Speaker notes - Minnesota Health Literacy Partnership
advertisement

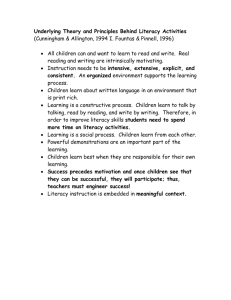
Slide 1 A program created by the Minnesota Health Literacy Partnership Health Literacy 101: Focusing on clear health communication Alisha Ellwood, MA, LMFT Chair, Minnesota Health Literacy Partnership September 2, 2009 MHLP monthly meeting Health Literacy has been gaining more National attention since the release of 2 key documents in 2004: • A report from The Institute of Medicine - “Health Literacy: A Prescription to End Confusion” • And one from the Agency for Healthcare Research and Quality – “The Evidence Based Report on Health Literacy” There are conferences held across the country from California to Washington, DC. Quality Improvement, Patient Safety, Accreditation, and Medical agencies are all beginning to discuss health literacy (such as The Joint Commission, The American Medical Association, Minnesota Department of Health and many many more) Today, a simple google search shows over half a million results Let me start by sharing a story, from the Institute of Medicine (IOM) report, to highlight the issues of health literacy… A two-year-old is diagnosed with an inner ear infection and prescribed an antibiotic. Her mother understands that her daughter should take the prescribed medication twice a day. After carefully studying the label on the bottle and deciding that it doesn’t tell how to take the medicine, she fills a teaspoon and pours the antibiotic into her daughter’s painful ear. (Institute of Medicine, “Health Literacy: A Prescription to End Confusion”, 2004, pg.3) Slide 2 Objectives • Define key concepts of health literacy • Understand implications of low health literacy on patient understanding, health outcomes, and medical costs • Apply strategies and techniques to increase clear communication and patient understanding After today’s session I hope you all will be able to : Define key concepts of health literacy Understand the implications of low health literacy on patient understanding, health outcomes, and medical costs, and Be able to apply strategies and techniques to increase clear communication and patient understanding. Slide 3 What is literacy? Using printed and written information to function in society, achieve one’s goals, and develop one’s knowledge and potential - Kirsch et al, 1993 You may be more familiar with general literacy, which is often reflected in the simple question “Can you read?” General literacy is our ability to function in today’s society and yes, does go beyond simple reading ability. Literacy represents a constellation of skills, including: reading, writing, basic mathematical calculations, listening, speaking and cultural and conceptual knowledge. Health Literacy then, challenges these general literacy skills, by placing them in the complex context of the health care system. So, while they are both connected – they are different. Slide 4 What is health literacy? Health Literacy: “The degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.” - Ratzan and Parker, 2000 / Healthy People 2010 Health Literacy is defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” It is our ability to find, understand, and act on health information. The health care industry is very complex. You can be very highly educated and read at a high grade level and still have difficulty understanding health information. Think about these examples and how you would know what to do about them: • a middle aged lawyer with diabetes trying to figure out her medication schedule during a business trip • a man wondering if he can have coffee before a lab test that requires fasting • a busy single mom searching the local drug store for the right medicine to reduce her 5-year-old child’s fever Here’s another way to look at this, think about the last time you had to do your taxes, plan for retirement, buy a house? These are difficult tasks and we rely on experts to interpret the details for us. Health information is like that for many people. Our patients look to us (medical professionals) to “translate” for them. *definition taken from U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2010. Slide 5 Expanding the definition A patient's ability to obtain, understand and act on health information A provider’s capacity to communicate clearly, educate about health and empower their patients However, there is general talk in the field that the previous definition doesn’t go far enough. In fact, some will argue that it focuses too much on “the patient’s ability”. At the Minnesota Health Literacy Partnership, we too have wrestled with the definition and in our current focus on promoting clear communication we have expanded our definition to include both the patient’s ability to obtain, understand and act on health information and the provider’s capacity to communicate clearly, educate about health and empower their patients. You will see throughout the presentation today that issues with health literacy are less reflective of the function of individual patients, but more a reflection of the system that serves us all. Slide 6 Health literacy impacts Access Safety Quality Outcomes Low health literacy impacts all aspects of care. Access: Health care information is