Chapter 5 notes a1
advertisement

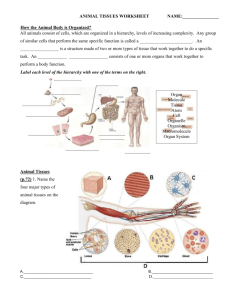
P. 94 Anatomy & Physiology 1 Mrs. Linde 1. adip- = fat 2. areola- = open space 3. chondr- = cartilage 4. -crine = secretion 5. -ectomy = to cut out 6. epi- = upon 7. exo- = outer 8. -glia = glue 9. hist- = tissue 10. meso- = middle 11. neuro- = nerve 12. os- = bone 13. pseudo- = false 14. retic- = net 15. squam- = scale 16. strat- = layer 17. viscero- = body organ Cells are highly organized living units, but they typically do not function alone. Instead, cells work together in groups called tissues groups of similar cells that function together to carry out specialized activities. Histology is the science that deals with the study of tissues. A pathologist is a physician who specializes in laboratory studies of cells and tissues to help other physicians make accurate diagnoses; they examine tissues for any changes that might indicate disease. Body tissues are classified into four basic types based on their structure and functions: 1. Epithelial tissue covers body surfaces; lines body cavities, hollow organs, and ducts (tubes); and forms glands. 2. Connective tissue protects and supports the body and its organs, binds organs together, stores energy reserves as fat, and provides immunity. 3. Muscular tissue generates the physical force needed to make body structures move. 4. Nervous tissue detects changes inside and outside the body and initiates and transmits nerve impulses (action potentials) that coordinate body activities to help maintain homeostasis. A. Most cells are tightly joined into functional units by points of contact between their plasma membranes called cell junctions. 1. Some fuse cells together so tightly that they prevent substances from passing between the cells. a. Important for tissues that line the stomach, intestines, and urinary bladder prevents the contents from leaking out. 2. Others hold cells together so that they don’t separate while performing their functions. 3. Still others form channels that allow ions and molecules to pass between cells = permits cells in a tissue to communicate with each other, enables nerve or muscle impulses to spread rapidly among cells. A. Two types of epithelial tissue (epithelium): (1) Covering and lining epithelium forms outer covering of the skin and some internal organs; lines body cavities, blood vessels, ducts, and the interiors of the respiratory, digestive, urinary, and reproductive systems. It makes up, along with nervous tissue, the parts of the sense organs for hearing, vision, and touch (2) Glandular epithelium makes up the secreting portion of glands, such as sweat glands. 1. Epithelium consists of closely packed cells with little extracellular material between them, and the cells are arranged in continuous sheets, in either single or multiple layers. 2. Epithelial cells have a(n): a. apical (free) surface, which is exposed to a body cavity, lining of an internal organ, or the exterior of the body b. lateral surfaces, which face adjacent cells on either side c. basal surface, which is attached to a basement membrane. 3. Epithelia are avascular = they lack blood vessels. The vessels that supply nutrients to and remove wastes from epithelia are located in adjacent connective tissues. They exchange materials by diffusion. 4. Epithelia have a nerve supply. 5. Because epithelium is subject to a certain amount of wear and tear and injury, it has a high capacity for renewal by cell division. 1. Arrangement of cells in layers. Cells are arranged depending on the functions the epithelium performs: a. Simple epithelium single layer of cells that functions in diffusion, osmosis, filtration, secretion (production/release of mucus/sweat/enzymes), and absorption (intake of fluids/substances). b. Pseudostratified epithelium appears to have multiple layers of cells because the cell nuclei lie at different levels and not all cells reach the apical surface. c. Stratified epithelium consists of two or more layers of cells that protect underlying tissues where there is considerable wear and tear. 2. Cell shapes: a. Squamous cells flat, arranged like floor tiles, and thin = rapid passage of substances. b. Cuboidal cells as tall as they are wide, and shaped like cubes or hexagons; may have microvilli and function in either secretion or absorption. c. Columnar cells much taller than they are wide (like columns) and protect underlying tissues. May have cilia or microvilli, and often are specialized for secretion and absorption. d. Transitional cells change shape, from flat to cuboidal, as organs (like urinary bladder) stretch