BHS 116.3- Physiology III Date: 5/1/13 Notetaker: Vivien Yip Page
advertisement

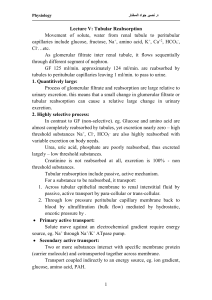
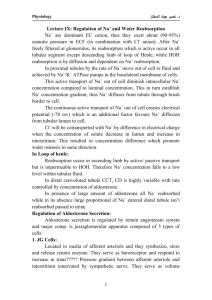
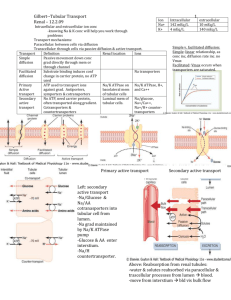
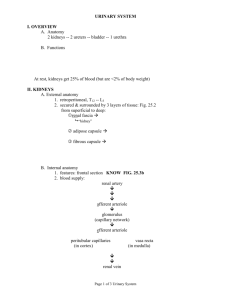
BHS 116.3- Physiology III Notetaker: Vivien Yip Date: 5/1/13 Page: 1 Not all inclusive - Approximately 70 questions - About 60-65% new material - About 20% from exams 1 & 2 on immunology (lecture 18 on vaccines will not be included) - About 10% from exam 3 on primarily renal with some reproductive physiology - 4-5 questions from presentation handouts (1 from each topic and maybe a 2 nd question from one of them) Final Exam Review Inflammation - cardinal signs: what they are, what do they mean acute and chronic: differences, cellular mechanisms innate immune system - physical barriers to infection: epithelial barrier (skin), mucus, saliva, tears phagocytic cells: macrophages, neutrophils NK cells: cytotoxicity Complement system: MAC Cytokines and plasma proteins: interferons, CRP Fever know major differences between innate vs adaptive adaptive immune system - antigen recognition molecules more specific type of immunity, longer lasting, greater degree of diversity b cell, t cell complement system - major system involved in attacking primarily bacteria and ab/ag complexes main complement protein: tend to get broken into a and b component “b” are opsonins, bind to membranes “a” act as cytokines to draw more leukocytes to the site, increase inflammatory response complement activation pathways - leads to formation of MAC, poke holes in target (bacteria or another type of cell) and kill that cell specific sequence involved in making those MAC, 3 pathways: alternative, classical, lectin pathways alternative: most different classical and lectin: pretty much identical all the way through w/ exception of initiation C1- classical, manose binding lectin – initiates lectin pathway antibodies - structure: 2 HC & 2LC both LC will be the same group gamma, delta, miu HC function: different isotypes, class switching distinct regions: variable will serve as antigen binding sites BHS 116.3- Physiology III Notetaker: Vivien Yip - Date: 5/1/13 Page: 2 constant: structural in nature lymphocyte maturation - B cell goes through specific maturation process, different from T cell maturation process B cell: express both IgM and IgD on surface in order to get full mature B cell all this is occurring in bone marrow for B cell T cell maturation process occurs in thymus once each of these reach maturity, it can leave its primary lymphocytic organ and migrate to lymph node, spleen, MALT (secondary lymph organ) where it encounters Ag for the first time T cell subsets - cytotoxic CD8+ helper CD4+ all T cells will have CD3+ Can further subdivide helper T cells into Th1 (primary helper T cell) and Th2 (found more in parasitic type infection) T cell activation CD4+ - 2 signals required first: MHC binding to T cell receptor second: CD8 of T cell binding to b7 on the APC then IL2 released can bind to IL2 receptor and trigger proliferation of T cell CD8+ activation - - infected cell that is phagocytosed by APC o expression of MHC I and MHC II initial signal: CD8+ binding to MHC I on APC CD4+ binding to MHC II o release cytokines, act as second signal for that CD8+ T cell o proliferate and activated other form is standard: MHC T cell receptor complex, followed by CD8 b7 complex effector function of CD4+ T cell - activating macrophages, many times they will phagocytose microbes but won’t be able to kill it CD4+ will help stimulate that process and allow it to kill the phagocytosed microbe activate and provide second signal for B cells – lead to class switching of antibody Ig Class change - only B cell activated by CD4 + T cell can class switch their type of antibody IgM is initial class if CD4+ T cell help, will allow for different isotypes effector function of CD8+ T cell - directly kill infected target cell stimulate lysis reaction and trigger apoptosis of infected cell primary vs secondary antibody responses BHS 116.3- Physiology III Notetaker: Vivien Yip - Date: 5/1/13 Page: 3 primary: frist time exposure to antigen, slower rxn, not very high stimulus, produce IgM, pool of memory cell against the antigen, if we encounter again, will get secondary response secondary response: greater, faster and produce IgG B cell activation - - T cell dependent (protein antigens), with CD4 help o CD4 can only present protein peptides to MHC to be recognized o utilize helper T cells to further stimulate activated B cell o provides 2nd signal for antibody class switch T cell independent (non protein antigens) o carbohydrates, nucleic acids, some instances lipids o does not utilize helper T cells to further stimulate B cell, no 2nd signal provided and no antibody class switch o weaker response o produce only IgM (secretory) Transplantation - 4 types: allogenic, xenogenic, autograft, isograft mechanism of rejection hypersensitivities - 4 primary types: 1: immediate, IgE mediated 2: IgM, IgG mediated, against a tissue antigen 3: immune complex, IgM or IgG bound to soluble antigen forming complex that triggers inflammation 4: only T cell mediated hypersensitivity reaction autoimmune diseases - classify according to: o systemic/organ specific o antibody mediated t