often difficult to find. Where to look? If you think about websites…how do you know which one to use? (general literacy, computer skills, comprehension) Health care services and institutions are also complex and confusing. Where do you go to find the care that you need? There are so many options today (nurse line, urgent care, e-vitis, e-mail your doctor or clinic, call your doctor, go to a retail clinic – like minute clinic, emergency department, regular primary care visit, specialty visit….etc.) How do you know when to seek out or why you need preventive care? What about navigation? Where do I go once I get there? (maps, numeracy, bus schedules). Safety: Patients with low health literacy may not be able to clearly report about their condition and/or medication, this can be dangerous if treatment is based on inaccurate self-reports. Informed consents are often written less for the patient and more for legal issues, in Minnesota, the MN Alliance for Patient Safety has created a more understandable informed consent form and process to help increase the safety for patients…ensuring that they truly do understand what they are consenting to. Patients may be nervous when talking with professionals and not speak up. Quality: Patient satisfaction is an important measure these days, and patients who have trouble understanding their doctor’s instructions often report lower satisfaction with their clinic. Health professionals also need to pay attention to cultural and linguistic needs of each patient. Outcomes: Low health literacy impacts understanding of medication labels and treatment regimens, overall treatment adherence problems arise when patients don’t understand the importance of maintaining a treatment course or follow-up appointments. As you can see, being health literate involves many skills: reading, writing, arithmetic, comprehension and complex reasoning, map reading/navigation, advocating for oneself and more… Slide 7 What is it like? I want to give you the opportunity to experience or remember what it feels like to struggle with reading information. I want you to read the following paragraph out loud, together, and I’ll give you a minute to do this. A hint is that the words are written backwards. Activity 1 What is it like? 5 minutes (slides 7-9) Slide 8 One minute to read this . . . GNINAELC – Ot erussa hgih ecnamrofrep, yllacidoirep naelc eht epat sdaeh dna natspac revenehw uoy eciton na noitalumucca fo tsud dna nworb-der edixo selcitrap. Esu a nottoc baws denetsiom htiw lyporposi lohocla. Eb erus on lohocla sehcuot eht rebbur strap, sa ti sdnet ot yrd dna yllautneve kcarc eht rebbur. Esu a pmad tholc ro egnops ot naelc eht tenibac. A dlim paos, ekil gnihsawhsid tnegreted, lliw pleh evomer esaerg ro lio. Ok, begin. CLEANING - to assure high performance periodically clean the tape heads and capstan whenever you notice an accumulation of dust and brown-red oxide particles. Use a cotton swab moistened with isopropyl alcohol. Be sure no alcohol touches the rubber parts, as it tends to dry and eventually crack the rubber. Use a damp cloth or sponge to clean the cabinet. A mild soap, like dishwashing detergent, will help remove grease or oil. Keep track of the time and advise them when 15 seconds are left – adds a sense of urgency and discomfort. You might find that participants stop and start…sometimes encouragement can help…”keep going…don’t give up”. You can always stop earlier than one minute if you feel that is best. The main point is to get them to talk about what gets in the way when you struggle with reading information. Slide 9 What was it like? How did you feel? Do you know what to do? Discuss participant’s reaction to doing this exercise. Some questions to help guide discussion are listed below. • Did anyone finish? (Most won’t finish.) • How did you feel during the exercise? (You will get responses like…”I felt dumb…frustrated…I gave up”.) • Do you know what you were reading about? (“No”. “Yes, cleaning a tape head”) • What got in the way…or what was difficult? (Most people will recognize that they had to spend so much time determining what each individual word was that they lost the context of the article. They couldn’t remember what they had just read because each word was too difficult.) • Does anyone know what to do next? What does the article tell you to do? (It says to clean the tape heads or capstan using a cotton swab with isopropyl alcohol.) • What if this was about your health care…would you know what to do? (Bring the focus back to health care and the difficulty that comes with reading unfamiliar terminology, etc.) Slide 10 Only 12% of adults are proficient percentage of population at each level Health Literacy results from the National Assessment of Adult Literacy, US Dept of Education, 2003 Now that you’ve had the experience of struggling with a piece of written information. Let’s look at how many people also have this type of difficulty when trying to understand health information. The Department of Education conducted surveys in 1993 and 2003 regarding literacy levels in the U.S. The 2003 survey is called the National Assessment of Adult Literacy and had 19,000 participants. The results were disappointing in that they showed that over the 10 years