Coma & Brain Death
advertisement

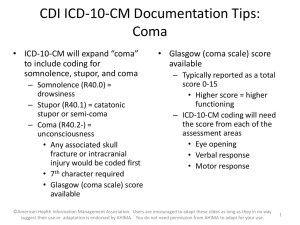
Michelle-Lee Jones Neurology PGY-3 July 15th, 2009 Coma & Brain Death - Outline • COMA: – – – – Definition Pathophysiology Aetiologies Exam & relevant investigations – Differential diagnosis & related conditions – Prognostication • BRAIN DEATH: – Definition – Determination, including the role of confirmatory testing – Ongoing controversies COMA • Definition: –Greek in origin – “deep sleep or trance” –It refers to an unconscious state characterised by a lack of both arousal and responsiveness COMA • Related disorders of consciousness: – Stupor (Latin “ to be stunned”): aroused by and responsive to only the most vigorous stimuli – Minimally conscious state: Markedly impaired consciousness with evidence of self or environmental awareness (intermittent rudimentary vocal or motor responses) COMA • Related disorders of consciousness: – Vegetative state: No awareness of self or environment, but basic cycling of arousal states & periodic eye-opening are present – Persistent vegetative state: Vegetative state persisting for at least 30 days COMA • Pathophysiology: – The ascending reticular activating system (ARAS) controls one’s level of arousal or alertness – The ARAS is comprised of the rostral brainstem tegmentum (cholinergic peribrachial nuclei*), the diencephalon and associated cortical projections – *pedunculopontine tegmental nucleus & lateral dorsal tegemental nucleus COMA • Pathophysiology: – The peribrachial nuclei project via 2 major pathways – dorsal & ventral pathways – Dorsal: glutaminergic projections from thalamic nuclei to various cortical areas – Ventral: histaminergic projections from the posterior hypothalamus (hypocretin, orexin also) & cholinergic projections from the basal forebrain to many cortical areas (McGill connection Herbert Jasper 1961 & Barbara Jones 2000) COMA • Pathophysiology: – Sleep centre: Preoptic area of hypothalamus (GABAergic) – Notably, the ARAS pathways exhibit redundancy that may facilitate recovery of the arousal system (within 2-3 weeks if lesions are more rostral) COMA PERIBRACHIAL NUCLEI (http://www.nature.com/nature/journal/v437/n7063/images/nature04284f2.2.jpg) COMA Dorsal & Ventral ARAS pathways (Jones, B.E. 2000) COMA • CAVEAT: Damage to the ARAS and associated structures or both hemispheres is usually necessary to cause a comatose state. Occasionally, left hemispheric dysfunction can per se lead to coma... COMA • Aetiologies – Structural lesions: • Destructive & compressive • Ischemic stroke, haemorrhage, tumours & inflammation/infection • Long list including SDH, EDH, SAH, cerebral contusion, pontine hemorrhage, cerebellar hemorrhage/infarction, brain abscess, vasculitis, venous sinus thrombosis, etc. COMA • Aetiologies – Herniation Syndromes: • Munro-Kellie doctrine to consider • Lateral displacement of the diencephalon (e.g. basal ganglia bleed) – monitor via displacement of the calcified pineal gland; need 9 to 13 mm shift to produce coma; related to initial impairment of consciousness COMA • Aetiologies – Herniation Syndromes: • Falcine herniation – – expanding mass causes the cingulate gurus & pericallosal/callosomarginal arteries to be compressed & displaced under the falx – Medial wall of hemisphere - infarction & edema – Diencephalic distortion via downward herniation or midline shift COMA • Aetiologies – Herniation Syndromes: • Uncal hernation – – expanding mass causes medial and downward herniation of the medial temporal lobe into the tentorial notch – ipsilateral fixed & dilated pupil – ocular dysmotility – contralateral (uncus presses on nearby cerebral peduncle) or ipsilateral hemiparesis (Kernohan’s sign) – PCA infarction COMA • Aetiologies – Herniation Syndromes: • Central transtentorial herniation – expanding mass causes downward herniation of the diencephalon and pressure on the midbrain – Ischemia & infarction as feeder vessels are stretched and compressed – Diabetes insipidus with pituitary stalk avulsion COMA • Aetiologies – Herniation Syndromes: • Tonsillar herniation – Cerebellar tonsils forced down through foramen magnum e.g. SAH – Medullary compression apnea & compensatory HTN • Rostrocaudal deteriortion – downward displacement of pons/midbrain; Duret h. • Upward brainstem herniation Posterior fossa lesion expands upward, compresses dorsal midbrain COMA Herniation Syndromes