Renal Physiology
advertisement

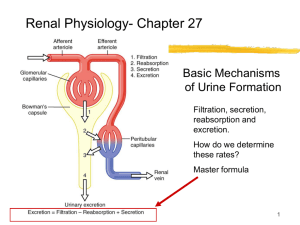
Renal Physiology PART TWO Renal Clearance 1 Basic Mechanisms of Urine Formation Filtration, secretion, reabsorption and excretion. How do we determine these rates? The master equation: Rate of excretion = filtration + secretion – reabsorption 2 TERMS Urinary output is a flow rate; how much urine are you producing per unit of time, ml/min This refers to the amount of urine dripping into the urinary bladder, not the amount voided. 3 TERMS Rate of filtration is the flow rate of plasma fluid going into Bowman’s capsule. This plasma fluid is called “filtrate”. The filtrate is not the same as plasma since there are no plasma proteins in it (proteins don’t get through the filtration membrane, not just because of their size, but also because of their negative charge). 4 TERMS Glomerular Filtration Rate (GFR) is the amount of fluid going into Bowman’s capsule per unit of time. Normal GFR is 90 - 120 mL/min Dissolved in that filtrate are electrolytes, glucose, and amino acids. We can also calculate how much of those molecules are entering Bowman’s capsule. 5 GFR z Glomerular filtration rate (GFR) can be calculated by measuring any chemical that has a steady level in the blood, and is freely filtered but neither reabsorbed nor secreted by the kidneys. 6 GFR z One such substance is creatinine. z To determine GFR from creatinine, collect urine for 24hours and draw blood before and after the 24-hour period. z Then measure the amount of creatinine that was removed from the blood during that time. Then apply the results to a formula to determine GFR. You do not need to do this for this class. On test questions, I will tell you what the patient’s GFR is. 7 TERMS Filtered Load (or Tubular Load) is the amount of a specific solute (electrolyte, glucose, or amino acid) dissolved in the fluid that enters Bowman’s capsule. There is an equation for this, but you have to know two things: Patient’s GFR Plasma concentration of that solute. To determine this, draw blood, place in spectrophotometer. TL s = Ps x GFR Filtrate vs. Solute If I had a cup and I filled it with 125ml of water, and then added one packet of Crystal light, how much fluid entered the cup? 125 ml. How much fluid (the filtrate) went into the cup is the GFR. If you know how much solute (Crystal light) went into the cup, you can calculate the filtered load. 9 How to calculate Tubular Load If we want to know how much glucose was filtered into the nephron, we need to know that person’s blood plasma glucose levels, and we would need to calculate their GFR (normal is 90120mL/min). Each individual solute will have its own tubular load calculation. TL glucose = Pglucose x GFR TL sodium = Psodium x GFR TL chloride = Pchloride x GFR Kidney Function and Aging With age, our filtration membranes deteriorate, and we also lose some of our glomeruli. With age, the permeability of our kidney membranes also declines, causing a decline in GFR. Thus, we have a decline of urine production, gradually over our lifetime. Some people age better than others with our skin, some age better with their GFR. Older people have to take a lower dosage of medicines that are excreted in the urine. 11 Solutes Suck! Sodium (Na+) is the most numerous of the solutes in our plasma. Remember, if solutes are being reabsorbed, water will come with it….solutes SUCK water! When salt is reabsorbed, water will be reabsorbed too. When salt is secreted, water is secreted too. 12 Solutes Suck! Some solutes are being reabsorbed, pulling water with them, but other solutes are not being reabsorbed, so they stay in the kidney tubules and are trying to keep water with them. If there are more particles being reabsorbed, the water will mostly be reabsorbed also. What will happen to the concentration of the particles in the tubule that are not being reabsorbed, while water is leaving? Their concentration in the tubule will go up. Those things that are not reabsorbed will leave the body. 13 Renal Equations For any substance, The rate of excretion (Urinary output) = rate of + filtration rate of – secretion rate of reabsorption (GFR or TL) Other terms that are used to express these ideas: •For “Rate of excretion” we often use the term “urinary output” •For “Rate of filtration,” when referring to filtered fluid, we often use the term GFR (glomerular filtration rate) if referring to filtered solute, we use TL (Tubular Load) 14 Calculating Tubular Load of a Substance (any solute, “s”) At the glomerulus, fluid and solutes (solids that were dissolved in the fluid) are constantly being filtered and enter the kidney tubules. GFR is the term for the volume of plasma fluid filtered each minute. Once in the tubule, it is “tubular fluid” and no longer plasma, but not yet urine. Tubular Load (TLs): the amount of any substance (s) entering the tubule, each minute. TL depends on two things: the plasma concentration of the solute and the rate of filtration of that solute TL s = Ps x GFR 15 Tubular Filtrate Resembles Plasma By far, filtered fluid is mainly NaCl and water. But it also