since the 1993 measurement, the literacy levels in the U.S. had basically remained the same. The 2003 survey added questions that were specific to determining health literacy levels. The results show that only 12% of adults are proficient in understanding health information. Or in other words more than 1/3 of adult English speaking Americans are at basic or below basic health literacy skills – if we put that in MN terms it equals about 1.86 million people 1) Only 1/3 of patients with limited health literacy skills were able to answer correctly what it means to “take 2 tablets twice daily” – Wolf, annals of internal med 2006 1) 42% couldn’t understand “take on an empty stomach” and 60% did not understand informed consent – Williams et al, JAMA 12/95 Examples of tasks at each level: (from National Assessment of Adult Literacy, US Dept of Education, 2003) Below Basic: circle date on doctor’s appointment slip Basic: give 2 reasons a person with no symptoms should get tested for cancer based on a clearly written pamphlet Intermediate: determine what time to take prescription medicine based on label Proficient: calculate employee share of health insurance costs using table *only a 67% probability individual can perform task at that level Slide 11 Why are patients at risk? Reliance on the written word for patient instruction Increasingly complex healthcare system • More medications • More tests and procedures • Growing self-care requirements • Esoteric language Why are patients at risk? We rely heavily on the written word for health communication. Patients are handed information as they leave a doctor’s office, insurance information is mailed out, and waiting rooms are often filled with brochures. Health information is often communicated at a very high level – 12th grade or higher – when the average American reads at an 8th grade level. This creates a large gap in the ability to understand important health messages. And the health care system isn’t getting any easier. There are more medications, tests, and procedures. Patients are given more options and expected to be able to choose the best one for them. Patients are expected to do more on there own, to be able to take care of things at home – self-care requirements. In terms of patient education, 35 yrs ago a new diabetic patient would have been hospitalized for 3weeks and received 2 hours of patient education a day. So by the time they were discharged, they would have received about 15 classes or 30 hours of instruction before leaving the hospital. Now new diabetics are treated as outpatients with limited instruction before returning home. When I think of self-care, I often think of when I’ve tried to go out and look up a symptom or disease on the internet. The internet is a challenging place where several literacy skills are needed to correctly navigate yourself to a reputable page that contains the information you are looking for. We, as consumers, are often directed...”to look at our website”. It may not surprise you to hear though, that even with all of these great resources at our fingertips, for those we most want to reach…those at the lowest levels of literacy, 80% NEVER use the internet to get health information. – NAAL, U.S. Dept of Education We often use an esoteric language in health care. Does anyone know what this means? Esoteric actually means mysterious - confined to and understandable by only an enlightened inner circle, intended for understanding by only a particular group, not publicly disclosed. This is not the kind of message that health care is trying to get across. Slide 12 Who is most at risk? • Elderly • Ethnic and racial minorities • Limited education Immigrants • Low socioeconomic status • People with chronic disease Health Literacy is critical when we consider who is most at risk and our changing demographics in Minnesota. We have an aging population. According to the MN state Demographic Center, by the year 2035, the number of Minnesotans greater than equal to age 65 will increase by 125%. Elderly represent a population that is surviving longer with more complex and long-term medical needs. We are also becoming more and more diverse. Minnesota does not have the same cultural make-up it did even 10 years ago. Minnesota had more immigrants arrive in 2005 than in the last 25 years. Two in five of these immigrants were from African nations. We have the largest urban Hmong and Somali populations in the United States. Slide 13 Health literacy by age - 2003 National Assessment of Adult Literacy (NAAL), US Dept of Education Seniors are one of the most at risk populations for not understanding health information. These results show that 29% of those over age 65 fall into below basic health literacy levels and that another 30% are at basic. How many of you have helped a parent or grandparent with medications? Why do you think seniors are at risk? • Physical limitations – poor eyesight and/or hearing, memory problems • Passive learning style – learn more from TV, watching…whatever comes by them, rather than pursuing knowledge through reading • Living longer with complicated illnesses & increased self-care requirements • Perhaps they grew up in a time where questioning the doctor was not considered ok A recent study