Joints! - Bremen High School District 228
advertisement

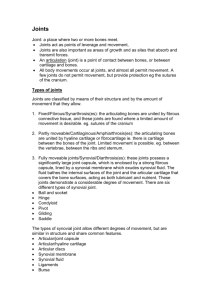
Joints! 3 types of joints if we classify by function (i.e., by the degree of movement possible): 1. Diarthroses (Synovial) Freely moveable joints Shoulder, knee, hip, elbow, interphalangeal, tarsal, and carpal joints 2. Amphiarthroses (Cartilaginous) Amphi-slightly Slightly moveable joints Intervertebral discs, costosternal joints, pubic symphysis 3. Synarthroses (Fibrous) Syn--together Joints with little or no movement Skull sutures, teeth in sockets, 1st costosternal joint. Joint Classification We can also classify joints by structure: 1. Synovial joints: Bones separated by a joint cavity; lubricated by synovial fluid; enclosed in a fibrous joint capsule. Shoulder, hip, elbow, knee, carpal, interphalangeal How would we classify these joints functionally? Joint Classification 2. Fibrous joints: Bones held together by collagenous fibers extending from the matrix of one bone into the matrix of the next. No joint cavity Little or no movement occurs between bones Skull sutures, teeth joints, distal radioulnar joints & tibiofibular joints Types of Fibrous Joints There are three types of fibrous joint: Sutures—very tight articulations between adjacent bones. Only found in the skull. Syndesmosis—the bones are held together by strong, fibrous connective tissue. Bones may be held together by ligaments or interosseous membranes. Very little movement is possible. Gomphosis—a unique peg-and-socket joint at which no movement occurs. Only found between the permanent teeth and the maxilla. Joint Classifications 3. Cartilaginous joints: Bones held together by cartilage; no joint cavity Epiphyseal plates of long bones, costosternal joints, pubic symphysis, intervertebral discs Types of Cartilaginous Joints There are two types of cartilalaginous joints: 1. Symphysis—Examples include the intervertebral discs and the symphysis pubis. 2. Synchondrosis—Examples include the epiphyseal growth plate in a long bone. Herniated Disc Disc Surgery Herniated - Learn about Herniated Disc Surgery YouTube - Back Surgery for Disc Herniation Structure and Function Joints are designed for their function. Let’s look at sutures as our 1st example: What function do you suppose sutures are designed for? Structure and Function Let’s look at some symphyses. What kind of joint is a symphysis? What kind of movement is possible? Name a symphysis! (an obvious one is in the picture) What connects the bones in these joints? Structure and Function Now let’s talk about synovial joints. How do they differ from the previous 2? 5 main structural characteristics: 1. Articular cartilage What kind of cartilage is it? (H _ _____) Where do we find it? What does it do? Structure and Function 2. Articular capsule 2 layered. Surrounds both articular cartilages and the space btwn them. External layer is made of dense irregular CT & is continuous w/ the perisoteum. Inner layer is a synovial membrane made of loose connective tissue. It covers all internal joint surfaces except for those areas covered by the articular cartilage. Structure and Function 3. Joint (Synovial) Cavity 4. The potential space within the joint capsule and articular cartilage Synovial Fluid A small amount of slippery fluid occupying all free space w/i the joint capsule Formed by filtration of blood flowing through capillaries in the synovial membrane Synovial fluid becomes less viscous as joint activity increases. Structure and Function 5. Reinforcing Ligaments What kind of tissue are they? What do you suppose their function is? Double-jointedness results from extra-stretchy ligaments and joint capsules. Is this necessarily a good thing? Other Synovial Structures The knee and hip joints have cushioning fatty pads btwn the fibrous capsule and the synovial membrane or bone. Discs of fibrocartilage (i.e., menisci) which improve the fit btwn bone ends, thus stabilizing the joint. Found in the knee, jaw, and sternoclavicular joint. Bursae are basically bags of lubricant - fibrous membrane bags filled w/ synovial fluid. Often found where bones, muscles, tendons, or ligaments rub together. Synovial Joints YouTube - Types of Synovial Joints Types of Synovial Joints 1. Plane joints Articular surfaces are flat and allow short slipping or gliding movements. Intercarpal and intertarsal joints 2. Hinge joints A cylindrical projection of one bone fits into a troughshaped surface on another (like a hotdog in a bun) Movement resembles a door hinge. Elbow joint – ulna and humerus; Interphalangeal joints Type of Synovial Joints 3. Pivot joints Rounded end of one bone protrudes into a ring formed by another bone or by ligaments of that bone. Proximal radioulnar joint Atlas-axial joint 4. Condyloid joints Oval articular surface of one bone fits into a complementary depression on another. Radiocarpal joints Metacarpophalangeal joints Types of Synovial Joints 5. Saddle joints Each articular surface has convex and concave areas. Each articular surface is saddle-shaped. Carpometacarpal joints of the thumbs. 