Lessons from the Ocular Hypertension Treatment Study (OHTS)
advertisement

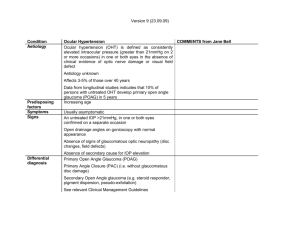
1 Practical Implications of the The Ocular Hypertension Treatment Study (OHTS) G. Richard Bennett, M.S., O.D., F.A.A.O. Professor and Chief, The Glaucoma Service The Eye Institute of Salus University The Ocular Hypertension Treatment Study Group (OHTS) National Eye Institute, National Center for Minority Health and Health Disparities, NIH grants EY09307, EY09341, EY02687, Unrestricted Grant from Research to Prevent Blindness, Merck Research Laboratories and Pfizer, Inc. August 2010 National Eye Institute Clinical Trials Across the Ongoing trials Spectrum of Glaucoma Interim results Completed trials CIGTS OHTS Ocular Hypertension Early Glaucoma AGIS GLT EMGT Brandt JD. Large prospective glaucoma trials: Where are we now? Presented at: American Glaucoma Society Annual Meeting 2002. March 2, 2002; San Juan, Puerto Rico. Advanced Glaucoma FFSS 2 Ocular Hypertension A common condition What to do with these patients? How often should they be examined? Is preventative treatment effective? Who should be treated? August 2010 3 Ocular Hypertension 1. 2. 3. 4. 5. IOP > 21 mmHg No detectable visual field loss No detectable optic disc or nerve fiber layer damage Open angles No ocular or systemic cause of increased IOP August 2010 4 Ocular Hypertension 119 million people in US over age 40 (Census 2000) 4%-8% of people in the United States over age 40 (4.8 – 9.5 million people) have OHT The number of affected people will increase with the aging of the population Managing this large group of people is associated with substantial costs for examinations, tests and treatment August 2010 5 Ocular Hypertension Elevated IOP is a leading risk factor for development of POAG Only modifiable risk factor for POAG Patients can lose a substantial proportion of their nerve fiber layer before POAG is detected by standard clinical tests Quigley HA, et al. Arch Ophthal 1981;99:635 August 2010 6 Does Treatment of Ocular Hypertension Prevent POAG? Protective Investigator Protective Graham no Becker & Morton yes Norskov no Shin et al. yes Levine no Kitizawa yes David et al. no Epstein et al. yes Chisholm no Kass et al. yes Schulzer et al. no Heijl et al. no Limitations of previous studies: Kamal et al. no Miglior et al. no Investigator Varying endpoints Limited treatment regimens Small sample size August 2010 7 Ocular Hypertension Treatment Study (OHTS) Primary Goals Evaluate the safety and efficacy of topical ocular hypotensive medication in delaying or preventing the development of POAG in individuals with elevated IOP Identify baseline demographic and clinical factors that predict which participants will develop POAG Kass, et al. 2002 8 The OHTS Entry Criteria Age 40 - 80 Normal visual fields Humphrey 30-2 Normal optic discs Untreated IOP: 24 to 32 mm Hg in one eye 21 to 32 mm Hg in fellow eye Kass, et al. 2002 9 OHTS Phase 1 Begins February 28, 1994 Eligibility Criteria • Eligible untreated IOPs on 2 visits • 2 sets of normal & reliable HVFs per VFRC • Optic discs judged normal by ODRC Randomization Medication Topical treatment to lower IOP 20% and IOP < 24 mm Hg Adjust therapy if target not met Observation No topical treatment to lower IOP Monitoring Humphrey 30-2 q6 months Stereoscopic disc photos annually Reproducible Abnormality 3 consecutive visual fields and/or 2 consecutive sets of optic disc photographs as determined by masked readers at ODRC or VFRC POAG Visual field and/or optic disc changes attributed to POAG by masked Endpoint Committee Kass, et al. 2002 10 Baseline Characteristics Baseline Characteristics N=1,636 Age (mean ±SD) 55.4 ±9.6 SD White 70% African American 