to a larger size and then collapse to a smaller size. A. Simple squamous epithelium Description: Single layer of flat cells; centrally located nucleus. Location: Lines heart, blood vessels, lymphatic vessels, air sacs of lungs, Bowman’s capsule of kidneys, and inner surface of the eardrum; forms epithelial layer of serous membranes, such as the peritoneum. Function: Filtration, diffusion, osmosis, and secretion in serous membranes. B. Simple cuboidal epithelium Description: Single layer of cube-shaped cells; centrally located nucleus. Location: Covers surface of ovary, lines anterior surface of capsule of the lens of the eye, forms the pigmented epithelium at the posterior surface of the eye, lines kidney tubules and smaller ducts of many glands, and makes up the secreting portion of some glands such as the thyroid gland. Function: Secretion and absorption. C. Nonciliated simple columnar epithelium Description: Single layer of nonciliated columnlike cells with nuclei near bases of cells; contains goblet cells and cells with microvilli in some locations. Location: Lines most of the gastrointestinal tract (from the stomach to the anus), ducts of many glands, and gallbladder. Function: Secretion and absorption. D. Ciliated simple columnar epithelium Description: Single layer of ciliated column-like cells with nuclei near bases; contains goblet cells in some locations. Location: Lines a few portions of upper respiratory tract, uterine (fallopian) tubes, uterus, some paranasal sinuses, and central canal of spinal cord. Function: Moves mucus and other substances by ciliary action. E. Pseudostratified columnar epithelium Description: Not a true stratified tissue; nuclei of cells are at different levels; all cells are attached to basement membrane, but not all reach the apical surface. Location: Pseudostratified ciliated columnar epithelium lines the airways of most of upper respiratory tract; pseudostratified nonciliated columnar epithelium lines larger ducts of many glands, epididymis, and part of male urethra. Function: Secretion and movement of mucus by ciliary action. F. Stratified squamous epithelium Description: Several layers of cells; cuboidal to columnar shape in deep layers; squamous cells form the apical layer and several layers deep to it; cells from the basal layer replace surface cells as they are lost. Location: Keratinized variety forms superficial layer of skin; nonkeratinized variety lines wet surfaces, such as lining of the mouth, esophagus, part of epiglottis, part of pharynx, and vagina, and covers the tongue. Function: Protection. G. Stratified cuboidal epithelium Description: Two or more layers of cells in which cells in the apical layer are cube-shaped. Location: Ducts of adult sweat glands and esophageal glands and part of male urethra. Function: Protection and limited secretion and absorption. H. Stratified columnar epithelium Description: Several layers of irregularly shaped cells; only the apical layer has columnar cells. Location: Lines part of urethra, large excretory ducts of some glands such as esophageal glands, small areas in anal mucous membrane, and a part of the conjunctiva of the eye. Function: Protection and secretion. I. Transitional epithelium Description: Appearance is variable (transitional); shape of cells in apical layer ranges from squamous (when stretched) to cuboidal (when relaxed). Location: Lines urinary bladder and portions of ureters and urethra. Function: Permits distention. J. Endocrine glands Description: Secretory products (hormones) diffuse into blood after passing through interstitial fluid. Location: Examples include pituitary gland at base of brain, pineal gland in brain, thyroid and parathyroid glands near larynx, adrenal glands superior to kidneys, pancreas near stomach, ovaries in pelvic cavity, testes in scrotum, and thymus in thoracic cavity. Function: Produce hormones that regulate various body activities. K. Exocrine glands Description: Secretory products released into ducts. Location: Sweat, oil, and earwax glands of the skin; digestive glands such as salivary glands, which secrete into mouth cavity, and pancreas, which secretes into the small intestine. Function: Produce substances such as sweat, oil, earwax, saliva, or digestive enzymes. Connective tissue is one of the most abundant and widely distributed tissues in the body. In its various forms, connective tissue has a variety of functions. It binds together, supports, and strengthens other body tissues; protects and insulates internal organs; compartmentalizes structures such as skeletal muscles; is the major transport system within the body (blood, a fluid connective tissue); is the major site of stored energy reserves (adipose, or fat tissue); and is the main site of immune responses. 