contains other salts and electrolytes, amino acids, small sugars, vitamins and other small molecules, such as wastes. Na+ and Cl- are present in such large amounts; they are over 99% reabsorbed along the length of the tubule. (Why? We need it to keep our blood pressure up) At a constant GFR, as plasma concentration of a freely filtered substance rises, the tubular load of the substance rises in direct proportion to plasma concentration 16 Remember the route the fluid takes: Glomerulus Proximal convoluted tubule (PCT) Descending limb of LOH Ascending limb of LOH Convoluted tubule Collecting duct Proximal convoluted tubule Collecting duct Distal convoluted tubule Glomerulus Loop of Henle descending limb Loop of Henle, thick ascending limb Solutes are reabsorbed into the blood stream The next photo is of a Proximal Convoluted Tubule (PCT), just beyond the glomerulus. The lumen of the tubule contains the filtrate which leaked out of the capillaries and into the glomerulus, entered Bowman’s capsule, and has now arrived in the PCT. There are cells (tubular cells) lining the lumen of the PCT. The cells have proteins that allow some solutes to diffuse into the cell, and right back out cell, and into the peritubular capillaries that surround the PCT. In that way, solutes re-enter the blood stream. 19 Filtrate arriving from Bowman’s Capsule Peritubular Capillaries Tubular Cells Lumen of PCT 20 Peritubular capillaries 21 Proximal Convoluted Tubule PCT PCT 22 Proximal Convoluted Tubule Water will follow the solutes. The PCT is the biggest site for reabsorption of solutes (substances dissolved in water). 100% of glucose and amino acids are reabsorbed in the PCT. 67% of Na and water are reabsorbed here. If ADH levels are very high, most of the water will be reabsorbed in the PCT. Water reabsorption along the proximal convoluted tubule (PCT) occurs by osmosis resulting primarily from reabsorption of sodium 23 Proximal Convoluted Tubule In a state of acidosis, the PCT will secrete H+ ions. When the H+ ions are secreted, reabsorption of bicarbonate ions occurs at the same time. H+ ions are also secreted in the DCT, but bicarbonate cannot be reabsorbed there. 24 Pressures Because we drop off a lot of fluid (125 ml of filtrate) into Bowman’s capsule every minute, the water pressure in the peritubular capillary beds is low. Because proteins cannot get through, the osmotic force is very high here (proteins are trying to get in, but cannot). In the glomerulus, the forces favor fluid to leave the glomerulus and enter Bowman’s capsule. In the peritubular capillary bed, the forces favor the fluid to enter the capillary bed. 25 Solutes without transporters There are some solutes that cannot get through the tubular cell membranes because they have no protein transporters, so they become more concentrated in the tubular lumen. The concentration increases until they are forced to diffuse down their concentration gradient and then they can enter the tubular cells and be reabsorbed. One such solute is chloride (Cl-). 26 Active Transport Active transport, facilitative transport, and simple diffusion are all involved in renal clearance. It all starts in the membrane of the tubular cells, which have protein transporters that allow Na+, K+, glucose, and other substances to get through. This is called Active transport (it requires ATP, so it uses energy). 27 Glucose reabsorption Glucose and amino acids leave the tubule and enter the peritubular capillaries. That is reabsorption. When any substance leaves the bloodstream and enters the lumen of the kidney tubules, it is secretion. By adjusting reabsorption and secretion, your body adjusts its acid-base balance; if too many H+ ions were kept in the plasma, there is too much acid, and the H+ ions will start to be secreted more. 28 Transport Maximum When proteins are shuttling solutes, the rate of this shuttling has a maximum, called a transport max (Tm). If there are more solutes present than can be transported, the solutes will end up in your urine. There will be a point at which you can saturate these transporters. For instance, when your blood glucose levels are elevated because you have a problem making insulin or responding to insulin, then you will have an increase in glucose load in Bowman’s capsule. This excess filtered load will cause a spill of glucose into the urine. After the PCT, there are no more glucose transporters to reabsorb it. 320 mg/ml is the max rate to filter glucose. If you filter 125 mg/ml and reabsorbed 125 mg/ml, how much did you excrete? None. If you filter 375 mg/ml but reabsorb 320 mg/ml (transport maximum), 55 mg/ml is excreted 29 Threshold Transport maximum is the total transport maximum throughout all of the nephrons in the kidney. They do not all have the exact number and type of transporters. One single nephron might get to maximum and a tiny amount of glucose will appear in the urine. As more nephrons reach their maximum, more glucose will appear in the urine. That appearance of glucose in the urine before you reach the overall Tm of the kidney is called threshold. Threshold is the plasma concentration at which a substance begins to appear in the urine 30 =solute = transporter 5/min 1 2 3 4 5 Transport maximum is reached when carriers are saturated. 