AAA Parenteral Nutrition
advertisement

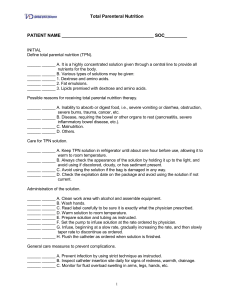
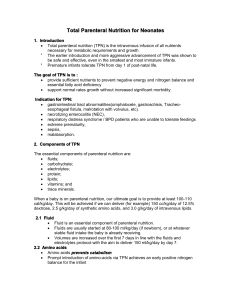
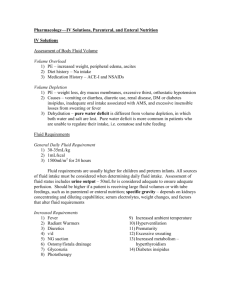
Adult Health Nursing II Block 7.0 Parenteral Nutrition Adult Health II Block 7.0 Block 7.0 Module 1.4 Learning Objectives Differentiate between Total Parenteral Nutrition and Partial Parenteral Nutrition Discuss Nursing Considerations for Clients with Complications in Parenteral Nutrition Discuss Age-Related Considerations Prioritize Nursing Care of Clients receiving Parenteral Nutrition Block 7.0 Module 1.4 Partial/Peripheral Parenteral Nutrition (PPN) Used when client unable to take nutrition through GI tract Need complete nutrition source, but are not totally depleted Usually used when client needs support less than 14 days Used when a central line is not indicated Delivered through a peripheral vein Concentrations of 5%-10% dextrose and 2%-5% amino acids Lipids may be added as well Block 7.0 Module 1.4 PPN PPN is mildly hypertonic (10%-20% dextrose) Usually administered through a large peripheral vein or can use central line Mid-line catheters are frequently used PPN is most commonly used for short term therapy Block 7.0 Module 1.4 Total Parenteral Nutrition TPN or Hyperalimentation Goal: Prevent or Correct Nutritional Deficiencies to Minimize the Adverse Effects of Malnourishment Used when client requires complete support Beneficial for long term use Allows bowel rest and healing Used for clients with large caloric and nutrient needs Delivered through a central line/PICC line Contains hypertonic glucose solutions-(20%-70% dextrose) Block 7.0 Module 1.4 TPN Different from standard IV solutions in that it contains all nutrients including: Carbohydrates- Calories Protein-Amino Acids- Tissue growth and repair Essential Fatty Acids/20% Lipid Emulsions- Heat and Energy, provides twice as many calories as proteins and carbs. Vitamins- growth and maintenance Minerals Electrolytes- K+, NA+ CA, Mg, phosphorus Trace Elements Calories- High glucose concentration Block 7.0 Module 1.4 TPN Basic Guideline for Initiating TPN 5-Day Rule: Has not eaten for 5 days and not expected to eat within the next 5 days or inadequate nutrition for 7-10 days Weight loss of 7% body weight and NPO for 5-7 days Hypermetabolic state Block 7.0 Module 1.4 Common Conditions Requiring TPN Chronic Pancreatitis Diffuse Peritonitis Bowel Syndromes Gastric Paresis Alcoholism Severe Burns Anorexia Cancer Trauma Block 7.0 Module 1.4 Complications Metabolic Mechanical Infection Fluid Imbalance Most common complication of parenteral nutrition is hyperglycemia Block 7.0 Module 1.4 Metabolic Complications Hyperglycemia Hypoglycemia Vitamin Deficiencies Electrolyte Imbalance particular NA+, K+, CA+ Nursing Considerations Monitor Daily Labs Monitor GlucoseAccuchecks Block 7.0 Module 1.4 Mechanical Complications Phlebitis Air Embolism Infiltration PneumothoraxUpon Subclavian Catheter placement Assess Site for redness, swelling warmth or cold Discourage client from talking/laughing when changing tubing Chest X-Ray Block 7.0 Module 1.4 Complications-Infection High Glucose concentration makes good medium for bacteria Contamination of the catheter on insertion Long Term Catheter Use Nursing Considerations Assess sites for redness, swelling, tenderness, drainage, warmth Assess for fever, WBCs STERILE dressing change every 72 hours or per agency protocol DO NOT use TPN line for other IV fluids and medications. May have to remove catheter, save the tip and send to lab Block 7.0 Module 1.4 Complications-Fluid Overload Hyperosmotic Solution-3 to 6 times the osmolarity of blood so at risk for fluid shifts Nursing Considerations Daily Weights Monitor Intake and Output Assess breath sounds MUST use a controlled infusion pump Usual rate is 100cc/hr or less NEVER speed up infusion to “catch up” Block 7.0 Module 1.4 A Word on Medications Many references support a “NO medication added” to TPN however medications, usually only insulin (reduce the potential for hyperglycemia) and heparin (prevent fibrin buildup on the catheter tip) may be added BY THE PHARMACIST during preparing of the TPN solution Block 7.0 Module 1.4 Care of the Elderly More vulnerable to fluid and electrolyte imbalances More vulnerable to CHF- Check history Increase incidence of glucose intolerance Age-related physiological changes influence the reliability of measures used for nutritional assessment Block 7.0 Module 1.4 Nursing Care-Pre Infusion Assess weight, BMI, nutritional status, diagnosis Assess labs-CBC, Chemistry Profiles, PT/PTT,iron, lipid profile, liver function tests, Electrolytes, BUN/Creatinine and Blood Sugar Line insertion is STRICT aseptic technique Block 7.0 Module 1.4 Nursing Care-Pre Infusion Check PCP orders MUST complete 2 nurse check prior to administration-Verify elements contained in the mixture is accurate to the prescription MUST use infusion pump Check bag for any leaks “Cracking”- Calcium or Phosphorous content of mixture is too high and presents with an oily appearance or a layer of fat on top of the mixture. DO NOT USE!!!! Block 7.0 Module 1.4 Nursing Care Pre Infusion Must be refrigerated until ready to use then at room temperature prior to hanging Careful in administering lipids either within the bag or piggyback to clients with hyperlipidemia or severe hepatic disease- usually contraindicated Block 7.0 Module 1.4 Nursing Care-During Infusion Check rate not to exceed 100mls/hr Never “catch up” Continue to assess lab values, glucose/accuchecks, daily weights, intake and output Continue to assess access site Continue to assess “YOUR CLIENT” Block 7.0 Module 1.4 Nursing Care- During Infusion If you run out of solution and new bag is not available you can hang a bag of D10% or D20% dextrose solution IV tubing is changed every 24hours or with every new bag (check protocol) TPN bag discarded after 24 hours Dressing changes are STRICT ASEPTIC technique every 72 hours (check agency protocol) Block 7.0 Module 1.4 Nursing Care Post Infusion & When to Discontinue NEVER discontinue TPN abruptly…WHY? Should be decreasing infusion rates Discontinue TPN: When client is able to eat (60% of caloric requirements) Weight gain is achieved (1 kg/day) Albumin levels reach 3.5-5.0 g/dl Serious complication Block 7.0 Module 1.4