Cyclic TPN - WordPress.com
advertisement

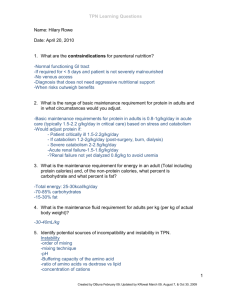
Done by : Fatimah Al-Shehri Pharmacy intern King Abdul-Aziz University Superviesd by : Dr.Asmaa Tahaa. - Introduction(Definition/indications/starting criteria/composition TPN ). - Clinical conditions warranting the use of TPN. - Types of TPN Infusion . - Cyclic versus continuous . - Advantages and disadvantages of both. - Monitoring . - Home TPN. - Case scenario. TPN is the administration of a nutritionally adequate hypertonic solution consisting of glucose, protein hydrolysates, minerals, and vitamins through an indwelling catheter into the superior vena cava or other main veins. Indications of TPN : - Inadequate absorption. - Gastrointestinal fistula. - Bowel obstruction. - Prolonged bowel rest. - Severe malnutrition. - Significant weight loss . - Hypoproteinaemia when enteral therapy is not possible. - Other disease states or conditions. Starting criteria: 1-If early EN is not feasible or available over the first 7 days after admission. More than 10% involuntary weight loss over a 2-3 months period. Less than 75% of ideal or usual body weight Serum prealbumin less than 10 mg/dl serum transferrin less than 100 mg/dl History of inadequate oral intake for more than 7 days . Composition of TPN solution: 1- Amino acids . 2-Dextrose . 3-Electrolytes. 4-Lipids. 5-Vitamines and minerals. DETERMINING ENERGY NEEDS: Normal/mild stress level: 20-25 kcal/kg/day Moderate stress level: 25-30 kcal/kg/day Severe stress level: 30-40 kcal/kg/day DETERMINE THE PROTEIN NEEDS: Usually start with 0.8 g/Kg and add stress and other factors as needed. Renal failure: Acute (severely malnourished or hypercatabolic): 1.5-1.8 g/kg/day Chronic, with dialysis: 1.2-1.3 g/kg/day Chronic, without dialysis: 0.6-0.8 g/kg/day Hepatic failure: Acute management when other treatments have failed: With encephalopathy: 0.6-1 g/kg/day Without encephalopathy: 1-1.5 g/kg/day Chronic encephalopathy: Use branch chain amino acid enriched diets only if unresponsive to pharmacotherapy AMOUNT OF FLUIDS THE PATIENT NEEDS: Methods to calculate fluid needs: 1-patients need a minimum of 30 cc fluid/Kg maintain hydration: 30-50 cc/Kg is a good amount to aim. 2- 100 cc free water/gram N intake + 1 cc/Kcal provided. 3- use 100 cc/Kg for first 10 Kg + 50 cc/Kg for the second 10 Kg. + 20 cc/Kg for each additional Kg. THE AMOUNT OF FAT NEEDED DEPENDS ON THE TOTAL ENERGY NEED 10%, 20% and 30% fat emulsion are available. 10% fat emulsion has 1.1 Kcal/cc 20% fat emulsion has 2.0 Kcal/cc 30% fat emulsion has 3.0 Kcal/cc CARBOHYDRATE IS THE MAIN SOURCE OF FUEL TO MEET ENERGY NEEDS: CHO is given as dextrose monohydrate, which yields 3.4 Kcal/gram. Condition: Suggested criteria: Hyperglycemia . Glucose >300mg/dL Azotemia. BUN >100mg/dL Hyperosmolarity. Serum osmolality >350mosm/kg Hypernatremia. Na>150mEq/L Hypokalemia. K<3mEq/L Hyperchloremic metabolic acidosis. Cl>115mEq/L Cl<85mEq/L. Hypochloremic metabolic alkalosis . Hypophosphatemia. Phosphorous <2mg/dL Continuous TPN . Cyclic TPN. Continuous TPN: Typically initiated over 24 hour (infusion). Advantages of continuous TPN: 1-Well tolerated by most patients. 2-Requires less manipulation. 3-Decreased nursing time. 4-Decreased potential for “touch” contamination. Disadvantages on long term : - Continuously connected to infusion equipment. - Interfere with daily activities. - Perpetually immobilize the patient. Cyclic TPN: It’s a type of TPN which administered on a cyclic, discontinuous Basis infusion usually over 10–14 hours . Indications : widely employed in patients who receive PN long term esp. patients on home health care settings. -It involves daily interruption of PN, allowing patients periodic freedom. - Improves quality of life. - Approximates normal physiology of intermittent feeding. -In hepatobiliary dysfunction switching to cyclic infusion when total