PI: Jody R. Piltz-Seymour, MD
– Coordinator: Jane Anderson
•
Henry Ford Medical Center
– PI: Gary Trick, PhD
– Coordinator: Melanie Gutowski
•
University of California-Davis,
– PI: James D. Brandt, MD
– Coordinators: Ingrid Clark, Vickie Jaicheum
•
Jules Stein Eye Institute, UCLA
– PI: Anne L. Coleman, MD, PhD
– Coordinators: Tina Gonzales, Jackie
Sanguinet
•
•
New York Eye and Ear Infirmary
– PI: Jeffrey M. Liebmann, MD
– Coordinator: Jean Walker
University of California-San Diego
– PI: Robert N. Weinreb MD
–
Rigby Slight, MD
– Coordinators: Valerie Lepper, R.N.
Eva Kroneker, Rivak Hoffman
UCSD CSLO Reading Center
Robert N. Weinreb, MD, Primary Investigator
Linda M. Zangwill, PhD, Co-investigator
Chuck C Berry, PhD, Biostatistician
Keri L. Dirkes, MPH, Supervisor
Suzanne Vega, MPH, Coordinator
Amanda Policastro, Coordinator
Amanda R. Smith, MPH, Coordinator
Michelle Cambou, MPH , Coordinator
Chris Asvar , Coordinator
Isabela Niculae, MPH , Coordinator
Image Acquisition Methods
• Heidelberg Retina Tomograph (HRT1) images
acquired annually at dilated exam
• Both eyes: 10-degree field of view images
• OD: An additional 15 degree field of view
• 3 scans taken for each field of view
• K-values used to correct for magnification error
• Image series exported to CSLO Reading Center
• No processing at study centers
Standardized, centralized image
processing at CSLO Reading Center
(UC San Diego)
Quality Assurance
• Data Completeness
• Image Quality
• Only Certified Operators Acquire Images
Image Processing
• Creation of Mean Topographies
• Outlining of Disc Margin
• Exporting Data to OHTS Data Coordinating Center
CSLO OHTS Ancillary Study Participants
Demographic Characteristics
African-American Other
Total
Number of subjects* 75 (17%)
376 (83%)
451
Gender (% male)
29%
45%
42%
Mean Age (years)
54.4 ± 8.5
54.4 ± 9.4
54.4 ± 9.3
* With informed consent
CSLO Ancillary
Study to the OHTS
AJO 2004;137:219-227
Conclusions
• HRT topographic measurements are strongly correlated
with stereophotographic assessment of horizontal and
vertical cup disc ratios - even in OHTS participants with
normal appearing optic discs
• These results suggest that the HRT optic disc
measurements describe features that are reflected in
standardized assessment of cup-to-disk diameter ratios
from stereophotographs
CSLO Ancillary
Study to the OHTS
Arch Ophthalmol
2004;122:22-28
Conclusions
• African-Americans have significantly larger optic discs, cups, neuroretinal
rims and cup-to-disc ratios, and smaller rim-to-disc ratios than other OHTS
CSLO Ancillary Study participants
• After adjusting for the difference in disc area, none of the differences in optic
disc topography between African-Americans and other participants remained
statistically significant
• These results highlight the need to consider race and optic disc size when
evaluating the appearance of the optic disc in glaucoma
Racial Differences in Optic Disc Area
(both eyes)
p=<.0001
3
2
1
Other
(N=725)
African-American
(N=148)
Univariate Results:
Racial Differences in Optic Disc Topopgraphy
African Americans had larger:
• Disc area
• Cup area, volume and depth
• Rim area and volume
• RNFL cross-sectional area
African Americans had smaller:
• Rim to disc ratios
African American Eye
Caucasian Eye
Disc area:
2.2 mm2
Disc area:
1.9 mm2
Cup area:
0.9 mm2
Cup area:
0.4 mm2
Rim area:
1.4 mm2
Rim area:
1.5 mm2
Rim/Disc area:
0.6
Rim/Disc area:
0.8
Differences by Race
p<.001
p<.001
RimArea
AreaBRefG
2
1
2
1
0
African American
Race AA v Other
Other
Cup Area (mm2)
African American
Race AA v Other
Rim Area (mm2)
Other
Disc Size is Important
(e.g. Cup Area)
0.9
0.8
p<.001
0.7
0.6
0.5
African American
Other
0.4
0.3
0.2
0.1
0
All Discs (n=873)
Disc Size is Important
(e.g. Cup Area)
0.9
0.8
p=.7
p<.001
0.7
mm2
0.6
0.5
African American
Other
p=.7
0.4
0.3
0.2
0.1
0
All Discs (n=873)
Disc Area < Median
(n=439)
Disc Area > Median
(n=434)
Multivariate Results:
Racial Differences are no Longer Statistically Significant
(P-Values Adjusted for optic disc area, IOP, first study visit and age)
0.8
0.7
p=.39
0.6
mm2
0.5
African American
Other
0.4
p=.5
0.3
p=.49
0.2
0.1
0
Cup Area
Mean Cup Depth
Cup Volume
Objective:
• To determine whether baseline confocal
scanning laser ophthalmoscopy (CSLO) optic
disc topographic measurements are associated
with the development of primary open angle
glaucoma (POAG) in ocular hypertension.
