21-renal physiology
advertisement

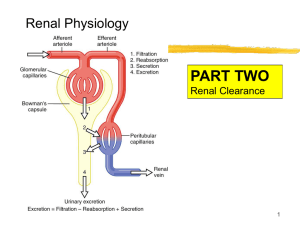
Renal Physiology- Chapter 27 Basic Mechanisms of Urine Formation Filtration, secretion, reabsorption and excretion. How do we determine these rates? Master formula 1 Renal Equations (for lab exercise) For any substance, The rate of excretion = rate of + filtration rate of – secretion rate of reabsorption Other terms that are used to express these ideas: •For “Rate of excretion” we often use the term “urinary output” •For “Rate of filtration,” when referring to filtered fluid, we often use the term GFR if referring to filtered solute, we use Tubular Load 2 Calculating Tubular Load of a Substance (any solute, “s”) At the glomerulus, fluid and solutes are constantly being filtered and enter the tubule. GFR is the term for the volume of plasma fluid filtered each minute. Once in the tubule, it is “tubular fluid” and no longer plasma, but not yet urine Tubular Load (TLs): the amount of any substance (s) entering the tubule, each minute. TL depends on two things: the plasma concentration and the rate of filtration of that solute TL s = Ps x GFR 3 Tubular Filtrate Resembles Plasma By far, filtered fluid is mainly NaCl and water. It contains other salts and electrolytes, amino acids, small sugars, vitamins and other small molecules, such as wastes. Na+ and Cl- are present in such large amts; they are over 99% reabsorbed along the length of the tubule. (Why? Remember that plasma volume affects blood pressure) Reabsorption of other solutes, like amino acids and sugars, is often linked to the transport of Na+ 4 Luminal Membrane Note: this side contains microvilli in PCT. Filtrate arriving from Bowman’s Capsule Basolateral Membranes Tubular Cells Peritubular Capillaries Tubular Lumen The PCT has an extensively amplified apical membrane called the brush border and its basolateral membrane is highly invaginated and contains many mitochondria 5 Transport: Active (primary or Tubular Reabsorption secondary) and Diffusion Many different solutes are reabsorbed by various transport methods As a result of solute reabsorption, osmosis will occur As a result, water movement from the tubule will affect the gradients of other solutes still in the tubule, and if they are permeable, their reabsorption. Figure 27-1; Guyton and Hall 6 3 modes of net reabsorption + Primary Active Transport of Na of sodium Sodium/Potassium ATPase Facilitated diffusion/ Secondary active transport on apical membrane Simple diffusion Bulk flow into peritubular capillary Figure 27-2; Guyton and Hall 7 Mechanisms of Secondary Active Transport Across the luminal membrane: Co-transport of Na+ Glucose Na+ Amino Acids. Na+ H+ Counter-transport (Exchange) • Across the basolateral membranes: glucose and amino acids diffuse out to peritubular capillaries (they are permeable there) but Na must be actively transported out of the cell by Na/K pump. Figure 27-3; Guyton and Hall 8 Transport Maximum Figure 27-4; Guyton and Hall Some substances have a maximum rate of tubular transport due to saturation of carriers, limited ATP, etc. • Transport Maximum (Tm): Once the transport maximum is reached for all nephrons, further increases in tubular load are not reabsorbed, but are then excreted. • Threshold is the plasma concentration at which tubular load just exceeds the transport maximum (Tm) for reabsorption, where below threshold all solute molecules are reabsorbed, and above threshold, some solutes are not Examples: glucose, amino acids, phosphate, sulfate 9 =solute = transporter 5/min 1 2 3 4 5 Transport maximum is reached when carriers are saturated. 10 =solute = transporter 5/min 1 2 3 4 Excretion 5 Saturation is reached, Maximum speed, Tm 11 A patient with uncontrolled diabetes has a GFR of 90 ml/min, a plasma glucose of 200 mg/dl (2mg/ml), and a transport max (Tm) shown in the figure. What is the glucose excretion for this patient? 250 (mg/min) 200 Glucose a. 0 mg/min b. 30 mg/min c. 60 mg/min d. 90 mg/min e. 120 mg/min Transport Maximum (150 mg/min) Reabsorbed 150 100 Excreted . Threshold 50 0 50 100 150 200 250 300 350 Filtered Load of Glucose (mg/min) Copyright © 2006 by Elsevier, Inc. 12 Answer: Filt Glu = (GFR x PGlu) = (90 x 2) = 180 mg/min Reabs Glu = T max = 150 mg/min Excret Glu = 30 mg/min 250 GFR = 90 ml/min PGlu = 2 mg/ml Tmax = 150 mg/min (mg/min) 200 Glucose a. 0 mg/min b. 30 mg/min c. 60 mg/min d. 90 mg/min e. 120 mg/min Transport Maximum (150 mg/min) Reabsorbed 150 100 Excreted . Threshold 50 0 50 100 150 200 250 300 350 Filtered Load of Glucose Copyright © 2006 by Elsevier, Inc. (mg/min) 13 Make sure you understand that Reabsorption of Water and Solutes is Coupled to Na+ Reabsorption in the PCT Interstitial Fluid K+ - 70 mV ATP Na + Tubular Cells Na + ATP 0 mv Copyright © 2006 by Elsevier, Inc. K+ Tubular Lumen H+ Na + glucose, amino acids Na + Urea H20 Na + Cl- - 3 mV 14 Changes in Concentration in Proximal Tubule Special feature of PCT: is freely permeable to water As a result of solute reabsorption, osmosis will occur Isosmotic reabsorption…what does that mean? Define. (300mOsm) As a result, water movement from the tubule will affect the gradients of other solutes still in the tubule, and if they are permeable, their reabsorption. ~100% Glucose and Amino Acids 67% of Filtered Sodium 65% of Filtered Water What happens to a