003 Lect 3 Reabsorption Secretion
advertisement

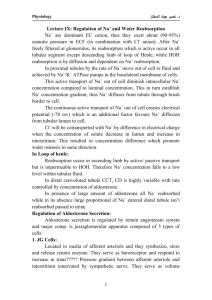
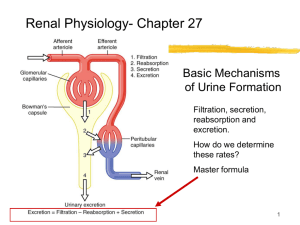
RENAL SYSTEM PHYSIOLOGY Dr Shahab Shaikh PhD, MD Lecture – 3: Tubular Reabsorption - I •••••••••••••••••••••••••••••••••• College of Medicine Al Maarefa Colleges of Science & Technology OBJECTIVES • Qualitatively describe the forces that determine movement of reabsorbed fluid from interstitium into peritubular capillaries. • State the major characteristics of the proximal-tubular systems for active reabsorption of organic nutrients. • Understand pressure natriuresis, pressure diuresis and osmotic diuresis. • List the approximate percentages of the filtered load of sodium reabsorbed by the various tubular segments. • Understand the active step of sodium reabsorption in all sodium-reabsorbing segments. • Understand the mechanisms of water reabsorption. • Understand the water permeability characteristics of each tubular segment. • Understand the maximum urinary osmolarity. • Define obligatory water loss, and understand its determinants. Urine Formation • Three Basic Mechanisms (Renal Processes) of Urine Formation include: 1.Glomerular filtration - GF 2.Tubular reabsorption - TR 3.Tubular secretion - TS 3 Urine Formation • Thus Urinary Excretion is total sum of the three processess: Urinary excretion = Glomerular filtration - Tubular reabsorption + Tubular secretion WHERE & HOW Tubular Reabsorption • Reabsorption – It is return of most of the filtered water and many solutes to the bloodstream. • Water, Essential substances and electrolytes needed by the body are reabsorbed but waste products are eliminated . • Reabsorbed substances carried by the peritubular capillaries to the venous system. • Tubular reabsorption is highly selective process. • Both active and passive processes are involved in Reabsorption. • GFR is 125ml/min, out of this 124ml/min is reabsorbed. Only 1ml/min excreted. – 99% of water is reabsorbed. – 99.5% Na+ is reabsorbed. – 100% glucose is reabsorbed. 5 Tubular Reabsorption Steps in Tubular Reabsorption: – Substance must leave tubular fluid by crossing luminal membrane of tubular cell. – Substance must pass through one side of tubular cell to the other. – Substance must cross basolateral membrane of tubular cell to enter interstitial fluid. – Substance must diffuse through the interstial fluid. – It must penetrate the capillary wall to enter blood plasma. 6 Tubular Reabsorption Routes for Tubular Reabsorption: • Reabsorption occurs either via the tubular cells ‘the transcellular route’ or between the cells ‘the paracellular route’. • The reabsorption and secretion that occur via the transcellular route are largely the result of active transport of solutes by the tubular cells. • Paracellular reabsorption is passive and occurs as a result of concentration or electrical gradients that favor movement of solutes out of the tubular fluid. 7 Tubular Reabsorption • Passive Reabsorption occurs from tubular lumen to the plasma, when no energy is spent. Movement occurs due to electro-chemical or osmotic gradient. • Active Reabsorption is, when energy is required for trans epithelial transport i.e. when there is movement of substance from tubular lumen to plasma against electro chemical gradient. e.g. Na+ , Glucose, Amino acid, Phosphate (PO4-3) – Primary active transport • E.g. Sodium-potassium pumps in basolateral membrane. – Secondary active transport • E.g. co-transport (glucose, amino acids) • E.g. counter-transport (K+, H+) 8 Tubular Reabsorption Transport Mechanisms used: 9 Tubular Reabsorption Transport Mechanisms used: 10 Tubular Reabsorption Transport Mechanisms used: 11 Tubular Reabsorption Transport Mechanisms used: 12 13 Role of Different Parts of Nephron Reabsorption and Secretion : Tubular Reabsorption Proximal Convoluted Tubule Role in Reabsorption • GFR delivers ~125ml/min of filtered plasma to the Proximal tubule. • Nearly 65 - % of this volume is reabsorbed by the proximal convoluted tubule and returned back to the blood. • Needed products such as glucose and amino acids are reabsorbed 100% rapidly. • Other products are slowly reabsorbed such as Urea or not at all such as Creatinine. • Proximal tubule also secretes some substances that the body needs to get rid of rapidly. These include toxins and drugs. 