pubdoc_5_19505_1010

Physiology راتخملا داوج ريصن .د
Lecture V: Tubular Reabsorption
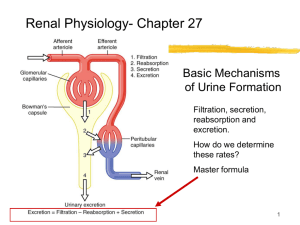
Movement of solute, water from renal tubule to peritubular capillaries include glucose, fructose, Na + , amino acid, K + , Ca +2 , HCO
3
,
Cl …etc.
As glomerular filtrate inter renal tubule, it flows sequentially through different segment of nephron.
GF 125 ml/min. approximately 124 ml/min. are reabsorbed by tubules to peritubular capillaries leaving 1 ml/min. to pass to urine.
1. Quantitively large:
Process of glomerular filtrate and reabsorption are large relative to urinary excretion. this means that a small change in glumerular filtrate or tubular reabsorption can cause a relative large change in urinary excretion.
2. Highly selective process:
In contrast to GF (non-selective). eg. Glucose and amino acid are almost completely reabsorbed by tubules, yet excretion nearly zero – high threshold substances Na + , Cl , HCO
3
are also highly reabsorbed with variable excretion on body needs.
Urea, uric acid, phosphate are poorly reabsorbed, thus excreted largely – low threshold substances.
Creatinine is not reabsorbed at all, excretion is 100% - non threshold substances.
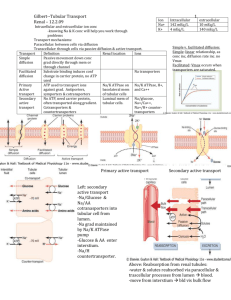
Tubular reabsorption include passive, active mechanism.
For a substance to be reabsorbed, it transport:
1.
Across tubular epithelial membrane to renal interstitial fluid by passive, active transport by para-cellular or trans-cellular.
2.
Through low pressure peritubular capillary membrane back to blood by ultrafiltration (bulk flow) mediated by hydrostatic, oncotic pressure by .
Primary active transport:
Solute move against an electrochemical gradient require energy source, eg. Na + through Na + /K + ATpase pump.
Secondary active transport:
Two or more substances interact with specific membrane protein
(carrier molecule) and cotransported together across membrane.
Transport coupled indirectly to an energy source, eg. ion gradient, glucose, amino acid, PAH.
1
Physiology راتخملا داوج ريصن .د
Passive transport:
Water diffuse from region of low solute concentration to high solute concentration when solute transported out of tubules, creates concentration gradient causes osmosis of water.
Cl is passively reabsorbed either because of –ve charge or Cl concentration gradient that developed when H2O is reabsorbed from tubules by osmosis. Thereby concentrating Cl in tubular lumen. Urea is also passively reabsorbed, after removal of water, urea concentration rises in tubular fluid creates concentration gradient between tubular fluid and blood peritubular capillaries.
Reabsorption along different parts of Nephron:
1. Proximal tubule:
65% of water, solute are reabsorbed in proximal tubule. This high capacity is due to:
1.
High concentration of mitochonderia Support potent active transport system.
2.
Extensive apical plasma membrane micovilli serve to expand surface area.
3.
High concentration of Na + contransporter on apical plasma membrane.
Loop of Henle:
Descending segment highly permeable to water, water rapidly reabsorbed from tubular fluid to interstitium, moderately permeable to solute (Na + , urea)
In thin and thick ascending segment
water permeability is zero, large amount of Na + , Cl , K + are reabsorbed causing tubular fluid becomes dilute as it flows back to cortex and at same time, active transport of Na + , Cl out of ascending limb to interstitial causes a high concentration of these ions in interstitial fluid of renal medulla. This mechanism for trapping NaCl and building up highly osmolarity of medulla called counter current multiplier essential for forming highly concentrated urine.
Distal and collecting tubule:
Na + /Cl are actively transport and permeability to water is under hormonal control (ADH/ Aldosterone).
2
Physiology راتخملا داوج ريصن .د
Regulation (Factor) of Reabsorption:
Because it is essential to maintain precise balance between tubular reabsorption and glomerular filtration, multiple nervous hormonal local control mechanisms are operated:
1.
Glomerulotubular balance: Tubules ability to increase reabsorption rate in response to increase tubular load.
2.
Increase arterial pressure: Decrease tubular reabsorption, increase renal excretion of Na + , water called pressure nitriuresis or pressure diuresis.
3.
Aldosterone: Increase Na + reabsorption and K + secretion.
4.
Angiotensin II: Increase Na + reabsorption directly and indirectly by aldosterone secretion.
5.
ADH: Increase water reabsorption in distal and collecting tubules.
6.
Parathyroid Hormone: Increase Ca +2 reabsorption, decrease PO
4
+2 reabsorption.
7.
Atrial natiruretic peptide: Decrease Na + reabsorption
increase excretion.
8.
Sympathetic nervous activity: Increase Na + reabsorption.
3