cell mediated or both o mechanism: type of hypersensitivity rxn o MG, SLE, Scleroderma, Sjogren’s, Graves disease, Multiple sclerosis, Type I diabetes, Rheumatoid Arthritis, Hashimoto’s thyroiditis Urine Function - general process of urine formation filtration, reabsorption, secretion and combination of those 3 leads to amount of specific solute that is excreted in the urine GFR - hydrostatic, colloid osmotic forces both in glomerulus and bowman’s capsule how those things change w/ compression of afferent and efferent arteriole or dilation autoregulation of GFR and renal blood flow - myogenic BHS 116.3- Physiology III Notetaker: Vivien Yip - Date: 5/1/13 Page: 4 o both arterioles have smooth muscle o afferent has normal response to stretch o increase or decrease amount of blood flow in glomerulus tubuloglomerular feedback o JG cell and macula densa (MD) o depending on NaCl concentration in distal tubule that gets to MD o MD have chemoreceptors that sense NaCl, trigger JG cells to release renin there’s when low levels of NaCl Peritubular capillary and renal interstitial fluid physical forces - Pc, opposes capillary reabsorption Pif, favors capillary reabsorption πif favors capillary reabsorption πif opposes capillary reabsorption Proximal tubules - 2/3 of everything getting reabsorbed other regions have specific things going on, know what is absorbed or secreted o distal tubule and cortical collecting tubules principal cells: reabsorption of Na and by default water, secrete K+ back into renal tubules if we have too much K+ in blood intercalated cells: reabsorb bicarbonate and K+, secrete H+ (acidic condition) Aldosterone - direct effect on principal cells: increases Na+ reabsorption and K+ secretion Osmoreceptor ADH feedback - role in different osmolarities in blood high osmolarity in blood: want to reabsorb water to dilute, release ADH, acts on late distal tubule and cortical collecting tubules Summary of urine excretion - late distal tubule and collecting tubule are sensitive to ADH in the presence of ADH they will reabsorb water and produce a concentrated urine early distal tubule and thick ascending limb are always impermeable to water no matter what, reason why it’s called diluting segment absence of ADH, whole back end is impermeable to water get very dilute urine, not reabsorbing any water renal potassium excretion - greatest variation is due to secretion of potassium back in by principal cells calcium and phosphate handling - Ca++ majority is reabsorbed in proximal tubules, another area is in later portion of renal tubules o early distal or late distal (under PTH control will reabsorb if present) P, mostly reabsorbed along length of proximal tubule, in the presence of PTH the reabsorption is inhibited BHS 116.3- Physiology III Notetaker: Vivien Yip o Date: 5/1/13 Page: 5 PTH phosphate is excreted more Acid base regulation - - - - - fundamental mechanisms in which kidneys regulate ECF H+ conc: o secrete H+ o reabsorb filtered bicarbonate o production of new bicarbonate primary mechanism will be in proximal tubule: h+ secretion and bicarb reabsorption go hand in hand indirect reabsorption o not reabsorbing the filtered bicarbonate, processing it in epithelial cell and reabsorbing the newly created bicarbonate, getting 1:1 but not getting the same exact one that was filtered In early portion of tubules, we have Na+/H+ counter transport – secondary active, Na+ goes into renal epithelial cell, H+ is pumped out o get one bicarbonate reabsorbed Latter part of tubules: primary active transport of H+, if bicarb still remaining in tubules, will get indirect reabsorption o can get phosphate and create new bicarb in times of acidosis, will get more of the ammonia system playing a role, create a lot more bicarbonate when we involve ammonia system, kicks in only with acidotic conditions in the blood Renal clearance - Primary renal filtration rate is 125ml/minute what value means it is filtered reabsorbed or secreted = inulin, filtered not reabsorbed, not secreted <inulin, filtered, reabsorbed, secreted >inulin, filtered, not reabsorbed, secreted renal pathologies - - - - acute vs chronic primary acute type: acute glomerulonephritis 2 primary mechanisms, both involving autoimmunity o circulating immune complexes embedded in subepithelial or subendothelial tissue, complexes trigger inflammatory response o antibody binding to glomerular tissue: in capillary or basement membrane, trigger inflammatory reaction o know type II or III hypersensitivity rxn acute tublar necrosis o ischemic form: decreased oxygen delivered to renal epithelial cell, can get necrosis, focal type, sporadic, regions of necrosis and then regions of normal cell, form casts of necrotic debris that plug up tubules downstream o nephrotoxic: due to poisons, long regions of necrosis, plug up regions downstream chronic glomerular nephritis o if the offending agent is still around from acute glomerular nephritis o irreversible damage to nephron chronic obstructive pyelonephritis o usually superior and inferior poles of kidneys are destroyed o caused by UTI BHS 116.3- Physiology III Notetaker: Vivien Yip abnormal nephron function - due to loss of nephrons that is irreversible loss of water and electrolyte balance decreased waste product excretion uremia anemia osteomalacia Date: 5/1/13 Page: 6