Short Bowel Syndrome
advertisement

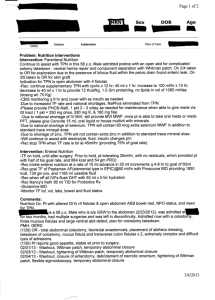
Short Bowel Syndrome Ricardo A. Caicedo, M.D. Pediatric Gastroenterology Definitions Short bowel syndrome (SBS) Functional impairment resulting from critical reduction in intestinal length Includes malnutrition, chronic diarrhea, malabsorption, growth failure The most common cause of… Intestinal failure Severely compromised intestinal function of any etiology (irrespective of bowel length) Total parenteral nutrition (TPN)-dependent Etiology: Neonates Congenital NEC - Gastroschisis - Omphalocele - SB atresias - Volvulus -Malrotation -Other - Thrombosis - Aganglionosis About 20 % of infants with NEC requiring resection develop SBS Etiology: Children/Adolescents Volvulus Trauma Intra-abdominal cancer Vascular anomalies Radiation enteropathy Overall Incidence 1:500,000 Prognostic Factors SB length Absorptive function of residual SB Proportion of daily calories tolerated enterally Intestinal adaptation Normal FT infant: 200-250 cm Loss of >70% (residual SB length < 70 cm in infants) portends SBS Compensatory events stimulated by massive bowel resection Anatomy of resection Loss of segment-specific functions Loss of ileocecal valve Anatomic Considerations Loss of segment-specific functions Jejunum: primary site of digestion and absorption Ileum: B12 and bile acid absorption Colon: water absorption and adjunctive carbohydrate absorption Ileo-cecal valve Regulation of intestinal transit Prevention of bacterial reflux into SB Management: Postoperative Period Maintenance of fluid/electrolyte balance Maintenance TPN Separate IVF for ostomy output replacement H2-blocker to tx gastric hypersecretion Await resolution of postoperative ileus Enteral Feeding Initiated when postop. Ileus resolved, UGI tract decompressed, and F/E/N status stable Advancement of EN and reduction/elimination of PN is the goal Promotes intestinal adaptation Follow hydration status, stool output, body growth, labs (albumin, prealbumin, Hb, BUN) Continuous tube feeds: decrease SB osmotic load and absorptive workload per unit of time Enteral Feeding Composition Protein Breast milk: promotes adaptation Hydrolysate (semi-elemental): peptides more easily assimilated in short gut Amino acid (elemental): prevention of milk protein hypersensitivity Fats MCT do not required bile acids/micelle formation for absorption Higher osmolarity Excess of MCT can lead to EFA deficiency Carbohydrate CHO malabsorption is the rate-limiting factor in advancing EN Glucose polymers digested more efficiently than lactose Start with dilute formula increasing in volume before increasing energy density OR Increasing in concentration before increasing rate Monitor stool output, pH, reducing substances Advancement of EN Supplements Vitamins ADEK, B12 Electrolytes: Na/K citrate, Ca, Mg Elements: Fe, Zn Cycle/window and wean TPN Increase EN at avg. rate of 0.5-1.0 cal/kg q 1-3 days Non-nutritive sucking and PO feeding to prevent oral feeding aversion Intolerance of EN but stable: home TPN Predicting Ability to Wean TPN Length of residual SB Percent daily enteral intake Earlier restoration of intestinal continuity Fewer complications Biomarkers: experimental stage Urine 3-0-methylglucose after PO feeding (rat model) Plasma citrulline levels (adult SBS pts) < 20 umol/L predict permanent intestinal failure Complications TPN-related CVL-related Cholestasis/hepatopathy Calcium-bilirubinate gallstone disease Infection- bacterial or fungal sepsis Thrombus/thromboembolism SB bacterial overgrowth Nutrient deficiencies Enterocolitis Mechanical or pseudo-obstruction (dysmotility) Pancreatitis Nephrolithiasis (oxalate stones) Prevention of TPN Liver Disease Reduce TPN/advance EN Cycle TPN (run < 18 hrs/d) Monitor TPN composition Glucose infusion rate < 8-12 mg/kg/min Keep AA at 2.5 g/kg/d Keep lipids at < 40% of total caloric intake Reduce trace elements (Mn, Cu) to 25% RDA once cholestasis develops Manage CVL infection and SBBO Start UDCA at 15-30 mg/kg/d SB Bacterial Overgrowth Factors Symptoms Feeding intolerance, abd. distention, weight loss, blood in stools D-lactic acidemia: lethargy, ataxia, WAGMA Diagnosis Dysmotility/poor peristalsis leading to stasis of enteral contents Loss of ICV Duodenal fluid aspirate and culture (> 105 col/ml) Breath hydrogen test Often made on clinical grounds Treatment Empiric antibiotics (metronidazole, TMP-SMX, PO gentamicin, amoxclavulonate, rifaximin) Adjunctive probiotics: little evidence, and a safety concern in SBS pts esp. those with CVL Medical Therapies Anti-motility agents Loperamide, diphenoxylate/atropine Slow transit time Bile acid binder (cholestyramine) Improve fluid absorption and reduce fecal fluid loss Prevents bile acid malabsorption and bile acid-induced secretory diarrhea Octreotide: reduces output from proximal enterostomies Glutamine/GH Mostly theoretical/animal or transient benefit GLP-2: may stimulate mucosal growth and reduce secretions; still experimental Surgical Interventions Longitudinal tapering Bianchi lengthening operation Doubles length, reduces diameter by 0.5 preserves effective surface area Serial Transverse Enteroplasty (STEP) Creates a maze-like tunnel within dilated segment Kim HB et al, J. Pediatr Surg. 2003; 38:881-5. SB Transplantation Indications (Am. Soc. Transplantation, 2001) Progressive/irreversible TPN liver disease (~ 4% of infants w/SBS) Cholestasis beyond 3-4 mos of age Features of PORTAL HTN Impaired synthetic function (albumin, INR) Recurrent sepsis Threatened loss of central venous access Contraindications Absolute: AIDS, overwhelming sepsis Relative: weight < 5 kg, multiple previous abdominal operations Survival Overall: 80-94% Mortality higher in patients with NEC Very long term (up to 25 y) TPN: 94% survival Transplantation Mortality is center-specific Largest experience: U. Pittsburgh (Reyes J, Semin Pediatr Surg 2001) 1-yr survival rate: 70% 3-yr, all ages combined: 55% Mortality greater in Patients under 2 y of age Combined SB-liver tx Higher risk of PTLD in SB transplantation