14 Proximal Convoluted Tubule Role in Reabsorption Common Substances Reabsorbed in PCT: – – – – – – – – Sodium Chloride Glucose Water Amino acid Bicarbonate Phosphate Urea 65% 50% 100% 65% 100% 90% 15 Proximal Convoluted Tubule Role in Reabsorption • Cells of the Proximal Convoluted Tubule (PCT): – The Simple Cuboidal cells of the PCT are called Brush Border cells because of their numerous Microvilli, which project into the lumen of the tubule. Mitochondria Lumen Interstitial space Basolateral membrane Luminal membrane Tight junction Microvilli 16 Loop of Henle Role in Reabsorption • The loop of Henle consists of three functionally distinct segments: – The thin descending segment – The thin ascending segment – The thick ascending segment • The descending limb of the loop is highly permeable to water • While the ascending limb, including both the thin and the thick portions, is virtually impermeable to water. • This characteristic of the loop is important for concentrating the urine. 17 Loop of Henle Role in Reabsorption Descending Limb: • The descending part of the thin segment is highly permeable to water and moderately permeable to most solutes, including urea and sodium. • About 20 per cent of the filtered water is reabsorbed in the loop of Henle, and almost all of this occurs in the thin descending limb. • The thin descending limb does not reabsorb significant amounts of the solutes. 18 Loop of Henle Role in Reabsorption Ascending Limb: • The ascending limb, including both the thin and the thick portions, is virtually impermeable to water. • It absorbs mainly solutes: – Na+, Cl-, K+ active transport – Ca2+, Mg2+ passive transport – Na+- H+ Counter-transport • The thick ascending limb of the loop of Henle is the site of action of loop diuretics 19 Distal Convoluted Tubule - DCT Role in Reabsorption J-G Apparatus: • The very first portion of the distal tubule forms part of the juxtaglomerular complex that provides feedback control of GFR and blood flow in this same nephron. Early DCT: • • • • Na+ : symporter mediated Ca2+ : PTH mediated Cl- : diffusion Water : impermeable 20 Late DCT and Cortical Collecting Tubule Role in Reabsorption • The second half of the distal convoluted tubule and the subsequent cortical collecting tubule have similar functional characteristics. • They have two distinct cell types, the Principal cells and the Intercalated cells • Principal cells: • Intercalated cells: – Na+ : Aldosterone mediated – Ca2+ : PTH mediated – Water : ADH mediated – H2CO3 reabsorption – K+ reabsorption 21 Late DCT and Cortical Collecting Tubule Functional characteristics: Role in Reabsorption • The tubular membranes of both segments are almost completely impermeable to urea. • The rate of reabsorption of sodium ions in both the segments is controlled by hormones, especially aldosterone. • These segments secrete potassium ions into the tubular lumen, a process that is also controlled by aldosterone and by other factors. • The intercalated cells of these nephron segments avidly secrete hydrogen ions by an active hydrogen-ATPase mechanism. It can do so against a large concentration gradient, as much as 1000 to 1 in contrast to the relatively small gradient (4- to 10-fold) that can be achieved by secondary active secretion proximal tubule. Thus, the intercalated cells play a key role in acid-base regulation of the body. • The permeability of the these segments to water is controlled by the ADH also called vasopressin. In the absence of ADH, they are virtually impermeable to water. This plays an important role in controlling the 22 degree of dilution or concentration of the urine. Medullary Collecting Duct Role in Reabsorption • Although the medullary collecting ducts reabsorb less than 10 per cent of the filtered water and sodium, they are the final site for processing the urine. • The permeability of the medullary collecting duct to water is controlled by the level of ADH. • The medullary collecting duct is permeable to urea. • The medullary collecting duct is capable of secreting hydrogen ions against a large concentration gradient, as in the cortical collecting tubule. Thus, it also plays a key role in regulating acid-base balance. 23 Regulation of Tubular Reabsorption Mechanisms of regulation: • Glomerulotubular Balance – The Ability of the Tubules to Increase Reabsorption Rate in Response to Increased Tubular Load • Peritubular Capillary and Renal Interstitial Hydrostatic and colloid osmotic forces. – Reabsorption = Kf X Net reabsorptive force • Effect of Arterial Pressure on Urine Output – The Pressure-Natriuresis and – Pressure-Diuresis Mechanisms • Hormonal Control: – – – – – aldosterone angiotensin II antidiuretic hormone (ADH) natriuretic hormones (ANF) parathyroid hormone • Sympathetic Nervous System • Osmotic factors 24 Regulation of Tubular Reabsorption 25 Regulation of Tubular Reabsorption Pressure Natriuresis & Pressure Diuresis: • When the body contains too much extracellular fluid, the blood volume and arterial pressure Increases. The rising pressure in turn has a direct effect to cause the kidneys to excrete the excess extracellular fluid, thus returning the pressure back toward normal. • An increase in arterial pressure in the human of only a few millimeters of mercury can double renal output of water, which is called pressure diuresis, as well as double the output of salt, which is called pressure natriuresis. Osmotic Diuresis: • high rate of water excretion resulting from osmosis caused by the filtered solutes in lumen such as mannitol. 