25% Hispanic 4% Other 1% Sex Male 43% Female 57% IOP, mm Hg 24.9 ±2.7 SD Vertical CD 0.39 ±0.2 SD CCT 572 ±38.4 SD Kass, et al. 2002 11 OHTS Phase 1: Primary POAG Endpoints Log rank P-value<0.001, hazard ratio 0.40, 95% confidence interval (0.27, 0.59) Cumulative proportion POAG at 60 months, 9.5% in OBS and 4.4% in MEDS Proportion of participants developing POAG 0.4 Medication Observation 0.3 0.2 0.1 0.0 6 12 18 24 30 36 42 48 54 60 66 72 78 84 Months Kass, et al. 2002 12 OHTS Phase 1: First Optic Disc POAG Endpoint Log rank P-value<.0001, hazard ratio 0.36, 95% confidence interval (0.23, 0.56) Cumulative proportion POAG at 60 months, 7.7% in OBS and 3.2% in MEDS Proportion of participants developing POAG 0.4 Medication Observation 0.3 0.2 0.1 0.0 6 12 18 24 30 36 42 48 54 60 66 72 78 84 Months Kass, et al. 2002 13 OHTS Phase 1: First Visual Field POAG Endpoint Log rank P-value=0.002, hazard ratio 0.45, 95% confidence interval (0.26, 0.76) Cumulative proportion POAG at 60 months, 5.2% in OBS and 2.1% in MEDS Proportion of participants developing POAG 0.4 Medication Observation 0.3 0.2 0.1 0.0 6 12 18 24 30 36 42 48 54 60 66 72 78 84 Months Kass, et al. 2002 15 OHTS Phase 1: Cumulative Proportion Developing POAG by Race African Americans Others 12.7% POAG endpoints in observation group 10.2% POAG endpoints in observation group 6.9% POAG endpoints in medication group 3.6% POAG endpoints in medication group Hazard Ratio 0.54 Hazard Ratio 0.34 P value 0.26 Kass, et al. 2002 17 OHTS Phase 1: Summary Medication produced about a 20% reduction in IOP. Medication reduced incidence of POAG in OHT participants by more than 50% at 5 years from 9.5% in the Observation Group to 4.4% in the Medication Group. Little evidence of safety concerns. Kass, et. al. 2002 18 OHTS Phase 2: Rationale OHTS Phase 1 provides proof of concept: medication reduces the incidence of POAG. OHTS Phase 1 does not indicate when medication should begin. OHTS Phase 1 does not indicate if all OHT patients should receive early medication. Is there a penalty for delaying medication in OHT? August 2010 19 OHTS Phase 2 Begins 06/01/2002 Medication Group Observation Group N = 694 N = 672 Medication is continued in the Medication group Medication is Initiated in the Observation group August 2010 20 OHTS Phase 2: Methods After 7.5 years of observation, participants originally randomized to observation group start medication. This creates: Delayed treatment group Observation group followed for 7.5 years then treated for 5.5 years Early treatment group Medication group treated for median of 13 years from the beginning Compare incidence of POAG at 13.0 years Kass, et al. 2010 21 Median IOP thru 13 Yrs by Randomization Group Medication 30 Observation 28 mm Hg 26 24 22 20 18 16 14 0 12 24 36 48 60 72 84 96 108 120 132 144 156 Months Kass, et al. 2010 22 Kass, et al. 2010 OHTS: Cumulative Incidence of POAG by Randomization Group 24 Complementary log log at 13 years, p=0.009 Cumulative proportion POAG at 13 years, 22% in OBS and 16% in MEDS Proportion of participants developing POAG 0.4 Medication Observation 0.3 0.2 0.1 0.0 6 18 30 42 54 66 78 90 102 114 126 138 150 162 Months Kass, et al. 2010 25 Median Time to Develop POAG Observation Group 6.0 years Medication Group 8.7 years P ≤ .001 Kass, et al. 2010 26 OHTS Phase 1 Incidence of POAG is nearly 60% lower in the Medication Group Hazard ratio for medication group at 60 months 0.40 (0.27-0.59); P ≤ .001 Kass, et al. 2002 OHTS Phase 2 Incidence of POAG is not different between observation and medication groups Hazard Ratio for medication group 1.06 (0.74-1.50); P = .77 Kass, et al. 2010 29 Cumulative Proportion Developing POAG at 13 Yrs. by Race African Americans 0.28 (0.23-0.33) Others (0.14-0.19) 0.16 P = .001 Kass, et al. 2010 OHTS: Cumulative Proportion POAG at 13 yrs by Race 30 Other Races: 19.5% OBS and 13% MEDS African Americans: 29% OBS and 26% MEDS Other race/Med Other race/Obs. African American/ Med African American/Obs Proportion of participants developing POAG 0.4 0.3 0.2 0.1 0.0 6 18 30 42 54 66 78 90 102 114 126 138 150 162 Months Kass, et al. 2010 31 Self-identified race not significant predictor of POAG in a multivariate model. Race not significant when central corneal thickness and baseline cup-disc ratio included. Kass, et al. 2010 32 Baseline Predictive Factors for the Development of POAG Age IOP CCT Vertical C/D Ratio PSD OHTS/EGPS,2007 Multivariate Hazard Ratios for Predictors of POAG 33 OHTS Observation group, EGPS Placebo group, DIGS and OHTS/EGPS Age Decade OHTS EGPS DIGS OHTS-EGPS IOP (mm Hg) OHTS EGPS DIGS OHTS-EGPS CCT (40 µm decrease) OHTS EGPS DIGS OHTS-EGPS PSD (per 0.2 dB increase) OHTS EGPS DIGS OHTS-EGPS Vertical CD ratio OHTS EGPS DIGS OHTS-EGPS 0.0 0.5 1.0 1.5 2.0 2.5 3.0 3.5 OHTS/EGPS 2007 34 Accuracy of Prediction Models for POAG compared to Framingham Heart Study* Prediction Models C-statistic Framingham Heart Study prediction model applied to different studies 0.63 - 0.83 D’Agostino et. al. JAMA, 2001. OHTS observation group 0.76 OHTS/EGPS Ophthal, 2007. EGPS placebo group 0.73 OHTS/EGPS Ophthal, 2007. Pooled OHTS EGPS sample 0.74 OHTS/EGPS Ophthal, 2007. August 2010 35 Using the OHTS/EGPS Prediction Model for the Development of POAG Available on web free of charge http://ohts.wustl.edu/risk OHTS/EGPS, 2007 36 August 2010 37 Baseline Risk of Developing POAG by Race At each level of risk. the percent of African Americans and “Other” participants developing POAG is similar. Percent of Participants Developing POAG to study end on top of bars Others African American Percent of participant by race 40 35 30 25 20 15 10 5 0 <5% >5% - 10% >10% - 15% >15% - 20% >20% - 25% Baseline Predicted 5 year Risk >25% Kass, et al. 2010 38 Cumulative Incidence of POAG in the “Lowest”, “Middle” and “Highest” Tertiles of Baseline Risk for Developing POAG* Lowest <6% Medication Observation Observation Medication 0.5 0.4 0.3 0.2 0.1 0.4 0.3 0.2 0.1 0.0 0.0 6 18 30 42 54 66 78 90 102 114 126 138 150 162 Months Observation 0.5 Proportion of participants developing POAG Proportion of participants developing POAG 0.5 Proportion of participants developing POAG (n=484) (n=482) (n=482) Medication Highest >13% Middle 6% - 13% 6 18 30 42 54 66 78 90 102 114 126 138 150 162 Months 0.4 0.3 0.2 0.1 0.0 6 18 30 42 54 66 78 90 102 114 126 138 150 162 Months * Risk estimated by OHTS/EGPS risk calculator, 2007 Kass, et al. 2010 39 Cumulative 13 year Incidence of POAG for “Lowest”, “Middle” and “Highest” Baseline Risk Group* Medication group Observation group P-Value Lowest Risk < 6% (n=482) Middle Risk 6% - 13% (n=482) Highest Risk 13% (n=484) 7% 14% 28% 4% - 11% 9% - 18% 22% - 34% 8% 19% 40% 4% - 11% 14% - 25% 33% - 46% 0.81 0.11 0.009 * OHTS/EGPS Risk Calculator, 2007 Kass, et al. 2010 40 Mean PSD Before and After POAG Patients who developed POAG had worse PSD at entry and worsened over time Patients who did not develop POAG did not change 4.75 Non-POAG OBS, n=494 Non-POAG MEDS, n=558 4.50 POAG OBS, n=164 POAG MEDS, n=117 4.25 4.00 Time of POAG diagnosis is time “0” Time before POAG is “-” Time after POAG is “+” 3.50 PSD Median time to POAG of 7 years is “0” for participants who do not develop POAG. 3.75 3.25 3.00 2.75 2.50 2.25 2.00 1.75 -7 -6 -5 -4 -3 -2 -1 0 1 2 3 Median Follow-Up or Years since POAG 4 5 6 7 Kass, et al. 2010 42 Safety No safety differences between randomization groups Mortality Adverse events Glaucoma Symptom Scale NEI