solute concentration in the tubule if it is reabsorbed more than water? or less than water? Figure 27-7; Guyton and Hall 15 Before we move onto the other nephron segments be mindful of the following: The kidneys must be able to excrete urine that is either hypo-osmotic or hyper-osmotic with respect to bodily fluids This means that the varying osmolality requires that solute be separated from water at some point along the nephron! The loop of Henle, in particular the thick ascending limb, is the MAJOR site where solute and water are separated. Thus the excretion of both dilute and concentrated urine requires normal function of the loop of Henle 16 LOH- Thin Descending limb permeable to water AQP-1 water channels ??? of filtered water reabsorbed here No active sodium transport minimal permeability to sodium and urea (simple diffusion INTO the tubule only 110% of urea) 17 Thick- Ascending limb—Diluting Segment!!!! Actively pumps sodium out of tubule to surrounding interstitial fluid (Na+/K+ ATPase) Na+/2 Cl-/K+ co-transporter on luminal side Na+/H+ counter-transport (H+ secretion) Also, Ca+2, HCO3-, Mg+2, K+, and Na+ paracellularly due to positive net charge in lumen from backflow of K+ Impermeable to water About ??? of sodium reabsorption Fluid leaving thick ascending limb is hypoosmotic 18 Sodium Chloride and Potassium Transport in Thick Ascending Loop of Henle Figure 27-9; Guyton and Hall 19 Look at properties of cells along tubule: Cells of tubules are NOT permeable to water. Water can’t go in or out. Cells of tubules actively reabsorb Na+ and Cl-(out of tubule and into surrounding area). Salt is removed but NOT water. Interstitial space becomes highly concentrated! This makes filtrate more dilute and osmolality decreases. 400 20 Purpose of the LOH- Counter Current Multiplier to create an osmotic gradient deep in medulla of kidney, not for its own benefit, but to benefit the collecting duct that sits adjacent to it. Creates “salt gradient.” If Loop is disabled, then collecting duct adjacent to it cannot give concentrated urine. Concentration and volume of urine is determined by concentration gradient produced in Loop of Henle and by the presence of certain hormones. Urine concentration can then range from 50 mOsmolal to 1400 mOsmolal. Let’s write in the osmolalities for the filtrate in the descending and ascending tubules 300 300 700 700 1000 1000 12000 21 Factors That Contribute to Buildup of Solute in Renal Medulla Countercurrent Multiplier Active transport of Na+, Cl-, K+ and other ions from thick ascending loop of Henle into medullary interstitium Active transport of ions from medullary collecting ducts into interstitium Passive diffusion of urea from medullary collecting ducts into interstitium Diffusion of only small amounts of water into medullary interstitium– most absorbed in PCT. “sluggish blood” 22 Characteristics of Early and Late Distal Tubules and Collecting Tubules • not permeable to H2O • not permeable to urea Juxtaglomerular apparatus • permeability to H2O depends on hormones • not permeable to urea Figure 27-11; Guyton and Hall 23 DCT- early associated with Juxtaglomerular apparatus (helps in tubuloglomerular feedback mechanism for GFR) Mesangial cells: smooth muscle like properties, structural support, phagocytic activity, secrete prostaglandins Granular cells of the afferent arteriole- makes renin Macula densa of DCTchemoreceptors Functionally similar to thick ascending loop Not permeable to water (still diluting segment) nor urea Active reabsorption of Na+, Cl-, K+, Mg++ Thiazide diuretics affect Na/Cl cotransporter 24 Late DCT, connecting tubule Principal cells: what do they do? No urea permeability K+ sparing diuretics work here Antagonists to aldosterone binding sites Sodium channel blockers (reduces K+) Water reabsorption dependent on hormones 25 Intercalated Cells what do they do? Intercalated Cells Tubular Lumen H20 (depends on hormones) H+ K+ K+ ATP ATP Na + K+ H+ ATP ATP ATP Cl 26 Copyright © 2006 by Elsevier, Inc. Medullary Collecting Ducts Permeable to urea goes back to ALOH Can reabsorb more water (ADH dependent)- to be discussed later! important for determining final urine output Can secrete hydrogen ions. 27 Concentration of Different Substances in Tubular System • Concentrations of solutes depend on relative reabsorption of the solutes compared to water. • if water is reabsorbed to a greater extent than the solute, the solute will become more concentrated in the tubule (e.g., creatinine, inulin) • if water is reabsorbed to a lesser extent than the solute, the solute will become less concentrated in the tubule (e.g., glucose, amino acids) Figure 27-14; Guyton and Hall 28 Peritubular Capillary Net reabsorption forces Figure 27-15; Guyton and Hall 29 Determinants of Peritubular Capillary Hydrostatic Pressure Glomerular Capillary Ra Peritubular Re Capillary Arterial Pressure Arterial Pressure Ra Re Pc Pc Pc 30 We’ve covered filtration and reabsorption….Now, it’s time for Tubular Secretion First step is simple diffusion from peritubular capillaries to interstitial fluid Enter to tubular cell can be active or passive Exit from tubular cell to lumen can be active or passive Examples: potassium, hydrogen, organic acids, organic bases, NH3 H+, K+, NH3 Organic acids and bases Secretion = Excretion – Filtration+ reabsorption (0)31