26 Tubular Reabsorption Some Major Substances Reabsorbed: – – – – – – – Sodium Water Glucose Amino acid Bicarbonate Phosphate Urea 27 Tubular Reabsorption - Sodium • 99.5% of filtered Na+ is reabsorbed back in the tubule. • Na+ is reabsorbed variedly throughout the tubule except descending limb of Loop of Henle as follows: • Proximal convoluted tubule • Loop of Henle (thick ascending limb) • Distal and Collecting Tubule 65 - 67% 25 % 8% • Na+ Reabsorption in proximal convoluted tubule helps in reabsorption of Water, glucose, amino acid, Cl-, Urea. • Na+ Reabsorption in DCT and CT (8%) is under control of hormone Aldosterone, thus plays a key role in regulating ECF volume, which is important in long-term control of arterial blood pressure. 28 Tubular Reabsorption - Sodium 29 Tubular Reabsorption - Sodium Na+ Reabsorption Mechanism: • Luminal side: Movement of Na+ from lumen to intracellular fluid by electrochemical gradient. • Basolateral membrane: Na+ - K+ ATPase (3 Na+ out/ 2 K+ in) Na+ leak out of the cell results in low intracellular Na+ concentration and osmolarity in the interstitial space. • Peritubular side: (Bulk flow) Movement of hyperosmotic fluid from interstitial space into peritubular capillaries. % Mechanism of Na+ entry Proximal tubule 65 Na+ K+ Pump Na+-H+ exchange, Na+ cotransport with AA & Glucose, Na+/H+-Cl/anion exchange Henle’s loop 25 1Na+-K+-2Cl cotransport Distal tubule ~5 Na+-Cl cotransport Late distal tubule & collecting duct ~4 Na+ channels Segment 30 Tubular Reabsorption - Sodium Substances Reabsorbed with Na+: 31 Tubular Reabsorption - Sodium Substances Reabsorbed with Na+: 32 Tubular Reabsorption - Sodium Renin–Angiotensin–Aldosterone system (RAAS) 33 Tubular Reabsorption - Sodium Control of Aldosterone Secretion By Na+ and K+ : The RAAS System • RAAS activity if abnormally increased can cause hypertension. • RAAS is also responsible for fluid retention and EDEMA occurring in congestive heart failure. • Angiotensin Converting Enzyme inhibitor – ACE inhibitor drugs are used for hypertension and congestive heart failure 34 Tubular Reabsorption - Sodium Role of ATERIAL NATRIURETIC PEPTIDE (ANP) in (Na+) Reabsorption: • Hormone ANP is Natriuretic i.e causes Na+ loss, therefore, decreases BP. • Site of production of ANP – Atria of heart. • Site of action of ANP – distal part of nephron (DCT and CT), causes decreased Na+ reabsorption, therefore, increased Na+ and water loss in urine. • Inhibits aldosterone secretion from adrenal cortex. • Inhibits renin secretion, therefore, has negative effect on RAAS. • Inhibits vasopressin secretion and its action, therefore causes decreased water reabsorption. • Dilates afferent arteriole and constricts efferent arteriole, therefore, increases GFR. 35 Tubular Reabsorption - Water • 99 – 99.7% water is reabsorbed • Average urine volume – 1 to 1.5 liter/day • Minimum urine needed per day to get rid of waste products 500ml/day. • Proximal convoluted tubule (PCT) – 60-70%. It is passive, due to osmotic gradient due to active reabsorption of solutes e.g. Na+ • Loop of Henle(Descending Limb) – 15% of water is reabsorbed. • DCT and CT – 20% of filtered water is reabsorbed. DCT – 5% water reabsorbed. CT – 15% water reabsorbed. • In DCT and CT, water is reabsorbed under the action of ADH (Anti-Diuretic Hormone) or Vasopressin. 36 Tubular Reabsorption - Water 37 Tubular Reabsorption - Water Mechanism of Action of ADH (Vasopressin): • In absence of ADH, collecting tubule epithelium is relatively impermeable to water. Diabetes Insipidus (DI): • occurs due to deficiency of ADH • Nephrogenic DI • occurs when V2 receptors in collecting tubule fail to respond to ADH. • Central DI • occurs due to deficiency of ADH • In both cases, person will pass dilute urine up to 22 liters/day 38 Regulation of Water Reabsorption 39 References • Human physiology by Lauralee Sherwood, 8th edition • Text Book Of Physiology by Guyton & Hall, 11th edition • Review of Medical Physiology by Ganong. 24th edition THANK YOU 41