from the Journal of General Medicine studying 17,000 community-dwelling Medicare beneficiaries age 65 and over, living in low-income neighborhoods, across all 50 states • Found that 40% of respondents reported some kind of non-adherence to medication regimen • And of those reporting 3 or more chronic conditions, more than half were not taking medicines as directed. Ref: Physician-Patient Communication about Prescription Medication Non-adherence: a 50-State Study of America’s Seniors, Journal of Gen Med, 2007 Therefore, those with the greatest need to read and understand health care information (those taking multiple medications for multiple conditions) have the poorest skills and the greatest burden of low health literacy Slide 14 …by race/ethnicity - 2003 National Assessment of Adult Literacy (NAAL), US Dept of Education The Hispanic population is one of the fastest growing populations in the U.S. Minnesota is no different. We have several Hispanic, Latino and Mexican communities within our state. The state demographic center projects that by the year 2030, there will be three times the number of Latinos as were here in 2000. This is also important to us as we see that 41% of Hispanics who were surveyed fell at the below basic health literacy level. More references/states for the national/state demographic information: Minnesota’s Latino population has grown rapidly in recent years, and this is expected to continue. The number of Latinos is projected to grow 98 percent between 2000 and 2015. By 2030 there will be 406,700 Latinos, up from 143,382 in 2000. Growth can be attributed to a combination of international migration, migration from other states, and a high rate of natural increase. http://www.demography.state.mn.us/DownloadFiles/PopulationProjectionsRaceHispanicOrigin.pdf http://www.demography.state.mn.us/resource.html?Id=10959 The Hispanic origin population is projected to increase rapidly over the 1995 to 2025 projection period, accounting for 44 percent of the growth in the Nation's population (32 million Hispanics out of a total of 72 million persons added to the Nation's population). The Hispanic origin population is the second fastestgrowing population, after Asians, in every region over the 30 year period. http://www.census.gov/population/www/projections/ppl47.html Slide 9 Patients with low literacy nearly twice as likely to be hospitalized 35% How likely to be hospitalized 30% 25% 20% 15% 10% 5% 0% Literate Marginal Low Literate Baker, Parker, Williams, et al. JGIM 1999 Patients with low health literacy are twice as likely to be hospitalized – and when they get to the hospital they often need to stay longer. Why does this happen? • Patients don’t understand treatment regimens &/or the importance of following them, • they make medication errors • Patients with asthma are less likely to know how to use an inhaler • Patients with diabetes are less likely to know symptoms of hypoglycemia • Patients with hypertension are less likely to know that weight loss and exercise lower blood pressure • Patients present at later stages of illness • waiting until symptoms are advanced - until the problem is severe before seeking help • And, they use the emergency department more often Here’s another example from the Institute of Medicine (IOM) report: A 45-year-old Hispanic immigrant, Mr. G., undergoes a job health screening and is told that his blood pressure is very high and he will not be allowed to continue work until his blood pressure is controlled. He goes to the local public hospital and is given a prescription for a Beta-blocker and a diuretic. The doctor prescribes two medications known to be effective and simple for adherence because they each are supposed to be taken once a day. Mr. G. presents to the emergency department one week later with dizziness. His blood pressure is very low, and Mr. G. says he has been taking the medicine just like it says to take it on the bottle. The puzzling case is discussed by multiple practitioners until one that speaks Spanish asks Mr. G. how many pills he took each day. “22,” Mr. G. replies. The provider explains to his colleagues that “once” means “11” in Spanish. Patients may also have trouble understanding discharge instructions. Things that they need to do to stay out of the hospital in the future. A Mayo Clinic study done in 2005 showed the following understanding for patients at discharge: • 27.9% could name medications • 37.2% knew purpose of medications • 14% knew side effects • 41.9% knew their diagnosis Slide 10 Burden to system Low health literacy increases US health care costs by $50 billion – $73 billion annually.