TPN - San Jose State University School of Nursing Spring 2008
advertisement

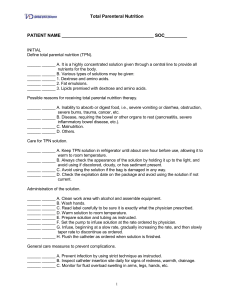
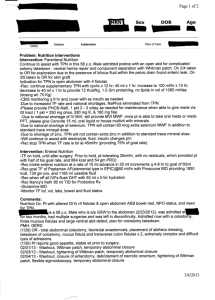
1 SAN JOSE STATE UNIVERSITY School of Nursing Nursing 155 Care of the Client Receiving Parenteral Nutrition KEY Independent Learning Activities Learning Outcomes 1. Describe the five typical components of a total parenteral nutrition (TPN) solution. 2. Identify five common clinical situations in which TPN might be used. 3. Identify common complications of TPN. 4. List nursing assessments or interventions that would help prevent, or treat, the following complications of TPN: infection, hypoglycemia, hyperglycemia, electrolyte imbalance, and air embolus 5. Describe types of patients who are likely to receive fat emulsion (lipids) in TPN. 6. Contrast peripheral parenteral nutrition (PPN) with TPN. 7. Describe nursing care for the client receiving TPN. 8. Discuss why TPN infusions are gradually increased to the target rate, and weaned slowly. TPN 2 Learning Activities 1. Briefly describe each of the 5 typical components of (TPN) solution listed below: Component What is it? Purpose Carbohydrates Dextrose 20% - 50% Provides majority of calories and energy needed to maintain physiologic function, metabolism of amino acids, and wound healing Protein Amino acids or protein hydrosylates Provides protein necessary for tissue building and wound healing Electrolytes Na+, K+, Cl-, magnesium, Ca++, Necessary to maintain physiologic function. Dosed according to Phosphate patient need. Trace elements Zinc, copper, manganese, cobalt, selenium, iodine Necessary to maintain physiologic function. Dosed according to patient need. Vitamins Added to 1 liter of TPN solution per day. Vitamin K and folic acid are given Necessary to maintain physiologic function. Dosed according to patient need. separately; they are not given IV 2. List 5 specific clinical situations in which TPN might be used. GI tract anomalies and Burns Chronic diarrhea and fistula vomiting Diverticulitis Failure to thrive GI obstruction Granulomatous enterocolitis Hypermetabolic states such as sepsis, or fractures Inflammatory bowel disease such as Crohn’s disease or ulcerative colitis Acute or chronic renal Malnutrition failure and reversible hepatic failure (extreme caution should be used in these cases) Pancreatitis Severe anorexia nervosa Short bowel syndrome Malabsorption TPN Complicated surgery or trauma Severe peptic ulcer disease 3 3. In each of the categories listed below, write 3 possible complications of TPN. a. Infection o fungus o gram-positive bacteria o gram-negative bacteria b. Metabolic problems o glucose metabolism: hyperglycemia, hypoglycemia, HHNK, glycosuria, osmotic diuresis, ketoacidosis o amino acid metabolism: serum amino acid imbalances, elevated serum ammonia, prerenal azotemia o essential fatty acid deficiency, o electrolyte and vitamin imbalances o trace mineral deficiencies c. Mechanical problems o insertion: air embolus, pneumo-, hemo-, or hydrothorax, hemorrhage o dislodgement o thrombosis of great vein o phlebitis 4. What nursing assessments or interventions would help prevent the following complications of TPN? a. Infection o assess for impaired immune status o refrigerate solution until 30 minutes before infusing o follow protocols for tubing and dressing changes o inspect the catheter insertion site for signs of inflammation and infection b. Hyper-, hypoglycemia, electrolyte imbalances o monitor for signs/symptoms hyperglycemia: thirst, polyuria, confusion, elevated fasting blood glucose, blurred vision, dizziness, nausea and vomiting, dehydration, Kussmaul respirations o monitor for signs/symptoms hypoglycemia: sweating, hunger, weakness, tremors TPN 4 o monitor serum electrolytes daily until stable o hyperkalemia: muscle weakness, flaccid paralysis, cardiac arrhythmias, abdominal cramps, diarrhea o monitor for hypokalemia: general weakness, decreased muscle tone, weak or irregular pulse, low blood pressure, shallow respirations, abdominal distention, ileus o check blood glucose Q4 hours o maintain accurate infusion rate: do not speed up or slow down infusion o check infusion frequently and use a pump o never increase or decrease flow rate by more than 10% o never stop TPN abruptly unless it is replaced by another glucose source c. Air embolus o place patient in Trendelenburg’s position when placing central venous catheter o instruct patient in Valsalva maneuver when catheter is inserted o use Trendelenburg’s position and Valsalva maneuver when changing tubing o monitor for signs of air embolus such as abnormal blood gases, cough, cyanosis, pain, anxiety, fatigue, respiratory rate and depth changes, altered chest excursion, shortness of breath o if embolism is suspected, place patient in Trendelenburg’s position on the left side o continue to observe for shock, cough, shortness of breath o notify physician immediately 5. Which patients would be likely to receive fat emulsion (lipids)? Fat emulsion would be used in: o patients receiving peripheral parenteral nutrition (PPN) who need additional calories, o patients receiving long-term parenteral nutrition who require a source of essential fatty acids, o patients receiving TPN who have high caloric needs. TPN 5 6. Contrast the differences between TPN and PPN by filling in the table. TPN PPN Concentration of dextrose: Concentration of dextrose: 20%-50% 20% maximum Method of administration: Method of administration: Central venous catheter, PICC line Large peripheral veins Indications for use: Indications for use: long-term nutritional support, the patient has high protein and caloric requirements, suitable peripheral veins are not available nutritional support is needed for only a short time (up to 2 weeks), protein and caloric requirements are not excessively high, risk of a central catheter is too great, nutritional support is used to supplement inadequate oral intake 7. List 5 nursing assessments or interventions for the client receiving TPN. o vital signs Q 4-8 in early therapy o monitor catheter insertion site for inflammation that may signal infection o change dressing and tubing according to agency policy o weigh daily initially, then weekly when the patient is stable o blood analysis that includes blood glucose, electrolytes, protein, complete blood count, and enzyme studies 3X/week until stable, then weekly 8. Why is TPN infused at a rate that gradually increases over 24 to 48 hours, and weaned slowly, as well? Infusing the solution slowly allows the pancreas time to adjust to the increased amount of glucose in circulating blood. Likewise, TPN should be weaned off slowly to give pancreatic islet cells time to adjust to the decreasing levels of glucose. TPN