Risk Factor versus Predictive Factor
• Epidemiologists differentiate between risk factors
and early damage
• Structural and functional indices of glaucoma may
be predictive factors but are not risk factors
Optic Disc Parameters Evaluated Included
•
•
•
•
•
•
•
•
•
•
•
•
Disc Area
Cup Area
Cup/Disc Area Ratio
Cup Volume
Cup Shape
Rim Area
Rim/Disc Area Ratio
Rim Volume
Cup Depth
RNFL Thickness
RNFL Cross-sectional Area
Mean Height Contour
Optic Disc Parameters Indices Included
(Outside normal limits or within normal limits compared to
normative data)
HRT Classification (linear discriminant function)
Moorfields Regression Analysis
• Global
• Six regions
• Overall (If any of the six regions or global is outside normal limits)
Moorfields Regression Analysis
Measured rim area compared to predicted age-corrected rim area,
adjusted for disc area
Classified as:
within normal limits (WNL)
outside normal limits (ONL)
Moorfields Regression Analyses
Outside Normal Limits
Moorfields Regression Analyses
Outside Normal Limits
Borderline: Considered WNL for this analysis
Sample HRT Data from OHTS CSLO
Ancillary Study Patient
OHTS POAG Endpoints
• 2 consecutive optic disc endpoints (Optic Disc Reading Center)
OR
• 3 consecutive visual field endpoints (Visual Field Reading Center)
Endpoint committee for final determination
Subjects Included in Analysis
• Good quality baseline images
– most baseline CSLO images obtained after randomization
– CSLO Ancillary Study was funded in July 1995 after OHTS began recruitment
– Added site later to increase African American enrollment
• If first CSLO image was acquired on or after the OHTS
examination with a suspicious photographic or visual field finding
later confirmed as POAG by the OHTS endpoint committee, that
eye was excluded from the analysis
Baseline Predictors of POAG Endpoints
CSLO Ancillary Study to the OHTS Subjects
439 with CSLO imaging
(n=874 eyes)
438 with CSLO before POAG
(n=865 eyes)
Subjects for
this study
{
36 Reached POAG
Endpoint
(n=41 eyes)
Images not acquired before
POAG (1 participant (OU) & 7
unilateral eyes)
432 Did not reach a
POAG Endpoint
(n=824 eyes)
POAG Endpoints in 41 eyes of 36 participants
• POAG initial suspicious dates before October 2003- confirmed and
entered into the database by February 9, 2004.
• 5 bilateral POAG, 31 unilateral POAG
– 9 (22%) eyes reached a visual field endpoint first
– 31 (76%) eyes reached an optic disc endpoint first
– 1 (2%) eye reached visual field and optic disc endpoint concurrently
CSLO OHTS Ancillary Study Participants
POAG (n=36)
Not POAG (n=402)
Mean Age (years)
57.5 ± 9.4
54.8 ± 9.1
Mean IOP (mm Hg)
25.1 + 2.8
25.0 + 2.3
Mean Visual Field PSD (dB)
1.95 + .20
1.90 + .21
Mean Photo based VCDR
.47 + .18
.38 + .19
Mean Corneal Thickness (µm) 554.3 + 37.4
577.0 + 37.0
Mean Follow-up (months)
79.5 + 20.8
% African Americans
48.4 + 25.2
14%
21%
Significant Baseline CSLO Measurements
Associated with the Development of POAG
from Multivariate Proportional Hazards Models
(Adjusting for age, IOP, PSD, CCT and history of heart disease, with medication status as a time dependent covariate)
Hazards Ratio (95% CI)
Mean Height Contour (per .1 mm greater)
2.7 (1.6, 4.5)
Mean Cup Depth (per .1 mm greater)
1.6 (1.1, 2.2)
Reference Plane Height (per .1 mm greater)
1.5 (1.0, 2.2)
Cup Area-to-Disc area (per .1 greater)
1.2 (1.0, 1.5)
Cup Volume below reference (per .1 mm3 greater)
1.2 (1.0, 1.4)
Rim Area (per .1 mm2 greater)
0.6 (0.4, 0.8)
Rim Volume (per .1 mm3 greater)
0.6 (0.5, 0.9)
Rim Area-to-Disc area (per .1 greater)
0.8 (0.6, 0.9)
Significant Baseline CSLO Indices
Associated with the Development of POAG
from Multivariate Proportional Hazards Models
(Adjusting for age, IOP, PSD, CCT and history of heart disease, with medication status as a time dependent covariate)
Hazards Ratio (95% CI)
(outside normal limits versus not)
HRT Classification (LDF)
2.5 (1.3, 4.9)
Moorfields Regression Analysis
Overall (Any region ONL)
2.4 (1.0, 5.6)
Global (Global values ONL)
3.4 (1.1, 10.0)
Temporal Inferior
5.8 (1.6, 21.0)
Nasal Inferior
4.2 (1.6, 10.9)
Temporal Superior
3.3 (0.98, 11.0)
Baseline CSLO measurements
Not Associated with the Development of POAG
from Multivariate Proportional Hazards Models
(Adjusting for age, IOP, PSD, CCT, history of heart disease, with medication status as a time dependent covariate)
Hazards Ratio (95% CI)
Disc area (per .4 mm2 greater)
0.9 (0.6, 1.3)
RNFL thickness (per .1mm greater)
0.6 (0.4, 1.2)
Cup Shape (per .1 greater)
1.0 (0.6, 1.7)
RNFL Cross Sectional area (per .3mm2 greater)
0.7 (0.5, 1.1)
Kaplan-Meier Survival Curves
Mean Height Contour
Rim Area
(above and below median values)
(above and below median values)
Moorfields Regression
Analysis Global
Summary of Results
• Baseline CSLO topographic optic disc measurements when
used alone or combined with central corneal thickness, IOP,
history of vascular disease are significantly associated with the
development of POAG among individuals with ocular
hypertension.