31 =solute = transporter 5/min Excretion 1 2 3 4 5 Transport maximum is reached when carriers are saturated. 32 Calculate Glucose Excretion Step 1: Calculate their filtered load: GFR x plasma glucose level 90ml/min x 2mg/ml Step 2: Determine reabsorption of glucose (maximum is 150mg/min). Step 3: Subtract 150 from 180, and that tells you their excretion. Filtration – reabsorption = Excretion Answer: 180 – 150 = 30 mg/min 33 A patient with uncontrolled diabetes has a GFR of 90 ml/min, a plasma glucose of 2mg/ml, and a transport max (Tm) shown in the figure. What is the glucose excretion for this patient? 250 (mg/min) 200 Glucose a. 0 mg/min b. 30 mg/min c. 60 mg/min d. 90 mg/min e. 120 mg/min Transport Maximum (150 mg/min) Reabsorbed 150 100 Excreted . Threshold 50 0 50 100 150 200 250 300 350 Filtered Load of Glucose (mg/min) Copyright © 2006 by Elsevier, Inc. 34 Answer: Filtration (GFR x Pglu) – reabsorption (Tmax) = Excretion 180 – 150 = 30 mg/min 250 GFR = 90 ml/min PGlu = 2 mg/ml Tmax = 150 mg/min (mg/min) 200 Glucose a. 0 mg/min b. 30 mg/min c. 60 mg/min d. 90 mg/min e. 120 mg/min Transport Maximum (150 mg/min) Reabsorbed 150 100 Excreted . Threshold 50 0 50 100 150 200 250 300 350 Filtered Load of Glucose Copyright © 2006 by Elsevier, Inc. (mg/min) 35 A patient with uncontrolled diabetes has a GFR of 90 ml/min, a plasma glucose of 2.33mg/ml, and a transport max (Tm) shown in the figure. What is the glucose excretion for this patient? 250 (mg/min) 200 Glucose a. 0 mg/min b. 30 mg/min c. 60 mg/min d. 90 mg/min e. 120 mg/min Transport Maximum (150 mg/min) Reabsorbed 150 100 Excreted . Threshold 50 0 50 100 150 200 250 300 350 Filtered Load of Glucose (mg/min) Copyright © 2006 by Elsevier, Inc. 36 Answer: Filtration (GFR x Pglu) – reabsorption (Tmax) = Excretion 210 – 150 = 60 mg/min 250 GFR = 90 ml/min PGlu = 2.33 mg/ml Tmax = 150 mg/min (mg/min) 200 Glucose a. 0 mg/min b. 30 mg/min c. 60 mg/min d. 90 mg/min e. 120 mg/min Transport Maximum (150 mg/min) Reabsorbed 150 100 Excreted . Threshold 50 0 50 100 150 200 250 300 350 Filtered Load of Glucose Copyright © 2006 by Elsevier, Inc. (mg/min) 37 Urea Urea is also reabsorbed in the PCT. This happens because its concentration in the tubule is high, so it diffuses down its concentration gradient, which means it will leave the tubule and enter the capillaries. This is an advantage because it is a particle, and it brings water with it. But urea is a waste product…how will we get rid of it? We will reabsorb it now and secrete it again further along in the nephron. By the time the reabsorbed urea travels in the vasa recta to the distal convoluted tubule, its concentration is higher in the bloodstream than it is in the tubule, so it diffuses back out of the capillaries and into the tubule to be excreted. The DCT is impermeable to water, so water does not follow it. 38 Salt concentration in the PCT As you go along the length of the PCT, the amino acids and glucose are reabsorbed, in addition to salt and water. The salt concentration in the filtrate stays the same as the blood plasma salt concentration. As we go through the rest of the nephron, the saltiness will diminish as it becomes more like urine and less like plasma. 39 Diuretics in the PCT cause diuresis by reducing net water reabsorption from the proximal convoluted tubule Some diuretics are “Potassium sparing” because they decrease potassium excretion Mannitol: potassium-sparing Lasix: not potassium-sparing 40 Diuresis in the PCT Diuresis means the person is excreting a lot of water. This is what happens in diabetes mellitus (and insipitus). It makes the person thirsty, so they drink a lot of water. However, that is not why they have diuresis. The reason for the diuresis is the large amount of glucose in the tubule draws water with it, since glucose is a particle. Thus, the large filtered load of glucose has an osmotic effect on the tubule 41 Summary of PCT functions Reabsorbs 2/3 of the salt and water Reabsorbs 100% of glucose and amino acids Reabsorbs 65% of potassium Reabsorbs 50% of urea Regulates pH in the filtrate Secretes creatinine (waste product after you eat protein) into the filtrate 42 Now we leave the PCT and enter the Loop of Henle Our kidneys are responsible for adjusting the urinary output. They are responsible for determining if you have a lot of urine which very dilute, or scant, concentrated urine. If you drink a lot of water, it will make your urine dilute (more water than solutes). If you are dehydrated, your urine will be concentrated (more solutes than water). Caffeine and alcohol are dehydrating, so they have the opposite effect of drinking water. They block antidiuretic hormone (ADH) too. 43 Before we move onto the Loop of Henle, be mindful of the following: How can you make a solution more concentrated? Take out water or add more solute. How can you make a solution less concentrated? Add water or take out more solute. Your kidneys play that game. To do that, we have to separate solutes and water. But how do we do that, since water follows particles? There are several parts of the nephron that are impermeable to water. 