Community Based Mental Health Re-design Project Communication
advertisement

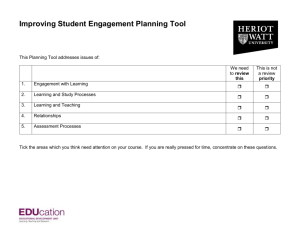
Community Based Mental Health Re-design Project Communication Brief August 2015 CURRENT MENTAL HEALTH SERVICE MODEL Where we are now General Public Third Sector General GP Orgs Public IAPT LYPFT SPA A&E Mon - Fri 24/7 24/7 Crisis FUTURE PROPOSED MENTAL HEALTH SERVICE MODEL Where we need to be Information Portal Information & Advice Prevention & self management Primary Care Wrap around & New Models of Care Mental health long term conditions and Liaison mental health 24/7 access to advice and guidance inc. psychiatrist, pharmacist CMHT Assessment Front Door Tiered assessment Third Sector Orgs same day wherever possible Triage accessed via call centre Crisis response & walk in Navigator service Mental Health Needs/ Cluster Pathways Weaknesses of the current model No public information on how to access services Assumptions on what services can do No central assessment service so when GP’s make a referral it can be bounced back due to ineligibility Results in inappropriate referrals Repeat referrals and assessments increase waiting times and dis-engagement with services Requirements of any new model Centralised Information and self-help resources Better use of universal services to support the issues that many service users face that relate to housing, debt, employment Principle of no wrong referral or bounce back Focus on early intervention avoiding unnecessary pathways into secondary care Shifts some current secondary care resource into primary care to “wrap around” GPs and contribute to the new models of care. Uses cluster based standardised assessment process reducing the number of repeat assessments Community Based Mental Health Re-design Project Communication Brief August 2015 Leeds has a range of mental health services provided by both statutory and voluntary community sector commissioned by NHS and LCC. Feedback from users, carers and professionals using and working within services tell us that these services are valued and are of high quality. However they also tell us that the system as a whole is difficult to understand or to navigate in a coherent way and hard to know what is the right place first time. In order to rebalance the system Leeds has developed a Mental Health Framework (2014) which describes the near future direction and priorities for mental health services for 2014-17. The agreed framework sets the direction of travel and commissioning priorities for health and social care mental health services of the future by describing five key outcomes and principles for our services. Accompanying this is also the intention to explore health and social care pooled budgets in the future in order to reduce duplication and maximise efficiency. From a series of Mental Health Framework implementation and provider& partner workshops, four cross cutting priorities were identified which if developed would achieve a significant contribution to the delivery of the five Mental Health Framework key outcomes. These are crucial if the whole system is to rebalance towards prevention, early intervention and timely access including extended and integrated offers of support that also address the wider determinants of poor mental health. The four priorities below now form the basis of a two year Mental Health Programme of work hosted by Leeds North CCG on behalf of the 3 Leeds CCG’s, supported by Leeds West & Leeds South & East CCGs and programme managed by Jenny Thornton. A project manager has been appointed for each priority. Information Community Based Mental Health Re-Design Crisis & Urgent Care Children & Families Community Based Mental Health Re-design Project Communication Brief August 2015 The Community Based Mental Health Re-Design Project - Consultation Phase. Consulting on a broad outline model of 3 key areas: Community Based Mental Health ReDesign 1) Primary Care Wrap Around-New Models Of Care 2) Single Point of Assessment 3) Mental Health Needs(Cluster) Pathways The development of a web based Information Portal is a first and integral ‘front end’ discrete project of the Mental Health Framework. The draft proposal model is based on a range of engagement events and meetings with user and carer groups, providers and partners and national reviews of best practice models across the country over the last 18 months. Through this work three key areas for change have emerged (above). An extensive service user consultation has been initiated to inform future models and agree core principles. The Community Based Mental Health Re-Design project has now begun the consultation phase with stakeholder groups exploring the broad outline model and three key areas for change. This transformation programme sits in a national context of developing New Models of Care for Primary Care and it is vital that mental health redesign is integrated into the development of these new models. Feedback from consultation will be used to further refine and develop the design of a more detailed model. Regular communications on progress will be made and stakeholders will be invited to use co-production methods to develop and test thinking and options. A final revised model will then return to the stakeholder groups and governance process for approval. Community Based Mental Health Re-design Project Communication Brief August 2015 Information Portal Information & Advice Prevention & self management Community Based Mental Health Re-Design Project Primary Care WrapAround/New models of Care One Assessment Front Door Mental Health Needs /Cluster Based Pathways IP Project Manager appointed- Alicia Ridout aridout1@nhs.net Website development - procured via YOUMEE. Project Manager appointed 1st July marrisa.carroll@nhs.net Broad outline model contains three high level work streams identified & now consulting for continuing design and coproduction planning Continuous Engagement and Consultation on: Primary Care Wrap around & New Models of Care Work Stream Mental health long term conditions and 24/7 access to advice and guidance inc. Liaison mental health psychiatrist, pharmacist Continuous Engagement and Consulting on: One Assessment Front Door Work Stream Tiered assessment same day wherever possible Triage accessed via call centre Crisis response & walk in How might new models of care look? Exploring how interventions concerned with addressing the wider determinants of poorer mental health could be Exploring possibilities for enhanced models of care within GP & integrated teams. Continuity/Navigator service Multi-disciplinary & multi-agency assessment hub for primary, secondary ASC & third sector Crisis & non-crisis pathways Same day triage & tiered holistic assessment, stepped model Low intensity intervention offer as standard, e.g. stress management seminar session Continuous Engagement and Consulting on: Mental Health Needs Cluster Based Pathways Work Stream Tiered Intervention linked to needs/cluster bands following NICE guidance Specialist staff prioritised for most complex needs & for advisory supervisory roles Recovery focussed culture & asset based care & support plans New ways of delivering Care coordination Increased and enhanced psychological thinking Increase in support worker/ peer support staff level Use a single recording system used across agencies How a re-designed whole community mental health support system could be in the future Tiered intervention linked to needs /21 cluster bands following NICE guidance Care Coordination by most appropriate, suitably trained person across agencies Specialist professionals focus on most complex needs Partnerships delivering recovery focused & asset based care coordinated support plans Shared single recording systems across agencies