diabetic emergencies - Anesthesia Slides, Presentations and
advertisement

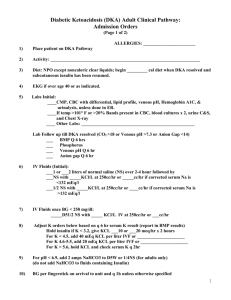
DIABETIC EMERGENCIES – UPDATE AND CONTROVERSIES Dr. S. Parthasarathy MD., DA., DNB, MD (Acu), Dip. Diab. DCA, Dip. Software statistics PhD (physio) Mahatma Gandhi Medical college and research institute , puducherry India When ever there are updates , there will be controversies Diabetic emergencies Diabetic keto acidosis Hyper osmolar hyperglycemic non ketotic coma Hypoglycemia Lactic acidosis - ?? nonexistent Definition – clinical and biochemical DKA is defined clinically as an acute state of severe uncontrolled diabetes associated with ketoacidosis that requires emergency treatment with insulin and intravenous fluids RBS = > 250 mg % Ketones > 5 meq/l pH < 7.3 bicarb < 18 meq / l Insulin Deficiency (Absolute or Relative) Glucose uptake Hepatic glucose Production Hyperglycemia Osmotic diuresis Hypotonic losses Lipolysis Protein catabolism Nitrogen loss Amino acids Gluconeogenesis Glycerol Free Fatty acids Ketogenesis Ketonemia ELECTROLYTE DEPLETION DEHYDRATION Pathophysiology of DKA ACIDOSIS Ketonuria Mind boggling slide !! Looks like As simple as this Uncontrolled DM Trigger factor Severe hyperglycemia Glycosuria , loss of water, electrolytes Protein breakdown Lipid breakdown and Ketogenesis What happens in DKA ?? Hyperglycemia Glycosuria Water ( 6 litres) Electrolytes ( K+ 300, Cl- 400 Na 500 meq) Beta oxidation of fatty acids – Keto acids -acetone, beta-hydroxy butyrate, aceto acetate. Fruity odour, nausea The “I” problem I am the professor !! I am rich !! I am well qualified !! I am the best doctor !! I am the best husband !! The precipitating factors Infection. Infarction (heart or cerebrum) Insulin lack. Indiscrete drugs. Infant (pregnancy) Injuries And as usual unidentified ?? Update avoid DKA self-testing for urinary ketones and adjusting their insulin regimens on sick days. Symptoms Anorexia, Nausea, vomiting, Acute abdomen Lethargy, Myalgia, Dyspnea Hypothermia, Hyporeflexia, Hypotonia, Seizures , Stupor, coma Headache, chest pain, pleurisy Signs Air hunger – acidotic (kussmaul) respiration Dehydration,Confusion, drowsiness, coma (= 10%). Hypotension,Tachycardia Acetone odour on breath Any system We know medicine !! symptom spectrum is a clinical collection but a patient may present with uncontrolled diabetes, an UTI and vomiting. Beware don’t treat as gastritis. It may be DKA Uncontrolled diabetes , Discomfort,vomiting ECG – MI , Ketones + ve Diagnostic Criteria For DKA Features Mild Moderate Severe Plasma glucose (mg/dl) > 250 > 250 > 250 Arterial pH 7.25-7.30 7.00-7.24 <7.00 Serum bicarbonate (mEq/L) 15-18 10 to <15 < 10 Urine ketones Positive Positive Positive Serum ketones Positive Positive Positive Effective serum osmolality Variable Variable Variable (mOsm/kg) > 10 > 12 > 12 Anion gap Alert Alert/drowsy Stupor/coma Alteration in sensoria Take history !! Investigate Blood – sugar , urea , creatinine, electrolytes ABG, (venous BG) ketones , TC, DC, blood cultures ,amylase, Serum lipase CVP , X ray, CT , MRI sos ECG every 6 hours if doubted Urine ketones, deposits and culture Plasma osmolarity 2 (Na + K) + BUN/3 + glucose/18 2( 135 +5) + 15/3 + 300/18 280 + 5 + 16.6 = 301.6 Around 290 in DKA Around 310 in HHS Don’t believe lab fully Test false High glucose hyponatremia High triglycerides low glucose Ketones high creatinine Treat patients – not labs Urine tests acetoacetate But betahydroxy butyrate is predominant Next day urine positive but patient better Treatment of DKA in Adults Fluid replacement Insulin replacement Potassium replacement Phosphate replacement Bicarbonate replacement Management of precipitating factor General Medical Care (ICU). The average fluid deficit is 3–5 liters In young, otherwise healthy patients begin with bolus of 1 liter of normal saline followed by an infusion of normal saline at 500 ml/hour for several hours. 1 +1 2 in medicine IV fluids - Vary in infarct patients , Appropriate monitoring and infusion √ mild DKA should be given normal saline at 250 ml/hour; those with elevated corrected serum sodium should be given half-normal saline at 250 ml/hour. (150 meq 0r osm 330 ) Glucose NS at 250 mg or 180 mg If sure of the electrolytes, Ringer lactate infusion is acceptable Insulin loading dose of regular insulin at 0.1 units/kg 60 kg means 6 units regular insulin IV Followed by 6 units / hour RBS comes down by 50 – 75 mg/ hour RBS does not fall – double the dose Mild cases no loading dose Actre Actress jayamala sabarimala controversy Insulin 0.14 units / kg start – no loading dose IM regular insulin (0.3 units/kg), – some centers Oral intake - SC insulin 6 hours prior to stopping IV Extended insulin- better results Electrolyte replacement: Serum potassium (mEq/L) > 5.3 Action No additional potassium; recheck in 1 hr 4.0–5.3 Add KCl 10 3.5 to < 4.0 Add KCl 20 < 3.5 Hold insulin Add KCl 20–60 Continuous cardiac monitoring Critically ill patients with DKA manifest hypophosphatemia during resuscitation avoid potential muscle