* *Estimated by National Academy on an Aging Society using 1998 figures Low Health Literacy increases US health care costs by an estimated $50 billion -$73 billion per year. Some recent reports estimate this to be even higher. A report released in October 2007 from the University of Connecticut states that the impact of low health literacy is anywhere from $106 billion – $236 billion annually. It may even be higher today. I believe that some of the reasons why low health literacy is so costly are already apparent to you. • The primary source of these higher costs is due to longer hospital stays. • Other factors include medication errors, excess hospitalizations, more use of the emergency department and higher level of illness. Who pays for all this? We all do. Cost References: • Friedland, RB. Understanding Health Literacy: New Estimates of the Cost of Inadequate Health Literacy. Washington, D.C.: National Academy of Aging Society, 1998. • University of Connecticut “New Report Estimates Cost of Low Health Literacy Between $106$236 Billion Annually”, October 12, 2007 Share this example from the Institute of Medicine report, “Health Literacy: a Prescription to End Confusion” if there is time. Here is an example highlighting unnecessary costs related to care: “Jose, a Bolivian man in his early 30s, stayed after class one night so I could help him understand a hospital bill. He had been having bad headaches for some time. Thinking it was his only option for care, he had gone to the emergency department to get treatment. There he was told the headaches would clear up if he got glasses. He was charged $300 for this diagnosis (Singleton, 2002).” Slide 117 Understanding the problem Health literacy and patient safety: Help patients understand The video we are about to see is a core component of many health literacy trainings. It was created by the AMA (American Medical Association) in 2007. It gives us a deeper understanding from the perspective of real patients and the doctors that try to help them. While you are watching, consider the barriers to care and what techniques you can use in your practice. Activity 2 Understanding the problem 30-40 minutes (slides 17-18) Slide 128 Discussion Discussion: What reactions do you have to the video? (expect comments like: the pharmacist tech is frightening, awe over the woman who had a hysterectomy, the amount of medicines, how you can’t tell by looking at them that they don’t understand) What are some of the key points that you will take away? What was the first thing that the receptionist did when she saw someone coming? (SMILE – answer the phone with a smile – I read in a magazine recently that if you smile when you pick up the phone, the person on the other end will ‘hear’ it.) Reference examples that you like: I especially like the man who has hypertension…. He understands what hyper means, yet he is the least hyper person I’ve ever seen. Can you imagine being him and believing that you doctor thinks you are hyper….that is a huge disconnect in understanding. Another thing I like about this example is that the provider takes responsibility for him not understanding, stating “I haven’t done a very good job teaching you about hypertension”. She owns it – this is very important to remember when we are trying to communicate clearly with respect and maintaining that shame-free experience. Transition…. So, what do we know…. Slide 19 What do we know? • Universal problem • Predictor of health status • Limited health literacy leads to: • Greater health costs • Poorer health outcomes We know that low health literacy is a universal problem – that anyone can have trouble understanding health information and that everyone struggles when hearing a new diagnosis. We know that health literacy is one of the best predictors of health status, regardless of race, socioeconomic level, etc. That lower health knowledge leads to less healthy behaviors, increasing costs, and leading to poorer health outcomes. Transition: And we know that there are things that we can do to increase our ability to clearly communicate health information. Slide 20 Strategy: Recognize red flags • • • • • Making excuses Perceived resistance Has no questions Frequently missed appointments, tests Non-adherent with meds or treatment It is not practical to give every patient a “health literacy test”. And yet, as we’ve seen in the video, knowing who has low health literacy might be difficult. The Minnesota Health Literacy Partnership advocates focusing on clear communication with all patients. There are some things that you can look for to help you recognize when patients are having a difficult time such as… Red Flags: • Making excuses: “I forgot my glasses, I’ll read it when I get home” “Let me bring it home to discuss it with my children/spouse”; using humor or clowning around • Perceived resistance: someone getting frustrated, not wanting to listen or follow instructions • Someone who has no questions – this may not mean that they understand everything… • Missed appointments, for example to specialists, or not refilling scripts when expected You may also want to watch for • Incomplete forms • If patient waits to seek help until they are so sick that they need to go to the ER or hospital rather than the doctor’s office • If they are unable to name medications or how to take them (the brown bag test) Slide 21 Strategy: Create a shame-free experience Convey an attitude of helpfulness, caring and respect—by all staff – Ask questions to help patients open up – Listen – Encourage patients to ask questions – SMILE Provide assistance confidentially Convey and attitude of helpfulness: First impressions make a big difference! • Remember to smile. Smiling helps set the stage and is welcoming to others. • Ask open ended questions to get patients to open up. What and How questions work well. You might start