• Majority of eyes with CSLO classifications “outside normal
limits” at baseline did not develop POAG within the follow-up
period of this analysis
“Predictive accuracy” during follow-up period
(% of POAG and non-POAG correctly classified at baseline)
Not at
POAG
(n=402)
POAG
(n=36)
Sensitivity
Specificity
Negative
Predictive
Value
Positive
Predictive
Value
HRT
Classification
Outside
Normal
Limits
128
20
55%
68%
95%
14%
MRA Overall
Outside
Normal
Limits
61
10
28%
85%
93%
14%
MRA Global
Outside
Normal
Limits
14
5
14%
96%
93%
27%
MRA Temporal
Inferior
Outside
Normal
Limits
13
3
8%
97%
92%
19%
MRA nasal
Inferior
Outside
Normal
Limits
24
7
19%
94%
93%
23%
MRA
temporal
superior
Outside
Normal
Limits
6
4
11%
99%
93%
40%
“Predictive accuracy” during follow-up period
(% of POAG and non-POAG correctly classified at baseline)
Not at
POAG
(n=402)
POAG
(n=36)
Sensitivity
Specificity
Negative
Predictive
Value
Positive
Predictive
Value
HRT
Classification
Outside
Normal
Limits
128
20
55%
68%
95%
14%
MRA Overall
Outside
Normal
Limits
61
10
28%
85%
93%
14%
MRA Global
Outside
Normal
Limits
14
5
14%
96%
93%
27%
MRA Temporal
Inferior
Outside
Normal
Limits
13
3
8%
97%
92%
19%
MRA nasal
Inferior
Outside
Normal
Limits
24
7
19%
94%
93%
23%
MRA
temporal
superior
Outside
Normal
Limits
6
4
11%
99%
93%
40%
“Predictive accuracy” during follow-up period
(% of POAG and non-POAG correctly classified at baseline)
Not at
POAG
(n=402)
POAG
(n=36)
Sensitivity
Specificity
Negative
Predictive
Value
Positive
Predictive
Value
HRT
Classification
Outside
Normal
Limits
128
20
55%
68%
95%
14%
MRA Overall
Outside
Normal
Limits
61
10
28%
85%
93%
14%
MRA Global
Outside
Normal
Limits
14
5
14%
96%
93%
27%
MRA Temporal
Inferior
Outside
Normal
Limits
13
3
8%
97%
92%
19%
MRA nasal
Inferior
Outside
Normal
Limits
24
7
19%
94%
93%
23%
MRA
temporal
superior
Outside
Normal
Limits
6
4
11%
99%
93%
40%
Need for Longer Follow-up
to better evaluate predictive accuracy
• Majority of eyes with outside normal limit values did not develop
POAG during current follow-up period.
• Important to determine whether participants with POAG
endpoints and CSLO indices within normal limits at baseline, had
CSLO measurements outside normal limits during their later
follow-up examinations.
This Study Did Not:
• Determine whether the OHTS prediction model that includes
baseline CSLO measurements is improved over one that
includes baseline stereophotograph cup-disc ratio measurements
– additional POAG endpoints are needed
• Determine whether CSLO is a better predictive tool than other
instruments, such as the GDX or the OCT
• Recommend specific CSLO parameters
Thank You
UCSD Hamilton Glaucoma Center
Mean Height Contour
• Displays height values moving around optic disc, in order:
Temporal -> Superior -> Nasal -> Inferior -> Temporal
Temp
Superior
Nasal
Inferior
Normal Eye
Double hump pattern
Temp
Temp
Superior
Nasal
Inferior
Temp
Glaucoma Eye
Inferior RNFL Loss
Mean Height Contour
• Y axis goes from negative to positive values, moving
from inside the eye outward toward the back of the retina
Inside Eye
- (negative values)
0 (zero)
Average height in
parapapillary region
+ (positive values)
Back of retina
Sample HRT Data from OHTS CSLO
Ancillary Study Patient
HRT Classification