outline6601 - American Academy of Optometry
advertisement

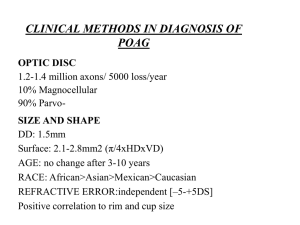
Revisiting the Structure-Function Relationship in Glaucoma: Implications from Recent Clinical Trials. Chair: John G. Flanagan PhD, MCOptom, FAAO Professor, School of Optometry, University of Waterloo and Dept. of Ophthalmology and Vision Sciences, University of Toronto, Ontario, Canada. Pamela Sample PhD Professor, Hamilton Glaucoma Centre Department of Ophthalmology University of California, San Diego Linda Zangwill PhD Professor, Hamilton Glaucoma Centre Department of Ophthalmology University of California, San Diego Chris Johnson PhD, Professor, Discoveries in Sight, Devers Eye Institute, Portland Abstract This course will review the current understanding of the structure-function relationship as it relates to glaucoma, and reviews important information from recent and ongoing clinical trials that may force us to modify current perceptions. Included will be a discussion of the OHTs ancillary studies involving both Short-Wavelength Automated Perimetry and the Heidelberg Retina Tomograph. In addition there will be discussion of the African Americans with Glaucoma (AAG) study. Learning Objectives 1. Review current understanding of the structure-function relationship in glaucoma 2. Understand the implications of the OHTs ancillary study incorporating SWAP 3. Understand the implications of the OHTs ancillary study incorporating HRT 4. Review the results of the AAG study Outline 1. Short Wavelength Automated Perimetry (SWAP) in the Ocular Hypertension Treatment Study (OHTS) 1.1 Purpose: i. To determine the percentage of SWAP deficits for participants enrolled in the OHTS ii. To evaluate the relationship between SWAP results and other baseline clinical characteristics and iii. To assess the predictive value of initial SWAP deficits. 1.2 Methods: All participants had normal and reliable standard Humphrey visual fields at baseline. SWAP testing was performed in 397 eyes of 199 participants enrolled in the OHTS SWAP ancillary study at nine participating clinical centers, using the previously-determined 1 optimal testing conditions for SWAP. A standardized protocol was used for all clinical centers and all technicians were required to complete a certification process prior to testing participants. 1.3 Results: i. The prevalence of SWAP abnormalities at the initial test, for the Glaucoma Hemifield Test (GHT) analysis was 20.9% when there was no detectable visual field deficit for standard (white-on-white) automated perimetry. ii. There was a higher prevalence of SWAP abnormalities in African Americans (32.6%) as compared to white, not Hispanics (19.2%) (p<.026). ii. There was a higher prevalence of SWAP abnormalities for participants with a high school education or less (31.6%) as compared to participants with 1 or more years of college (19.1%) (p<.016). iv. No other significant associations were found for the prevalence of SWAP deficits as a function of age, gender, IOP, diabetes, high blood pressure, low blood pressure, family history of glaucoma or migraine. v. SWAP abnormalities at the initial test were not significantly associated with prediction of a POAG endpoint. 1.4 Conclusions: i. Approximately 20% of OHTS participants enrolled in the SWAP ancillary study demonstrated abnormalities on the SWAP GHT analysis, despite having normal and reliable visual fields on standard automated perimetry. ii. Our results suggest that the prevalence of SWAP deficits is higher in African Americans and in participants with a lower education level. ii. Initial SWAP deficits were not significantly associated with the development of a Primary Open Angle Glaucoma (POAG) endpoint, although further follow-up may provide further information in this regard. 2. The Confocal Scanning Laser Ophthalmoscopy (CSLO) Ancillary Study to the OHTS 2.1 Study Design and Baseline Factors. 2.1.1 Purpose: To describe the study design of the CSLO Ancillary Study to the OHTS and to examine the associations between optic disk topography, and baseline demographic, clinical, and ocular factors at study entry. 2.1.2 Methods: Associations between Heidleberg Retina Tomograph (HRT) topographic optic disk measurements and IOP, baseline photographic estimates of horizontal and vertical cupto-disk diameter ratios by the OHTS Optic Disk Reading Center, baseline visual field indices, and demographic and clinical factors were assessed using linear mixed effects models. 2.1.3 Results: 439 participants with good quality images were included. No associations between HRT topographic optic disk measurements and diabetes, systemic hypertension, cardiovascular disease, IOP, or visual function were found. The HRT topographic optic disk measurements were associated with baseline stereophotographic estimates of horizontal and vertical cup-to-disk diameter ratios. The strongest associations were found between stereophotographic assessment of horizontal and vertical cup-to-disk diameter ratios, and HRT cup-to-disk area ratio (r = .85 and .84, respectively), rim-to-disk area ratio (r = -.85 and -84, respectively), mean cup depth (r = .84 and .83, respectively), and cup area (r = .83 and .80, respectively). After adjusting for optic disk area, all HRT topographic optic disk measurements remained associated with stereophotographic assessment of horizontal and vertical cup-to-disk diameter ratios. 2.1.4 Conclusions: The CSLO ancillary study to the OHTS is the first multicenter clinical trial to use CSLO imaging to monitor changes in the optic disk. At study entry, HRT topographic measurements corresponded well with both horizontal and vertical stereophotographic-based estimates of cup-to-disk diameter ratio in OHTS participants. 