44 Loop of Henle Ascending limb Descending limb LOOP OF HENLE: Descending Limb Water is reabsorbed Na+ and urea are secreted What will your filtrate taste like here? We are removing water and adding salt. 46 Keep track of the water: 20% of water is reabsorbed in the descending limb, and 67% was reabsorbed in the PCT. That means a total of 87% of our filtered water has now been reabsorbed. The remaining 13% can be tapped into if your body needs it. If you are well hydrated, it will go into the toilet. If you are dehydrated, hormones will be needed farther along in the nephron in order to reabsorb more water. In the PCT, you have reabsorbed 50% of urea. Although it is a waste product, we use it to create an osmotic gradient to reabsorb glucose and other good solutes. Now, we want to get rid of the urea since we are done reabsorbing all the glucose. By the time the filtrate is at the tip of the LOH, all of the urea that had gone back into the blood will be secreted back into the lumen, plus some more. The descending limb contains 110% of the urea you initially filtered. 47 LOOP OF HENLE: Ascending Limb Impermeable to water, so no water is reabsorbed or secreted. Permeable to NaCl and urea: NaCl (or sodium and chloride separately) diffuses out of tubule (reabsorbed) Urea diffuses into tubule (secreted) 48 Saltiness in the LOH Now let’s take the LOH together: on the descending limb we have water leaving and salt entering the lumen. On the ascending limb, we have salt leaving, and no more water leaving the lumen. As it goes up the ascending limb, it is becoming more and more hypo-osmotic (less and less salty). At the top of the ascending limb, it tastes less salty than blood plasma. Now we leave the LOH and enter the distal convoluted tubule (DCT) 49 Distal convoluted tubule Early DCT Late DCT Early Distal Convoluted Tubule (DCT) Thiazide diuretics have their effect in the early distal convoluted tubule. A thiazide diuretic is one that blocks sodiumchloride channels, so that sodium cannot be reabsorbed, so water cannot be reabsorbed. This will cause water loss, which will lower blood pressure. 51 Distal Convoluted Tubule (DCT) 5% more sodium is reabsorbed The DCT activity can be influenced by hormones. If there are no hormones around, these cells don’t do anything; whatever is remaining in the lumen will go into the bladder. If there are no hormones, the last 13% of water and the last 3% of Na goes into the toilet. Anti-diuretic hormone (ADH) and aldosterone will cause more water and salt to be reabsorbed (raises blood pressure). 52 Distal Convoluted Tubule (DCT) Special cells in the DCT, called intercalated cells manage your acid-base balance, to secrete more H+. If you are in a state of acidosis (too much acid in your blood) because you drank alcohol, your intercalated cells will secrete more H+ to bring the pH back to normal. If you are in a state of alkalosis because you have been hyperventilating (breathing fast), will the intercalated cells increase H+ reabsorption or H+ secretion? Answer: increase H+ reabsorption. 53 We’ve covered filtration and reabsorption….Now, it’s time for Tubular Secretion Secretion = Excretion – Filtration+ reabsorption 54 Secretion Secretion is the opposite of reabsorption. Any time you see a solute going from the tubular cells and into the lumen, it is called secretion. Secreted substances end up in the urinary bladder. It happens by active transport. We secrete acids, bases, phosphates, excess potassium. Secretion works this way: solutes diffuse out of the peritubular capillary bed and into the tubular cells, then they enter lumen of the convoluted tubule. From there, they go out the collecting duct, and into the urinary bladder. 55 Long-Term Dehydration Compensations in a dehydrated person who is deprived of water for 36 hours include the following: increased plasma renin increased plasma ADH decreased concentration of plasma atrial natriuretic hormone (vasodilator made by the heart; increases diuresis) increased water permeability of the collecting duct decreased water permeability in the ascending loop of Henle 56 Hormones affecting the kidney Renin: released by kidney when blood pressure is too low ACE: Pulmonary capillary enzyme that responds to renin. When renin is elevated, it cleaves angiotensin I into angiotensin 2. Angiotensin II: causes blood vessel constriction to increase blood pressure. It also stimulates the release of aldosterone. Aldosterone: Secreted from the zona glomerulosa of the adrenal cortex. It increases blood pressure by increasing sodium reabsorption. It is primarily released due to elevated potassium levels. ADH: Promotes aquaporin insertion in the cell membranes of the tubules Aquaporin is a protein that allows water to pass through the cell membrane, to be absorbed out of the tubule. Atrial natriuretic peptide (ANP): heart hormone that promotes more diuresis and urine production to lower blood pressure. Adenosine: Macula densa use this to molecule to change the radius of the afferent arteriole. 