optic disc cup
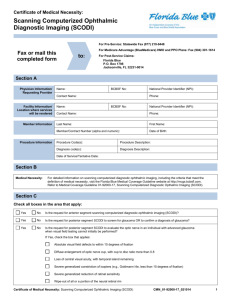
advertisement
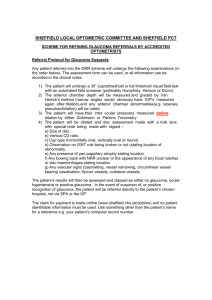
CLINICAL METHODS IN DIAGNOSIS OF POAG OPTIC DISC 1.2-1.4 million axons/ 5000 loss/year 10% Magnocellular 90% ParvoSIZE AND SHAPE DD: 1.5mm Surface: 2.1-2.8mm2 (π/4xHDxVD) AGE: no change after 3-10 years RACE: African>Asian>Mexican>Caucasian REFRACTIVE ERROR:independent [–5-+5DS] Positive correlation to rim and cup size Vertically oval (VDmax>HDmin by 10%) Abnoral shape or tilted: corneal astigmatism- amblyopia RIM SIZE AND SHAPE Related to disc size (+) ISNT rule (vert. oval disc/ Horizontal oval cup) Positive correlation to ret. arteriole diameter IT-ST-HT- IN-SN (predilection, mainly DIFFUSE loss) ST: sharp border cup-rim IT: some sloping (but NFL normal) Pallor: ? Non-glaucomatous (increased cup size) OPTIC DISC CUP Increases with disc size Horizontally oval Depth: with disc size (deepest: JPOAG, Shallowest: high myopic type of POAG)- negative correlation to PPA CD RATIO H>V hence H/V>1.0 but in early to medium G <1.0 Normal range:0.0-0.9 Independent of optic media magnification HCD/VCD: independent of cup and disc size RNFL Ganglion cells axons+astrocytes+ Muller cell processes Visibility: unevenly distributed/ with age IT>ST>SN>IN>S>I>HT>HN Correlates with rim thickness, retinal artery caliber and foveolar location Sandwich arrangment Red –free/ wide beam Achromatic white light Clinical examination Direct Indirect Slit lamp ophthalmoscope ophthalmoscope •Red-free •No stereo- •Young children •Uncooperative •High myopes •Opacities 90D 78D 60D FCL DISC CHANGES IN POAG GENERALIZED • Large cup • Cup asymmetry • Progressive in cup size • Saucerisation FOCAL • Notching •Vertical elongation •Cupping of rim margin •Regional pallor •Splinter haemorrhage( specificity, early-med advanced, IT-ST, Progression, NTG) LESS SPECIFIC •Exposed lamina cribrosa •Nasal displacement •Baring of circumlinear vessels/ constriction of arterioles •PP crescent (spatial correlation with NRR loss) •Shunt vessels of optic disc (advanced stage) RNFL CHANGES •Focal defects wedge shaped (disc border-broad base to temporal raphe) 20%, always pathologic but not pathognomonic v: from early to medium advanced G and very advanced Associated with notching, haem, PPA in that sector/NTG 50% loss of thickness: visible • Diffuse (commoner, more difficult to see) Sequence of sectors regarding RNFL visibility Retinal vessels( clearer- sharper) RECORDING OF FINDINGS 1. CD ratio: poor description 2. NRR: colour, contour, width 3. Diagram 4. PHOTO (stereo+ magnification) AQUEOUS HUMOUR DYNAMICS GOLDMAN EQUATION: IOP= (F/C)+P PRODUCTION Rate: 2-3 μl/min (1% turnover/min) Pigmented+non-pigmented cells •Active transport (70%) •Ultrafiltration (20%) •Osmosis (10%) OUTFLOW 0.22-0.28 μl/min /mmHg •Trabecular (90%) •Uveoscleral (10%) EPISCLERAL VENOUS PRESSURE 10mmHg IOP Mean 16mmHg SD:3mmHg (10-22mmHg) Non Gaussian distribution, skew to R (>40y) •Diurnal variation/ Seasonal (W>S) •Heart beat/ respiration •Exercise/ Posture •Fluid intake •Medication (systemic, topical, alcohol, caffeine, cannabis)) •Age •F>M after 40y •Genetically influenced IOP MEASUREMENT 1. Applanation tonometry (Imbert-fick: P= F/A) Goldmann, Perkins Airpuff (overestimate) Tonopen (scar, oedema) 2. Indentation: Schiotz 3. Digital pressure SOURCES OF ERROR • Squeezing •Valsalva •Pressure on globe •Tight collars •Calibration •EOM force to restricted globe • FL: IOP and vice versa • corneal astigmatism • corneal oedema •scar •CL •Central corneal thickness (LASIK, PRK) • Post scleral buckling