2 2.2 Racial Differences in Optic Disc Topography 2.2.1 Purpose: To examine racial differences in optic disc topography among ocular hypertensive participants in the Ocular Hypertension Treatment Study. 2.2.2 Methods: 439 participants with good-quality baseline CSLO images obtained using a HRT were included. Differences in HRT topographic optic disc parameter measurements by self-identified race were assessed using a mixed-effects linear model to control for confounders and for the use of both eyes in the model. 2.2.3 Results: By self-attribution, 74 (17%) of the 439 participants were of African origin, 329 (75%) were white, 24 (5%) were Hispanic, and 12 (3%) were Native American, Native Alaskan, Asian, Pacific Islander, or unknown. The African American participants had statistically significantly (P<.001) larger mean (SD) optic disc areas than the other participants, 2.17 (0.41) mm2 vs. 1.87 (0.38) mm2, respectively. African American participants had a larger cup area, cup volume, cup depth, neuroretinal rim area, rim volume, and smaller rim–to-disc area ratios than the other participants. No difference between African American and the other participants was found for cup shape and retinal nerve fiber layer thickness. After controlling for optic disc area, none of the differences between African American and the other participants found in the univariate analysis remained statistically significant (P>.10). 2.2.4 Conclusions: This study found that differences in topographic optic disc parameters between African Americans with ocular hypertension and other racial groups are largely explained by the larger optic disc area in the African Americans. These results highlight the need to consider race and optic disc size when evaluating the appearance of the optic disc in glaucoma. 2.3 Baseline Topographic Optic Disc Measurements are Associated with the Development of POAG 2.3.1 Purpose: To determine whether baseline CSLO optic disc topographic measurements are associated the development of POAG in ocular hypertension. 2.3.2 Methods: 865 eyes from 438 participants with good quality baseline CSLO images were included. Each baseline CSLO parameter was assessed in univariate and multivariate proportional hazards models to determine its association with the development of POAG (a confirmed visual field abnormality or a confirmed clinically significant confirmed optic disc deterioration attributed to glaucoma.) 2.3.3 Results: 41 eyes from 36 CSLO Ancillary Study participants developed POAG. 31 (77%) eyes reached an optic disc endpoint only, 9 (22%) eyes reached a visual field endpoint only, and 1 eye reached both types of endpoints concurrently. Several baseline CSLO measurements were significantly associated with the development of POAG in both univariate and multivariate analysis including larger cup-to-disc area ratio, mean cup depth, mean height contour, cup volume, reference plane height, and smaller rim area, rim area to disc area, and rim volume. In addition, classification as “outside normal limits” by the HRT “Classification” and the Moorfields Regression Analysis (MRA) (overall, global, temporal inferior, nasal inferior and superior temporal regions) classifications were significantly associated with the development of POAG. However, within the follow-up period of this analysis, the predictive value of a positive test was low for many CSLO indices, ranging from 14% (HRT Classification and MRA Overall) to 27% for MRA Global. 2.3.4 Conclusion: Several baseline CSLO measurements alone or when combined with baseline clinical and demographic factors were significantly associated with the development of POAG among OHTS participants. Longer follow-up is required to evaluate the true predictive accuracy of CSLO measures. 3 3. Comparison of New Diagnostic Techniques in Black and White Participants. 3.1 Background: Glaucoma is 5 times more likely to occur in Blacks than Whites, and is the leading cause of irreversible blindness in Blacks. Little is known about whether new diagnostic tests including vision function specific tests and optic disc and retinal nerve fiber layer imaging can improve our ability to detect and monitor glaucoma in the Black population. 3.2 Purpose: To compare differences in visual function tests and measures of optic nerve structure in normal, ocular hypertensive, and glaucomatous Black and White participants, to determine whether function specific perimetry tests show improved diagnosis in Blacks as they do in Whites, and to compare the rate and patterns of progression of glaucomatous damage in the two racial groups. 3.3 Methods: 125 normal and 275 Black participants with glaucoma. Black participants will be recruited primarily from New York Eye and Ear Infirmary and the University of Alabama Glaucoma Service. White participants are recruited under separate funding at UC San Diego. UC San Diego serves as a Reading Center for data processing, quality control and analysis for this study. The glaucomatous eyes will be followed with annual testing for 5 years. Visual fields will include standard clinical perimetry, and two function-specific tests, SWAP and Frequency Doubling Perimetry. Optic nerve structure will be qualitatively evaluated with stereoscopic fundus photography and quantitatively using the HRT and Optical Coherence Tomograph. Comparisons between Blacks and Whites will be made on each test and between the measures of function and structure. 3.4 Results: Preliminary results will be presented. 3.5 Significance: A greater understanding of the importance of race for development and progression of glaucoma will result leading to more precise endpoints for future clinical trials with this at-risk minority population. 4