57 Summary of What’s Going On Glomerulus Capillary hydrostatic pressure is very high here (about 60mmHg). Bowman’s capsule colloid osmotic pressure here is essentially zero 58 Summary of What’s Going On PCT part of the nephron normally reabsorbs the most water Site of sodium-glucose co-transport as well as sodium-amino acid co-transport Even though reabsorption is occurring, tubular fluid is isosmotic to plasma throughout the length of this region. Site of most potassium reabsorption when no aldosterone is present secretes hydrogen, is rich in carbonic anhydrase, and accounts for most bicarbonate reabsorption 59 Summary of What’s Going On Descending Limb allows secretion of sodium and urea and is permeable to water These are highly permeable to water, low permeability to solutes, and are considered diluting segments. 60 Summary of What’s Going On LOH have the maximally hyperosmotic fluid when ADH levels are high At the Tip of the LOH Tubular fluid here is always maximally hyperosmotic to plasma, and is not hormone sensitive 61 Summary of What’s Going On Thick ascending limb has the Na+/K+/Cl- co-transporter is sensitive to the diuretic furosemide (lasix). are impermeable to water, reabsorb solutes, and are considered diluting segments. 62 Summary of What’s Going On DCT Macula densa is found here is sensitive to sodium channel blockers like amiloride and aldosterone inhibitors Site of hormonally regulated potassium secretion The intercalated cells of this region secrete hydrogen, is rich in carbonic anhydrase, and makes “new” bicarbonate. 63 Summary of What’s Going On Collecting Duct have the maximally hyperosmotic fluid when ADH levels are high NOTE: Print the following slide and write notes on what is going in and what is coming out of each area of the nephron. 64 Glomerulus Early Distal convoluted tubule Bowman’s capsule Late Distal convoluted tubule Proximal convoluted tubule Collecting duct Descending limb Thick Ascending Limb Vasa recta Loop of Henle (tip) 65 Glomerulus Early Distal convoluted tubule Bowman’s capsule Macula densa is found here is sensitive to sodium channel blockers like amiloride and aldosterone inhibitors Site of hormonally regulated potassium secretion The intercalated cells of this region secrete hydrogen, rich in carbonic anhydrase, and makes “new” bicarbonate. Proximal convoluted tubule Descending limb Late Distal convoluted tubule allows secretion of sodium and urea and is permeable to water These are highly permeable to water, low permeability to solutes, and are considered diluting segments. Thick Ascending Limb Collecting duct have the maximally hyperosmotic fluid when ADH levels are high Vasa recta Loop of Henle (tip) has the Na+/K+/Cl- cotransporter is sensitive to the diuretic furosemide (lasix). are impermeable to water, reabsorb solutes, and are considered diluting segments. have the maximally hyperosmotic fluid when ADH levels are high At the tip: Tubular fluid here is always maximally 66 hyperosmotic to plasma, and is not hormone sensitive Early Distal convoluted tubule Glomerulus Capillary hydrostatic pressure is very high here (about 60mmHg). Bowman’s capsule Late Distal convoluted tubule colloid osmotic pressure here is essentially zero Vasa recta Proximal convoluted tubule Urea is also reabsorbed in the PCT. This happens because its concentration in the tubule is high, so it diffuses down its concentration gradient, which means it will leave the tubule and enter the capillaries. This is an advantage because it is a particle, and it brings water with it. But urea is a waste product…how will we get rid of it? We will reabsorb it now and secrete it again further along in the nephron. By the time the reabsorbed urea travels in the vasa recta to the distal convoluted tubule, its concentration is higher in the bloodstream than it is in the tubule, so it diffuses back out of the capillaries and into the tubule to be excreted. The DCT is impermeable to water, so water does not follow it. part of the nephron normally reabsorbs the most water Site of sodium-glucose cotransport as well as sodium-amino acid co-transport Even though reabsorption is occurring, tubular fluid is isosmotic to plasma throughout the length of this region. Site of most potassium reabsorption when no aldosterone is present secretes hydrogen, is rich in carbonic anhydrase, and accounts for most bicarbonate reabsorption Descending limb Thick Ascending Limb Loop of Henle (tip) Collecting duct 67 Clinical Correlations What are the symptoms of severe dehydration? 1. Disoriented 2. Falls unconscious 3. Measurable loss of weight during strenuous activity (water loss) 4. Blood pressure drops 68 Clinical Correlations A marathon runner becomes dehydrated during a race. 1. What will happen to their weight? 2. What will happen to blood volume? 3. What will happen to blood pressure? 4. What will happen to heart rate? 5. What will happen to their baroreceptors? 6. What will happen to sympathetic outflow? 