6. Ball-and-Socket joints Spherical or semi-spherical head of one bone articulates with the cuplike socket of another. Allow for much freedom of motion. Shoulder and hip joints. The Knee Largest and most complex diarthrosis in the body. Primarily a hinge joint, but when the knee is flexed, it is also capable of slight rotation and lateral gliding. Actually consists of 3 joints: Patellofemoral joint Medial and lateral tibiofemoral joints The joint cavity is only partially enclosed by a capsule – on the medial, lateral, and posterior sides. The lateral and medial condyles of the femur articulate with the lateral and medial condyles of the tibia. Between these structures, we have the lateral and medial menisci. Anteriorly, the patellar ligament binds the tibia to the inferior portion of the patella. The superior portion of the patella is then connected to the quadriceps femoris muscle The Knee At least a dozen bursae are associated with the knee. Multiple ligaments are present. The fibular collateral ligament extends from the lateral epicondyle of the femur to the head of the fibula. The tibial collateral ligament connects medial epicondyle of the femur to the medial condyle of the tibial shaft and is also fused to the medial meniscus. Both of these ligaments prevent excessive rotation The Knee The anterior and posterior cruciate ligaments are also very important. ACL connects the anterior intercondylar area of the tibia to the medial side of the lateral femoral condyle. Prevents forward sliding of the tibia and hyperextension of the knee. PCL connects the posterior intercondylar area of the tibia to the lateral side of the medial femoral condyle. Prevents backward displacement of the tibia or forward sliding of the femur. The Knee Clinical Conditions Arthritis describes about 100 different types of inflammatory or degenerative joint diseases. Osteoarthritis Most common arthritis. Normal joint use prompts the release of cartilagedamaging enzymes. If cartilage destruction exceeds cartilage replacement, we’re left with roughened, cracked, eroded cartilages. Eventually bone tissue thickens and forms spurs that can restrict movement. Most common in C and L spine, fingers, knuckles, knees, and hips. Rheumatoid arthritis Chronic inflammatory disorder Marked by flare-ups Autoimmune disease. Body creates antibodies which attack the joint surfaces The synovial membrane can inflame and eventually thicken into a pannus – an abnormal tissue that clings to the articular cartilage. The pannus erodes the cartilage and eventually scar tissue forms and connects the 2 bone ends. This scar tissue can later ossify, fusing the bones together. This is known as ankylosis. Clinical Conditions Clinical Conditions Gouty arthritis When nucleic acids are metabolized uric acid is produced. Normally uric acid is excreted in the urine. If blood [uric acid] rises due to decreased excretion or increased production, it may begin to form needle-shaped crystals in the soft tissues of joints. Inflammation ensues causing painful arthritis. Gout Risk Factors Risk factors for developing gout include obesity, excessive weight gain, especially in youth, moderate to heavy alcohol intake, high blood pressure, and abnormal kidney function. Certain drugs, such as thiazide diuretics (hydrochlorothiazide [Dyazide]), low-dose aspirin, niacin, cyclosporine, tuberculosis medications (pyrazinamide and ethambutol), and others can also cause elevated uric-acid levels in the blood and lead to gout. Furthermore, certain diseases lead to excessive production of uric acid in the body. Examples of these diseases include leukemias, lymphomas, and hemoglobin disorders. Bursitis Bursitis is the painful inflammation or irritation of the bursa. The bursa is a soft, fluid-filled sac that covers and cushions the movement between the bones, tendons and muscles near the joints. Bursitis usually occurs under the shoulder muscles, at the elbows (called epitrochlear bursitis or "tennis elbow"), the hip sockets (called trochanteric bursitis), heel bones (called retrocalcaneal bursitis) or the kneecaps (called infrapatellar bursitis or "housemaid's knee"). It can also occur in the buttocks (called ischiogluteal bursitis) or the thigh (called trochanteric bursitis). Buristis http://www.livestrong.com/video/1662bursitis-health-byte/ Causes of Bursitis Most commonly, bursitis is caused by trauma, infection, and crystal deposits. Some specific factors include: Overuse or injury to the joint areas from playing or working Incorrect posture at work or rest, or poor conditioning before exercise or playing sports An abnormal or poorly positioned joint or bone (such as leg length differences or arthritis in a particular joint) that stresses soft tissue structures. Sometimes in association with other diseases or conditions, such as rheumatoid arthritis, gout, tuberculosis or psoriatic arthritis Staphylococcal or other (bacterial) infection Symptoms of Bursitis Symptoms of bursitis may include: Pain that increases with movement of joint Tenderness of joint Limited movement in the affected areas Swelling and redness in affected areas Treatments of Bursitis Treatment for bursitis includes applying the R.I.C.E therapy, protecting the area, and anti-inflammatory drugs. It can help to protect bursae close to the skin, such as the ankles and knees, with padding. Additionally, deep-heat therapy (diathermy) can also relieve the discomfort and inflammation of bursitis. Anti-inflammatory medications, such as aspirin or over-the-counter nonsteroidal drugs (NSAIDs), such as ibuprofen, naproxen, or indomethacin can often be helpful. If the cause of the bursitis is bacterial, antibiotics will be administered. If the inflammation does not respond to the R.I.C.E. therapy and medications, surgical drainage (aspiration) of fluid from the bursa and the injection of corticosteroids into the bursa is an alternative treatment. Surgical removal of the bursa is a possibility for chronic bursitis. With adherence to treatment, bursitis usually subside in seven to 14 days.