http://www.lfhk.cuni.cz/patfyz/I ntranet/Figures/88/5.26.jpg COMA • Aetiologies – Metabolic disturbances/toxins • Hypoglycemia, hyperglycemic hyperosmolar state, diabetic ketoacidosis • Hyper/hyponatremia, hyper/hypocalemia, hypo/hypermagnesemia, hyper/hypothroidism • Uremic or hepatic encephalopathy • Drugs such as alcohol, sympathomimetics, opioids, antidepressants, salicylates, etc. • Hypothermia, porphyria, mitochondrial disorders – Ischemia/Hypoxia, inflammation, infections, seizures COMA • Physical Examination & Investigations – General inspection: Racoon eyes, Battle sign, hemotympanum, CSF rhinorrhea or otorrhea basal skull fracture – Elevated BP: hypertensive encephalopathy (>250/150), intracerebral or subarachnoid hemorrhage; acute ischemic infarct – Respiratory status: Cheyne-Stokes, apneustic breathing, atactic respiration etc. – Hypothermia: ethanol or sedative drug intoxication, myxedema, Wernicke encephalopathy, hepatic encephalopathy hypoglycemia COMA • Physical Examination & Investigations – Hyperthermia: status epilepticus, malignant hyperthermia, anticholinergic drug intoxication, hypothalamic lesions, pontine hemorrhage, heat stroke – Meningeal irritation signs for meningitis or subarachnoid hemorrhage – Fundoscopic exam: papilledema, retinal hemorrhages (chronic or acute HTN); subhyaloid (superficial retinal) hemorrhages for subarachnoid hemorrhage COMA • Physical Examination & Investigations Pupil size, location & reactivity Likely site of pathology > 7 mm, non-reactive 3rd nerve compression; anticholinergic intox. Slightly smaller, reactive Early thalamic compression Fixed midsized pupils ≈ 5 mm Midbrain injury Pinpoint, minimally reactive Opioid overdose; pontine injury, organophosphates, neurosyphilis COMA • Physical Examination & Investigations – Oculocephalic & oculovestibular reflexes: • If the brainstem is intact, a comatose patient will demonstrate full conjugate horizontal eye movements during the oculocephalic testing and tonic conjugate movement of both eyes to the side of the ice-water irrigation during caloric testing. • Absent oculovestibular responses in a comatose patient pontine injury, sedative drug intoxication (can also see downward deviation of one or both eyes) COMA • Physical Examination & Investigations COMA • Physical Examination & Investigations – Metabolic, infectious, vasculitic, stroke W/U – CT, MRI, EEG (mild slowing to burst suppression – mortality rate for the latter?) – One study found that 8% of patients comatose secondary to brain injury are in NCSE – role for continuous EEG monitoring in the ICU? COMA • Differential Diagnosis – the pseudocomas: – – – – Locked-in syndrome Akinetic mutism Catatonia Psychogenic unresponsiveness (which tests can help us differentiate it from a true coma) – Minimally conscious – Vegetative states COMA - Prognostication: AAN guidelines for coma post CPR COMA - Prognostication Probability of Recovering Independent Function (%) Time Since onset of Coma (Days) Sign 0 1 3 7 No verbal response 13 8 5 6 No eye opening 11 6 4 0 Unreactive pupils 0 0 0 0 No spontaneous eye movements 6 5 2 0 No caloric responses 5 6 6 0 Extensor posturing 18 0 0 0 Flexor posturing 14 3 0 0 Absent motor responses 4 3 0 0 Data from Levy et al2 Prognostic Signs in Coma from Global Cerebral Ischemia. Comparison of the Findings in Two Studies (Clinical Neurology, Aminoff) Data from Edgren et al3 No eye opening to pain 31 8 0 0 Unreactive pupils 17 7 0 0 BRAIN DEATH • Definition: – The irreversible loss of brain function, inclusive of the brainstem • Determination: – Triad to remember: COMA, ABSENCE OF BRAINSTEM REFLEXES (pupil, corneal, VOR, pharyngeal & laryngeal) & APNEA – Exclusion of confounding clinical conditions (see table) BRAIN DEATH Morenski et. al , 2003 BRAIN DEATH • Determination continued: BRAIN DEATH • Spontaneous and reflex movements that may be seen in brain death: BRAIN DEATH • Ancillary tests: – Transcranial doppler US – Conventional angiography – EEG – Technetium-99m brain scan – SSEPs: N20-P22 absence bilaterally with median nerve stimulation Morenski et. al, 2003 A few good references • AAN Determining Brain Death in Adults Current guidelines • Prediction of Outcome in Comatose Survivors after Cardiopulmonary Resuscitation Current guidelines July 2006 • Plum and Posner's Diagnosis of Stupor and Coma, 4th edition (☆☆☆☆☆) – great book!