1. 2. Two basic elements: cells and extracellular matrix the material between its widely spaced cells. The extracellular matrix consists of protein fibers and ground substance, the material between the cells and the fibers. The extracellular matrix is usually secreted by the connective tissue cells and determines the tissue’s qualities (in cartilage, matrix is firm but pliable; in bone, it is hard and not pliable. Unlike epithelia: Connective tissues do not usually occur on body surfaces, and usually are highly vascular (have a rich blood supply). Exceptions include cartilage, which is avascular, and tendons, with a scanty blood supply. Like epithelia: Except for cartilage, connective tissues are supplied with nerves. 1. Fibroblasts large, flat cells with branching processes present in several connective tissues, and usually the most numerous. Fibroblasts migrate through the connective tissue, secreting the fibers and ground substance of the extracellular matrix. 2. Macrophages develop from monocytes, a type of white blood cell. Macrophages have an irregular shape with short branching projections and are capable of engulfing bacteria and cellular debris by phagocytosis. 3. Plasma cells small cells that develop from a type of white blood cell called a B lymphocyte. Plasma cells secrete antibodies, proteins that attack or neutralize foreign substances in the body = important part of the body’s immune response. 4. Mast cells abundant alongside the blood vessels that supply connective tissue. They produce histamine, a chemical that dilates small blood vessels as part of the inflammatory response, the body’s reaction to injury or infection. Mast cells can also kill bacteria. 5. Adipocytes fat cells or adipose cells, are connective tissue cells that store triglycerides (fats). They are found below the skin and around organs such as the heart and kidneys. Each type of connective tissue has unique properties, based on the specific extracellular materials between the cells. The extracellular matrix consists of a fluid, gel, or solid ground substance plus protein fibers. Ground substance, the component of a connective tissue between the cells and fibers, supports cells, binds them together, and provides a medium through which substances are exchanged between the blood and cells. The ground substance plays an active role in how tissues develop, migrate, proliferate, and change shape, and in how they carry out their metabolic functions. Ground substance contains water and an assortment of large organic molecules, many of which are complex combinations of polysaccharides and proteins. Fibers in the extracellular matrix strengthen and support connective tissues. Three types of fibers are embedded in the extracellular matrix between the cells: collagen fibers, elastic fibers, and reticular fibers. 1. 2. 3. Very strong and resist pulling forces, but they are not stiff, which promotes tissue flexibility. Often occur in bundles lying parallel to one another = great strength. Consist of the protein collagen = the most abundant protein in your body, representing about 25% of total protein. Found in most types of connective tissues, especially bone, cartilage, tendons, and ligaments. Despite their strength, ligaments may be stressed beyond their normal capacity. This results in sprain, a stretched or torn ligament. The ankle joint is most frequently sprained. Because of their poor blood supply, the healing of even partially torn ligaments is a very slow process; completely torn ligaments require surgical repair. 1. 2. 3. 4. Smaller in diameter than collagen fibers; branch and join together to form a network within a tissue. Consists of elastin (protein) surrounded by fibrillin (glycoprotein), which is essential to the stability of an elastic fiber. Strong, but can be stretched up to one-and-ahalf times their relaxed length without breaking; also have the ability to return to their original shape after being stretched = elasticity. Plentiful in skin, blood vessel walls, and lung tissue. Marfan syndrome (MAR-fan) is an inherited disorder caused by a defective fibrillin gene. The result is abnormal development of elastic fibers. Tissues rich in elastic fibers are malformed or weakened. Structures affected most seriously are the covering layer of bones (periosteum), the ligament that suspends the lens of the eye, and the walls of the large arteries. People with Marfan syndrome tend to be tall and have disproportionately long arms, legs, fingers, and toes. A common symptom is blurred vision caused by displacement of the lens of the eye. The most life-threatening complication of Marfan syndrome is weakening of the aorta (the main artery that emerges from the heart), which can suddenly burst. 