69 Clinical Correlations A marathon runner becomes dehydrated during a race. 1. Weight goes down (water loss) 2. Blood volume decreases (water loss) 3. Blood pressure decreases (volume loss) 4. Heart rate increases (b/c of decreased BP) 5. Baroreceptors decrease firing (low BP) 6. Sympathetic outflow increases (to 70 compensate) Clinical Correlations A marathon runner becomes dehydrated during a race. 1. What will happen to their Renal blood flow (RBF)? 2. What will happen to their tubular load of sodium? 71 Clinical Correlations A marathon runner becomes dehydrated during a race. 1. Renal blood flow (RBF) will decrease The body does not want to lose more water 2. Tubular load of sodium will decrease Sodium is reabsorbed so water will come with it 72 Clinical Correlations A marathon runner becomes dehydrated during a race. 1. What hormones would compensate for this condition? These would all be elevated: Adenosine Renin Angiotensin II Aldosterone ADH 73 Clinical Correlations A marathon runner becomes dehydrated during a race. 1. What will be the urinary output? Low volume 2. What will be the urine concentration? High concentration 74 Clinical Correlations A marathon runner becomes dehydrated during a race and falls unconscious. 1. What type of shock is this? Hypovolemic shock 2. What is the treatment? I.V. saline/bicarbonate solution Giving saline will increase water retention Giving bicarbonate will reduce acidosis 75 Clinical Correlations A marathon runner becomes dehydrated during a race and falls unconscious. 1. Why do they have acidosis? Hypovolemic shock reduces oxygen delivered to tissues. Muscles without oxygen start to convert to anaerobic metabolism to get their ATP. The waste product of anaerobic metabolism is lactic acid. The buildup of lactic acid without the kidney 76 excreting it causes metabolic acidosis. Clinical Correlations January 12th, 2007, A 28 year-old mother of three from Sacramento decides to go on a radio program to compete in a contest called, “Hold your Wee for a Wii.” During this contest, contestants drank great volumes of plain water. She drank 6 liters in 2 hours (3 liters an hour). The maximum the kidney can filter is 1 liter an hour. After the contest, she called her co-workers to say she wasn’t coming to work because her head hurt so badly. Later she is found dead. 77 Clinical Correlations Drinking too much water changes the extracellular osmolality. When the plasma is too dilute (too much water, too few solutes), water will leave the bloodstream to enter the tissues, where there are more solutes (solutes SUCK!). Water will enter the tissues (intracellular body fluid compartment), including the brain. The excess water will cause the brain to swell. 78 Water moves through Compartments Intracellular water (or other fluid) is the watery substance inside a cell. Interstitial water (or other fluid) is the watery substance between cells. Extracellular water (or other fluid) is the watery substance that is outside of cells. Some of it may be interstitial, some may be in the blood, joints, CSF, etc. z The concentration of individual solutes (glucose, sodium, potassium, chloride) is different in intracellular fluid than it is in extracellular or interstitial fluid, but the total osmolarity (concentration of all the solutes combined) of the intracellular fluid, extracellular fluid, and interstitial and is the same. z Water can move from one compartment to another. It can be drawn out of the plasma to enter the interstitial compartment first, and then it may enter the cells. Water can also move from the cells to the interstitial compartment, then into the bloodstream. 79 Water/Salt Imbalance Problems Expansion: the body has retained too much water Contraction: the body has too little water Hypo-osmotic volume The water in the body has too much water, too few solutes Hyperosmotic volume The water in the body has too little water, too many solutes Isosmotic volume The water in the body has the proper balance of water and solutes. 80 Water/Salt Imbalance Problems Hypo-osmotic volume expansion Excessive water drinking; plasma osmolality is reduced from too much water, not enough solutes (hypo-osmotic) and the extracellular fluid (outside of cells) volume has increased (expansion). Hypo-osmotic volume contraction Excessive sweating; the person has lost a lot of salt, but has lost some water, too. They are dehydrated (contraction) and have low salt levels (hypo-osmotic). The water in the body has low osmolality due to loss of the salt. Hyperosmotic volume expansion High salt intake; there is too many solutes, water is retained, so the overall volume is increased (expansion), but there is a lot of salt, so osmolality is increased (hyperosmotic). Hyperosmotic volume contraction Dehydration; the person has lost a lot of water, so overall volume is decreased (contraction). The salt level has not changed, so that means 81 more salt dissolved in less water (hyperosmotic). Water/Salt Imbalance Problems Isosmotic Volume Contraction Diarrhea or burn victim; loss of water and solutes. Overall water/salt ratio is maintained (isosmotic), but person loses overall volume (contraction). Isosmotic Volume Expansion Salt Infusion; person receives an i.v. of normal saline (isosmotic), and overall volume of body fluid increases (expansion). 