VFQ MOS-SF 36 Kass, et. al. 2010 43 Delaying Treatment of OHT 1. Increased cumulative incidence of POAG at 13 years (22% vs.16%) 2. More eyes with structural and functional damage (8% vs. 5%) 3. More participants with bilateral disease (6% vs. 4%) Kass, et. al. 2010 44 Delaying Treatment of OHT … 4. Shorter time to develop POAG (6.0 vs. 8.7 years) 5. Waiting does not have a large effect on MD and PSD (0.5db for PSD) within 5 years of developing POAG. Kass, et. al. 2010 DRANCE HEMORRHAGES Optic Disc Hemorrhages – observed in glaucoma – perhaps noticed particularly in NTG – linked to progression of disease not adequately controlled – An endpoint of glaucoma progression?? Drance Hemorrhages Glaucomatous Optic Disc Hemorrhages – characteristically in the axon bundles – therefore, splinter-shaped and superficial » crossing the disc boundary, or » over a peripapillary crescent or halo – or within the disc, not flame-shaped Drance Hemorrhage? OHTS DATA Data from the Ocular Hypertension Treatment Study (OHTS) used to see: – what makes disc hemorrhage likely? – how predictive are they of the future course (incident glaucoma) in OHT? Definition of “Glaucomatous” ODH Flame- or splintershaped hemorrhage – radially oriented and – perpendicular to disc margin Definition of “Glaucomatous” ODH Flame- or splintershaped hemorrhage Not associated with disease other than glaucoma – Vascular occlusive disease – Diabetic retinopathy – Ischemic optic neuropathy Results: Cumulative Incidence of Disc Hemorrhage prior to POAG 0.15 0.10 0.05 0.00 0 12 24 36 48 60 72 84 96 Months Since Randomization Cumulative Incidence of Disc Hemorrhage prior to POAG endpoint 12 months between disc photos Disc hemorrhages may come and disappear between photographs Therefore previous graph almost certainly underestimates the true incidence of ODH Comments To our surprise Tx IOP lowering medicine did not reduce risk of ODH. Q: What does this mean? A: We don’t know – ODH marks inadequate IOP lowering – ODH marks pathogenic mechanism » mechanism is still there » but it no longer causes harm – ODH had lower incidence than POAG and analysis has insufficient power ODH prediction of POAG in multivariate analysis Hazard ratio 3.7 [2.1 – 6.6] After adjusted for: – Treatment Group – Age – Vertical cup/disc ratio – Pattern standard deviation (visual field) – Baseline IOP – Central corneal thickness Summary: Why do you get Drance Hemorrhages? OHTS participants who developed ODHs – Similar to those who develop POAG – including older age, thinner corneas, and larger vertical C/D, higher PSD EXCEPT THAT.. ODH not less frequent with – lower baseline IOP – assignment to treatment Summary: What if you get ODH? ODH is an additional independent risk factor for developing POAG But ODH is not synonymous with developing POAG – 87% of OHT participants with ODH did NOT develop POAG endpoint during follow-up period – 153 eyes of 168 who developed POAG did so without prior ODH Conclusions ODH are difficult to find, but a diligent search is worthwhile, because they represent one of the risk factors to be taken into account when making clinical decisions. 45 How to Incorporate Information From OHTS Into Clinical Practice? August 2010 46 Most OHT patients are at low risk. Most low risk OHT patients can be followed without medication. Delaying treatment for 7.5 years resulted in only a small absolute increase in POAG in low risk participants. Starting treatment of POAG at diagnosis has no major negative effect on prognosis over 5 years. August 2010 47 High risk OHT patients may benefit from more frequent examinations and early treatment taking into consideration: Patient age Health status Life expectancy Personal preference August 2010 48 Some clinicians may elect to follow all OHT patients without treatment. • Requires timely visits, appropriate tests and interpretation. • Risk status changes over time. • Patient education is key August 2010 49 Limitations of OHTS 1. Study IOP goal was 20% reduction. May not be sufficient. 