1. 2. Consist of collagen and a coating of glycoprotein, provide support in the walls of blood vessels and form branching networks around fat cells, nerve fibers, and skeletal and smooth muscle cells. Much thinner than collagen fibers, but like collagen fibers, provide support and strength and also form the stroma (= bed or covering) or supporting framework of many soft organs, such as the spleen and lymph nodes. These fibers also help form the basement membrane. A. Areolar connective tissue Description: Consists of fibers (collagen, elastic, and reticular) and several kinds of cells (fibroblasts, macrophages, plasma cells, adipocytes, and mast cells) embedded in a semifluid ground substance. Location: Subcutaneous layer deep to skin; superficial region of dermis of skin; lamina propria of mucous membranes; and around blood vessels, nerves, and body organs. Function: Strength, elasticity, and support. B. Adipose tissue Description: Consists of adipocytes, cells specialized to store triglycerides (fats) as a large centrally located droplet; nucleus and cytoplasm are peripherally located. Location: Subcutaneous layer deep to skin, around heart and kidneys, yellow bone marrow, and padding around joints and behind eyeball in eye socket. Function: Reduces heat loss through skin, serves as an energy reserve, supports, and protects. D. Dense regular connective tissue Description: Extracellular matrix looks shiny white; consists mainly of collagen fibers regularly arranged in bundles; fibroblasts present in rows between bundles. Location: Forms tendons (attach muscle to bone), most ligaments (attach bone to bone), and aponeuroses (sheetlike tendons that attach muscle to muscle or muscle to bone). Function: Provides strong attachment between various structures. E. Dense irregular connective tissue Description: Consists predominantly of collagen fibers randomly arranged and a few fibroblasts. Location: Fasciae (tissue beneath skin and around muscles and other organs), deeper region of dermis of skin, periosteum of bone, perichondrium of cartilage, joint capsules, membrane capsules around various organs (kidneys, liver, testes, lymph nodes), pericardium of the heart, and heart valves. Function: Provides strength. F. Elastic connective tissue Description: Consists predominantly of freely branching elastic fibers; fibroblasts are present in spaces between fibers. Location: Lung tissue, walls of elastic arteries, trachea, bronchial tubes, true vocal cords, suspensory ligament of penis, and ligaments between vertebrae. Function: Allows stretching of various organs. C. Reticular connective tissue Description: A network of interlacing reticular fibers and reticular cells. Location: Stroma (supporting framework) of liver, spleen, lymph nodes; red bone marrow, which gives rise to blood cells; reticular lamina of the basement membrane; and around blood vessels and muscles. Function: Forms stroma of organs; binds together smooth muscle tissue cells; filters and removes worn-out blood cells in the spleen and microbes in lymph nodes. G. Hyaline cartilage Description: Consists of a bluish-white, shiny ground substance with fine collagen fibers and many chondrocytes; most abundant type of cartilage. Location: Ends of long bones, anterior ends of ribs, nose, parts of larynx, trachea, bronchi, bronchial tubes, and embryonic and fetal skeleton. Function: Provides smooth surfaces for movement at joints, as well as flexibility and support. H. Fibrocartilage Description: Consists of chondrocytes scattered among bundles of collagen fibers within the extracellular matrix. Location: Pubic symphysis (point where hip bones join anteriorly), intervertebral discs (discs between vertebrae), menisci (cartilage pads) of knee, and portions of tendons that insert into cartilage. Function: Support and fusion. I. Elastic cartilage Description: Consists of chondrocytes located in a threadlike network of elastic fibers within the extracellular matrix. Location: Lid on top of larynx (epiglottis), part of external ear (auricle), and auditory (eustachian) tubes. Function: Gives support and maintains shape. Bones are organs composed of several different connective tissues, including bone or osseous tissue. Bone tissue has several functions. It supports soft tissues, protects delicate structures, and works with skeletal muscles to generate movement. Bone stores calcium and phosphorus; stores red bone marrow, which produces blood cells; and houses yellow bone marrow, a storage site for triglycerides. 