82 Water/Salt Imbalance Problems The same number of proteins remains in the blood, but water may increase or decrease. These volume changes therefore affect the protein concentrations in the blood. With more volume (expansion), protein concentrations decrease. With less volume (contraction), the protein concentrations increase. However, hematocrit is not always affected by blood volume changes. Small changes in volume affect the protein concentrations, but may not affect the hematocrit. 83 Hyperosmotic volume contraction Diabetes insipidus There would be elevated protein concentration but NO CHANGE in hematocrit with this condition 84 Hyperosmotic volume expansion Conn’s disease would cause this condition There would be decreased protein concentration and decreased hematocrit 85 Hypo-osmotic volume contraction Addison’s Disease would cause this condition There would be increased protein concentration and increased hematocrit 86 Hypo-osmotic volume expansion Syndrome of inappropriate ADH (excessive secretion of ADH) would cause this condition. Since too much ADH is present, water is kept in the body. There would be decreased protein concentration but NO CHANGE in hematocrit with this 87 Iso-osmotic volume expansion There would be decreased protein concentration and decreased hematocrit Infusion of a 0.9g% saline solution would cause this condition In these conditions there would be NO CHANGE in the intracellular volume nor osmolality 88 Iso-osmotic volume contraction Diarrhea or burns would cause this condition In these conditions there would be NO CHANGE in the intracellular volume nor osmolality There would be increased protein concentration and increased hematocrit 89 Water Imbalance category Condition Disorder Proteins Hct Drinking too much water Low Normal or inappropriate ADH Syndrome Hypo-osmotic volume expansion Excess water, low solutes Hypo-osmotic volume contraction Loss of water and salt Addison's disease High High Hyperosmotic volume expansion High salt intake Conn's disease Low Low Hyperosmotic volume contraction Loss of water, normal salt levels Diabetes insipidis High Normal Isosmotic volume expansion Increase in normal saline Normal saline iv Low Low Isosmotic volume contraction Loss of water and solutes, but water/salt is normal Diarrhea High High 90 Hypernatremia (excess sodium in the blood) Causes Hypovolemic Inadequate intake of water, typically in elderly or otherwise disabled patients who are unable to take in water as their thirst dictates. This is the most common cause of hypernatremia. Euvolemic Excessive excretion of water from the kidneys caused by diabetes insipidus, which involves either inadequate production of ADH or kidneys not responding to it. Hypervolemic Intake of a hypertonic fluid such as drinking seawater or receiving an i.v. of sodium bicarbonate after a vigorous resuscitation. Can also be caused by mineralocorticoid excess due to a disease state such as Conn's syndrome or Cushing's Disease 91 Hyponatremia (too little sodium in the blood) Causes excessive sweating persistent diarrhea overuse of diuretic drugs 92 Hypokalemia (low potassium in the blood) Mild hypokalemia Often without symptoms, although it may cause a small elevation of blood pressure, and can occasionally provoke cardiac arrhythmias. Moderate hypokalemia May cause muscular weakness, myalgia (muscle pain), and muscle cramps Severe hypokalemia May cause flaccid paralysis and hyporeflexia 93 Hypokalemia (low potassium in the blood) Causes Inadequate potassium intake (rare) Gastrointestinal loss (vomiting or diarrhea) Urinary loss Thiazide diuretics Alkalosis in the blood Disease states that cause high aldosterone levels Conn’s syndrome (hyperaldosteronism) Cushing's syndrome (excess cortisol binds to the Na+/K+ pumps, so it acts like aldosterone). 94 Hyperkalemia (high potassium in the blood) Extreme hyperkalemia is a medical emergency due to the risk of potentially fatal abnormal heart rhythms (arrhythmia). Symptoms include malaise (tired), palpitations and muscle weakness; mild hyperventilation may indicate a compensatory response to metabolic acidosis, which is one of the possible causes of hyperkalemia. Often, however, the problem is detected during screening blood tests for a medical disorder, or it only comes to medical attention after complications have developed, such as cardiac arrhythmia or sudden death. 95 Hyperglycemia and Hypoglycemia Glucose levels vary before and after meals, and at various times of day. Glucose in fasting adults should be 80 to 110 mg/dl. Above 126 mg/dl is hyperglycemia. Below 70 mg/dl is hypoglycemia. 