2. No measure of medication adherence. 3. Convenience sample, not populationbased epidemiologic study. 4. Participants healthy and “squeaky clean” at baseline. 5. High threshold for diagnosing POAG. August 2010 50 OHTS Summary 1. Early medical treatment reduces the cumulative incidence of POAG. 2. The absolute effect is greatest in high risk individuals. 3. There is little absolute benefit of early treatment in low risk individuals. August 2010 51 OHTS Summary 4. There are safe and effective treatment options for most ocular hypertensive patients. 5. The risk of developing POAG continues over at least a 15 year follow-up. August 2010 52 OHTS Summary 6. African Americans develop POAG at a higher rate despite similar treatment and similar levels of IOP. Higher incidence is related to baseline risk factors. 7. Individualized assessment of risk is useful to patients and clinicians. August 2010 53 Key References Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JK, Miller JP, Parrish, RK, Wilson MR, Gordon MO for the Ocular Hypertension Treatment Study Group. The Ocular Hypertension Treatment Study: A Randomized Trial Determines That Topical Ocular Hypotensive Medication Delays or Prevents the Onset of Primary Open-Angle Glaucoma. Arch Ophthalmol 2002; 120:701-713. PMID:12049574 Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JK, Miller JP, Parrish RK, Wilson MR, Kass MA for the Ocular Hypertension Treatment Study Group. The Ocular Hypertension Treatment Study: Baseline Factors That Predict The Onset of Primary Open-Angle Glaucoma. Arch Ophthalmol 2002; 120:714-720. PMID:12049575 The Ocular Hypertension Treatment Study (OHTS) Group and the European Glaucoma Prevention Study (EGPS) Group. A validated Prediction Model for the Development of Primary Open-Angle Glaucoma in Individuals with Ocular Hypertension. Ophthalmology 2007; 114(1):10-19. PMCID:1995665 Kass MA, Gordon MO, Gao F, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JK, Miller JP, Parrish RK, Wilson MR, and the Ocular Hypertension Treatment Study (OHTS) Group. Delaying Treatment of Ocular Hypertension. Archives of Ophthalmology 2010; 128(3):276-287. PMID:20212196 August 2010 54 OHTS Clinical Centers Bascom Palmer Eye Institute Baylor Eye Clinic Charles R. Drew University Devers Eye Institute Emory University Eye Center Eye Associates of Washington, DC Eye Consultants of Atlanta Eye Doctors of Washington Eye Physicians and Surgeons of Atlanta Glaucoma Care Center Great Lakes Ophthalmology Henry Ford Hospitals Johns Hopkins University Jules Stein Eye Institute, UCLA Kellogg Eye Center Kresge Eye Institute Krieger Eye Institute Maryland Center for Eye Care Mayo Clinic/Foundation New York Eye & Ear Infirmary Ohio State University Salus University Scheie Eye Institute University of California, Davis University of California, San Diego University of California, San Francisco University of Louisville University Suburban Health Center Washington Eye Physicians & Surgeons Washington University, St. Louis August 2010 55 OHTS Resource Centers Study Chairman’s Office & Coordinating Center Washington University St. Louis, MO Optic Disc Reading Center Visual Field Reading Center Bascom Palmer Eye Institute University of Miami Miami, FL University of California, Davis Sacramento, CA August 2010 OHTS 1,636 participants 880 individuals certified for OHTS: – Clinicians – Coordinators – Perimetrists – Photographers – Technicians August 2010