1. 2. Blood tissue (blood) connective tissue with a liquid extracellular matrix called blood plasma = pale yellow fluid that consists mostly of water with a wide variety of dissolved substances: nutrients, wastes, enzymes, hormones, respiratory gases, and ions. Suspended in the plasma are red blood cells, white blood cells, and platelets. Red blood cells transport O2 to body cells and remove CO2 from them. White blood cells are involved in phagocytosis, immunity, and allergic reactions. Platelets participate in blood clotting. Lymph fluid that flows in lymphatic vessels. It is a connective tissue that consists of several types of cells in a clear extracellular matrix similar to blood plasma but with much less protein. Muscular tissue consists of elongated cells called muscle fibers that are highly specialized to generate force. As a result of this characteristic, muscular tissue produces motion, maintains posture, and generates heat. It also offers protection. Based on its location and certain structural and functional characteristics, muscular tissue is classified into three types: Skeletal muscle tissue is named for its location—it is usually attached to the bones of the skeleton. 2. Cardiac muscle tissue forms the bulk of the wall of the heart. 3. Smooth muscle tissue is located in the walls of hollow internal structures such as blood vessels, airways to the lungs, the stomach, intestines, gallbladder, and urinary bladder. 1. Despite the awesome complexity of the nervous system, it consists of only two principal types of cells: 1. 2. Neurons or nerve cells sensitive to various stimuli; convert stimuli into nerve impulses (action potentials) and conduct these impulses to other neurons, to muscle fibers, or to glands. Neuroglia do not generate or conduct nerve impulses, but they do have many other important supportive functions. Membranes flat sheets of pliable tissue that cover or line a part of the body. The combination of an epithelial layer and an underlying connective tissue layer constitutes an epithelial membrane. The principal epithelial membranes of the body are mucous membranes, serous membranes, and the cutaneous membrane, or skin. Another kind of membrane, a synovial membrane, lines joints and contains connective tissue but no epithelium. 1. 2. 3. Lines a body cavity that opens directly to the exterior = line the entire digestive, respiratory, and reproductive systems and much of the urinary system. The epithelial layer of a mucous membrane secretes mucus, which prevents the cavities from drying out. It also traps particles in the respiratory passageways, lubricates and absorbs food as it moves through the gastrointestinal tract, and secretes digestive enzymes. The connective tissue layer helps bind the epithelium to the underlying structures. It also provides the epithelium with oxygen and nutrients and removes wastes via its blood vessels. 1. 2. Line body cavities that don’t open directly to the exterior, and it also covers the organs that lie within the cavity. Two parts: a. Parietal layer part attached to the cavity wall b. Visceral layer part that covers and attaches to the organs inside these cavities. Each layer consists of areolar connective tissue covered by mesothelium. Mesothelium is a simple squamous epithelium. It secretes serous fluid, a watery lubricating fluid that allows organs to glide easily over one another or to slide against the walls of cavities. 3. The serous membrane lining the thoracic cavity and covering the lungs is the pleura. The serous membrane lining the heart cavity and covering the heart is the pericardium. The serous membrane lining the abdominal cavity and covering the abdominal organs is the peritoneum. 1. 2. 3. Line the cavities of some joints. Composed of areolar connective tissue and adipose tissue with collagen fibers; NO EPITHELIAL LAYER. Contain cells which secrete synovial fluid to lubricate the ends of bones as they move at joints, nourishe the cartilage covering the bones, and remove microbes and debris from the joint cavity. New cells from stroma or parenchyma Epithelial cells originate from stem cells in defined areas of tissue layer Bone regenerates readily, cartilage poorly Muscular tissue can replace cells but slowly Nerve tissue is poorest at replacement although some stem cells seem to be available. Replacement from stroma –> scar tissue & functional loss.