96 Clinical Correlations Addison’s Disease Conn’s Disease Diabetes Mellitus Diabetes Insipidus Cushing’s Disease Know which of these diseases has hypernatremia, hypokalemia, hypo or hyperglycemia, etc. 97 Addison’s Disease Chronic adrenal insufficiency (low cortisol levels) Hyponatremia Hypoglycemia Hyperkalemia Possible death at times of extreme stress Addisonian crisis: low blood pressure coma 98 Conn’s Disease This is hyperaldosteronism. The person releases too much aldosterone, which increases sodium retention, so water follows, and hypertension results. Condition associated primarily with hypertension and mild hypernatremia and mild hypokalemia. No diabetogenic (glucose) problems. 99 Diabetes Mellitus Condition characterized by polyuria, glucosuria, polydipsia and ketonuria. Polyuria (frequent urination) Glucosuria (glucose in urine) Polydipsia (thirsty) Ketonuria (ketones in the urine) When insulin does not pull glucose into the body cells, it stays in high levels in the blood (hyperglycemia) and spills out in the urine (glucosuria). The body is starving, so it breaks down fat into fatty acids for energy, and ketones are the waste product. In small amounts, they are broken down in the liver, but in large amounts, they build up in the blood (ketoacidosis: lowers blood pH) and spill out into the urine (ketonuria). Starvation, fasting, prolonged vomiting, high protein diets, and low carbohydrate diets also cause this condition. 100 Diabetes Insipidus Condition characterized by polyuria and polydipsia, but not glucosuria. This is more like a disease of water loss (ADH is not produced). 101 Cushing’s Disease Hypernatremia Caused by lack of water in the blood, like dehydration. Hypokalemia (low potassium) Hyperglycemia (excess glucose) Diabetes mellitus Weight gain, particularly of the trunk and face with sparing of the limbs (central obesity), moon face, buffalo hump, and sometimes growth of facial hair. 102 K+ Na+ Glucose Addison's High Low Low Conn's Mild low Mild high Normal Diabetes Mellitus High Low High Diabetes Insipidus High High High Cushing's Low High High BP Low High Other Possible death at times of extreme stress Polyuria, glucosuria, polydipsia, ketonuria, ketoacidosis Polyuria, polydipsia only Diabetes (Polyuria, glucosuria, polydipsia, ketonuria), central obesity, moon face, buffalo hump, facial hair in women 103 Tests to assess kidney function BUN (Blood Urea Nitrogen or Urea Nitrogen) Creatinine BUN/Creatinine Ratio Calcium Sodium Potassium Chloride CO2 104 Tests to assess kidney function BUN (Blood Urea Nitrogen or Urea Nitrogen). This is the concentration of nitrogen (within urea) in the serum (but not in red blood cells). A waste product, derived from protein breakdown, produced in the liver and excreted by way of the kidneys. High values may mean that the kidneys are not working as well as they should. BUN is also elevated by blood loss, dehydration, high protein diets and/or strenuous exercise which may temporarily and artificially raise levels. A low BUN level may be the result of liver disease, a low protein diet, pregnancy, or drinking an extreme amount of water. 105 Tests to assess kidney function Creatinine. A waste product largely from muscle metabolism (breakdown). Concentration of creatinine in the blood depends upon the amount of muscle that you have and the ability of your kidneys to excrete creatinine. High values, especially with high BUN levels, may indicate problems with the kidneys. Low values are generally not considered significant. BUN/Creatinine Ratio - This ratio is sometimes used or diagnostic purposes. 106 Tests to assess kidney function Calcium. Calcium is one of the most important elements in the body. The parathyroid glands and the kidneys control the amount of calcium in the blood. The parathyroid gland is the main regulator of calcium in the body. Nearly all of the calcium in the body is found in bone (99%). The remaining 1% is very important for proper clotting, nerve, and cell and enzyme activity. An elevated calcium level can be due to medication (such as too much synthetic vitamin D), inherited disorders of calcium handling in the kidneys, bone disease, or excess parathyroid gland activity or vitamin D. Low calcium can be due to malnutrition, drugs and certain metabolic disorders. 107 Tests to assess kidney function Sodium. An electrolyte regulated by the kidneys and adrenal glands. This element plays an important role in the water/salt balance in your body. Potassium. Potassium is an electrolyte found primarily inside cells and must be controlled very carefully by the kidneys. Its role is to maintain water balance inside the cells and to help in the transmission of nerve impulses. A low potassium level can cause muscle weakness and heart problems. A high potassium level can be found in kidney disease or in over ingestion of potassium supplements. 108 Tests to assess kidney function Chloride. Chloride is an electrolyte regulated by the kidneys and adrenal glands. Chloride is important to the function of nerves, muscles, and cells. It is usually associated with a high or low level of sodium or potassium. Some drugs taken by prostate cancer patients such as estrogens and corticosteriods can cause increased chloride. CO2. Co2 levels reflects the acid status of your blood. Corticosteriods as well as kidney disease can be involved. 109