bilirubin is between 5 and 20 mg/dL may lead to stabilization of bilirubin and liver function tests . NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #97 Carol Rees Parrish, R.D., M.S., Series Editor -It requires daily starting and stopping of infusions, during which time the body must adapt to changes in blood nutrients. -It requires higher nutrient infusion rates to supply a similar nutrient load over a shorter period of time. - Fluid overload esp. in cardiac and renal patients . -It may induce hypourecemia. -Daily starting and stopping of PN infusion may increase the risk of hyperglycemia and hypoglycemia. - Increased potential for touch contamination. - Increased nursing time. Practical Gastroenterology . July 2011 Items of comparison : Cyclic TPN : Nitrogen balance : Continuous TPN : Similar Daily lipid oxidation: Lower Higher Carbohydrate oxidation : Higher . Lower Triglyceride secretion : Similar Total Energy expenditure: Similar Oxygen consumption : Similar Items of comparison : Cyclic TPN : Continuous TPN : Urinary volume: Increased . - Excretion of urea, creatinine, Na, Cl, Ca, phosphate, Mg. Increased . - daily concentrations of calcium, phosphate, and vitamin D. Similar . Circulating concentrations of counter -regulatory Hormones. Similar insulin responses. Greater . - Critically ill, mechanically ventilated patients may not be candidates for cyclic PN infusion. Continuous and cyclic TPN in hospital. Monitoring patients receiving TPN: Fluid balance: Glucose tolerance: Weight: Venous access: Routine biochemistry: Monitor daily. Initially levels checked every 4-6 hours; daily when stable. Daily weights can show fluid changes. Venous access site regularly checked for signs of infection, phlebitis. Serum Na, K, urea and creatinine checked daily initially. Ca, Mg and P checked at least twice a week initially. Trace elements zinc, copper, selenium checked monthly. Vitamins B12, Folate, Vitamin A, Vitamin E checked monthly. Urinalysis Urinary levels of electrolytes useful when determining clinical significance of plasma levels. - Weight. - Blood sugar . - Temperature . - Intake and output. Documentation that the patients GIT is nonfunctional and this condition is permanent . The patient must also have documented evidence of inability to tolerate enteral feeding ( malabsorption ,obstruction ). A 66 year old women presented with abdominal pain ,nausea ,and vomiting .She had problems with poor appetite ,early satiety and frequent nausea and vomiting following meals over the past month. During that time she lost 8.5 kg .Her history included Crohn's disease for 12 years ago and again 6 months ago resulting in an ileostomy .She has noninsulin-dependent diabetes mellitus that was diagnosed 6 years earlier .On physical exam ,she was a slightly obese ,ill appearing women who weighed 65kg and was 65 in tall. Admission lab values as following: . Na=141mEq/L. Total bilirubin=0.2mg/Dl. K=3.6mEq/L. ALT=22U/L. Cl=95mEq/L. AST=15 U/L. CO2=32mEq/L. ALP=118U/L. BUN=7mg/Dl. TG=125MG/dL . Creatinine=1.2mg/Dl. Cholesterol=112 mg/dL . Mg=1.6mEq/L. Osmolarity=300mOsm/kg. Glucose=189mg/dl. Trsnsferrin= 105mg/dL. Ca=7.4 mg/dl. Prealbumin=5mg/dL. Phosphorus=1.8mg/dL. Abdominal scan findings demonstrates a partial /complete bowel obstruction with pockets of fluid collections consistent with an intraabdomianl abscess. At surgery the patient was found to have a complete Crohn’s disease ,and a large suprapubic abscess. What are the starting criteria for TPN in this patients? Can we start the patient on a TPN ? Lipid emulsion provides a major source of calories in PPN formulations ? -http://www.wenourish.com/docs/PE 5.04_Home_Monitoring_forTPN.pdf - Guidelines on The Management of Enteral Tube Feeding in Adults, Clinical Resource . -Efficiency Support Team (2004) http://www.inmo.ie/Article/PrintArticle/4377. http://www.rxkinetics.com/tpntutorial/3_1.html.