cardiac weakness and and skeletal respiratory depression from hypophosphatemia, a serum phosphate of < 1.5 mg/dl should be repleted with K2PO4 at 0.5 ml/hour. Usually rare NO ROUTINE bicarbonate SIX’ indications of sodium bicarbonate after ABG Arterial pH ≤ 7.0 Serum HCO3 ≤ 5 mmol/L Imminent cardiovascular collapse /shock Coma Life threatening hyperkalemia Severe lactic acidosis complicating DKA Laboratory tests follow up Blood tests for glucose every 1-2 h until patient is stable, then every 6 h Serum electrolyte determinations every 1-2 h until patient is stable, then every 4-6 h Initial blood urea nitrogen (BUN) Initial arterial blood gas (ABG) measurements, followed with bicarbonate as necessary Complications of DKA The recovery pattern may be slow to come but complications like cerebral oedema, arrhythmias stroke, infarction, aspiration, infection and sepsis may hinder the recovery to cause death in some patients. Mortality (5-10%) Remember clinical clues Monitor blood pressure, pulse, respirations, mental status, fluid intake and output every 1–4 h. Update DKA is a thrombotic state DKA can precipitate stroke Stroke can precipitate DKA DKA in pregnancy- points to note with pregestational, insulin dependent diabetes Foetal loss – 50 % Maternal loss - 1 % Proper antibiotic choice Labour may precipitate DKA Paediatric DKA 0.05 units /kg insulin ideal to rehydrate in 36 hours than 24 fours initial resuscitation with 20 ml/kg of 0.9 % NS 0.45% saline avoids cerebral edema SC lispro suggested Hyperglycemic hyperosmolar syndrome Some insulin – no ketosis, no acidosis Less common Coma Hyper osmolarity , RBS 500- 600 10 liters or more Its is ideal to switch to half normal saline if either the osmolality or sodium is high. No urgent insulin Hypoglycemia: In practice, hypoglycemia is generally defined as a blood glucose level < 60 mg/dl. A definitive diagnosis Whipple’s triad: 1. Symptoms compatible with hypoglycaemia 2. A low plasma glucose concentration 3. Relief of symptoms after plasma glucose is raised. Why important Brain needs glucose It cant synthesize glucose We cant let it starved of glucose for even a few minutes 40 or 50 or 60 or 70??? Arterial plasma 10 % higher than venous. Fasting ok but pp no good. Whole blood (finger pricks) 10% lower!! High hematocrit – venous-arterial gap is more. Incidence of hypo Type 2 without insulin : 4-10 /patient/year Type 2 on insulin : 16 /patient/year Type 1 : 40 episodes /patient/year What happens if sugar decreases ?? approx 80 mg Decreased insulin secretion Approx 70 mg Increased glucagon Approx 65 mg Increased epinephrine Approx 55-65 – Cortisol & growth hormone (Noncritical) Less than 55 - cognition affected Symptoms Autonomic neuroglycopenic Palpitation headache Sweats fatigue Anxiety mental dullness Tremors vision blurring Tachycardia confusion Hypertension amnesia Nausea ,hunger seizure,coma Risk factors Use of insulin secretagogues ( sulphonyl ureas) insulin therapy Missed or irregular meals Advanced age Duration of diabetes, strict control Impaired awareness of hypoglycemia Autonomic failure, beta blockers DPP 4 inhibitors – less incidence In insulin patients !! The depth of needle Exercising limb Hot bath after injection Bigger size needle Type of insulin Glargine and detemir - less hypoglycemia Potentially hypoglycemic combines Aspirin - dec. insulin resistance Quinine – inc. insulin secretion. Tetracyclics - inc. insulin secretion Gatifloxacin - inc. insulin secretion Beta blockers- interact hepatic gluconeo Fibrates – sensitivity to insulin Fluoxetine -stimulate beta cells And a few others. Other diseases – prone for hypos Adrenal Gastrointestinal Hepatic Renal Dementia sepsis Categories of hypoglyemia Mild : 55-70 mg pallor,sweats,palpitation Moderate : 45-55 mg- headache,vertigo,mood changes Severe : < 45 mg. Conscious status? Treatment Mild : 15 grams glucose = increase 18 mg- 18 min 4 cubes sugar 2 spoons honey 150 ml fruit juice Chocolate ,milk ,cereal bars – some sweets are not good Moderate: 20 -25 grams Sulphonyl ureas induced hypos – prolonged , Observe and give snacks Severe – what is it?? Patient needs someone’s help 50 ml of 25 % dextrose IV –------- 2cc/kg-10% - infants 2cc/kg – 25% - adolescents 2cc/kg - 50% - adults See that the vein is free flowing – other wise risk of necrosis Some antidiabetics Acarbose - alpha glucosidase inhibitor So only glucose should be given Miglitol -- sometimes even glucose may be refractory Treatment continuum Measure blood sugar ,Assess conscious status Maintain vitals, Start 10 % dextrose solution 1 mg glucagon IM or SC Look for precipitating factors-alcohol Assess for liver status,renal status, Serum insulin, c peptide, epinephrine, cortisol TSH, growth hormones etc,etc….. Sulfonyl urea overdose Inj. Octretide 50 µgm SC can be repeated 8 hrly Refractory unconscious state – can be cerebral edema IV mannitol and dexa 10 mg to be considered Summary I hope the lecture was pushed into your brains Diabetic emergencies –update and controversies Or atleast the picture Thank you all