by asking “How can I help you today?” • Listen. It is so easy to forget this critical piece of clear communication. Giving the patient time to talk about his or her problems is very important…and doesn’t make visits any longer. • one study reports that when patients were allowed to talk without interruption for as long as they liked they spoke on average 1min 40secs Resource: Marvel, Epstein, Flowers, Beckman JAMA 1999; 281:283-287 • Another study shows that when pts were permitted to voice their initial concerns at the beginning of an office visit, again for as long as they wished without interruption, they talked on average for 92secs with a median of 52secs Resource: Langewitz et al, BMJ 2002; 325:682-683 • Encourage patients to speak up and ask questions. Assume that patients will not understand and let them know that what you are talking about is difficult. “Let me know when you have questions”…the ‘when’ gives them the impression that you are expecting them to have questions. • Take responsibility for communication breakdowns. One of the most important things to remember in creating a shame-free experience is to remember it is your job as the provider / educator to help the patient understand regardless of why they may have difficulty. “I didn’t explain that very well…let me try again”. Just like in the AMA video when the nurse is talking with the man who has hypertension she says, “I didn’t do a very good job explaining what hypertension is”. When you find that someone does need assistance. Provide help confidentially. Help them in a private area, not in the waiting room for all to see. Slide 22 Strategy: Improve interpersonal communication Slow down – take your time Use plain, non-medical language – “living room” language It is also very important to look at how we explain things…how we are talking and what words are we using. Slow down the pace of your speech. Don’t speak so quickly. Speaking more slowly gives the patient time to take in what’s been said and may help them develop important questions. Use plain, non-medical language: words that anyone could understand. Often called “living room” language, because you use words that you’d use talking to your family or friends at home. Keep away from medical jargon and terminology. If you must use medical terms, then explain them as well. Patients want to understand their medical conditions and treatment plans. Help ensure that they do by following some of these ideas: For example, use the words “pain killer” instead of “analgesic” What about these? what could you say instead? anti-inflammatory…………helps swelling go away Benign…………..not cancer Contraception…………...birth control Oral…………..by mouth Adverse…….. bad Lipids ……..fats in blood Monitor……..keep track of or watch Diet…………….what you eat Activity 3 Practice using living room language 10-15 minutes (slide 22) If there is not time you can just run through a few of the examples above. Slide 23 Strategy: Improve interpersonal communication Use analogies and pictures – charts – Models – diagrams Limit to most important concepts – focus on 1-3 key messages Repeat them Use analogies. Analogies can be very helpful because they can explain a concept that is unfamiliar to a patient in a more familiar way such as describing arthritis like a creaky hinge on a door. The key thing to remember when using analogies is that you need to understand the patient’s context as well. It wouldn’t make sense to use an analogy using the ocean if someone has never seen the ocean before. Use pictures. People learn in all different kinds of ways, auditory and visually. Using pictures can help people see parts of their body they would normally not be able to see. Limit to most important concepts. Another cause of communication breakdowns can be information overload. How many times have you picked something up, thinking you’d read it, and then discovered it was multiple pages and just too long….and eventually found it’s way into the trash can rather than being read? It can be difficult to limit health education. Health professionals often want to give the patient everything they can in the short amount of time they have. People can only remember one, two or three pieces of any conversation. You can start by asking what the patient already knows about their condition, this can help you skip over familiar information and focus on what else they need to know. Transition: Another way to help you stay to only the most important concepts is to consider using the Ask Me 3 questions. Slide 24 Strategy: Empower patients Ask Me 3 What Is My Main Problem? What Do I Need to Do? Diagnosis Treatment Why Is It Important for Me to Do This? Context Ask Me 3 was developed by the Partnership for Clear Health Communication (funded by Pfizer). It was written to help encourage patients to be active in their visits and empower them to be sure they know the answers to the three questions at the end of every visit/conversations/ etc. with a health care professional. Making sure that you, as a health care professional, provide the answer to these simple questions will help you give what the patient needs to know most regarding their diagnosis, treatment and context. The 3 questions are: What is my main problem? Explain in “living room” language what their diagnosis is. What do I need to do? Tell them what they need to do…what is their treatment. Why is it important for me to do this? Provides context and motivation for them to continue treatment The Partnership for Clear Health communication is a national, nonprofit coalition of organizations that are working together to promote awareness and solutions around the issue of low health literacy and its effect on health outcomes. Provide the reference if there is time. You can visit their website to learn more about this program. http://www.npsf.org/askme3/ You can also type in Ask Me 3 in google to find it. Slide 25 Strategy: Use teach-back method Ask patients to demonstrate understanding – “What will you tell your spouse about your condition?” – “I want to be sure I explained everything clearly, so can you please explain it back to me so I can be sure I did.” – “Show me what you would do.” Chunk and check Summarize and check for understanding throughout, don’t wait until the end. Do NOT ask . . . – “Do you understand?” Use the teach-back method. Ask the patient to demonstrate understanding. • The teach back allows you to check for understanding and, if necessary, re-teach the information. • This technique creates the opportunity for dialogue in which the physician provides information, then encourages the patient to respond and confirm understanding before adding any new information. • We must ask the patient to explain or demonstrate understanding in a way that is not demeaning. • It is important not to appear rushed, annoyed, or bored during these efforts – your affect must agree with your words. • You can also think of this as the “show-back” technique. Sometimes it is most appropriate to as for a physical demonstration of what the patient will need to do…to show you back how to do it. Research shows that practice by doing increases understanding and retention by 75% (Resource: National Training Laboratories, Bethel, Maine) Research also indicates that “teach backs” work. “Asking that patients recall and restate what they have been told” is one of 11 top patient safety practices based on strength of scientific evidence. - (Resource: AHRQ, 2001 Report on Making Health Care Safer) When using the teach-back, remember to not overload the patient with too much information before asking for understanding….don’t wait until the end of the visit…ask throughout the encounter, chunking information into sections and check in along the way. And, do not ask, “Do you understand?”. As the doctor from the video points out, “they may understand, but it may not be what you said”. Asking yes or no type questions doesn’t help you know where the patient is at. Activity 4 Practice situations 15-20 minutes (slides 23-25) Slide 13 Strategy: Use patient-friendly materials and forms Tips for easy-to-understand materials – Keep text short and simple – Limit medical jargon – Use clear headings, bullets and lots of white space – Use active voice – Focus only on 1-3 key points – Emphasize what the patient should do (actions) Think about the verbal techniques we just discussed and put them into print! If you do not create materials, but send things out that others have created.... Use these tips to help you choose appropriate information for your patient. Just like in verbal communication, it can be difficult to pare down and simplify materials when for many the natural tendency is to want to include everything. Try to keep materials short and simple. Sometimes it may be necessary to include specific terms. When possible, include a definition along with the medical term so the patient doesn’t need to look it up or guess what it means. Using headings helps the patient know what is important about this section and why they should read it. Using larger type – aim for 12 point size and always use a simple font. (for example, Times New Roman) Other things to look for: • Use of simple pictures - many translate to across languages • Sensitive to cultural preferences • Follow-up on materials at next call by asking them to give you 1-3 key points from the information sent. There are resources and tools in your packet to help you assess and write so all can understand. Using the active voice helps to keep things concise and less wordy as well. (The active voice is when the subject of the sentence acts….an example would be the dog bit the boy. A passive sentence would be the boy was bitten by the dog.) Slide 14 Next steps . . . Apply strategies learned today Do a walk-through in your area and identify barriers Review documents and forms and simplify as appropriate Develop a plan to educate all staff about health literacy What can you do right now? Begin to use the strategies and techniques we talked about today. Do a “walk through” in your area. What is it like to be your patient? Review letters and forms – can they be easier? Clearer? Develop a plan to educate others – how can you spread the message to your clinic? Perhaps you could even create a health literacy team or task force to maintain momentum and training. Note: Please feel free to tailor this to your own area or to the audience you are speaking to. Activity 5 Personal action plan 5-10 minutes (slide 27) Slide 15 Together we can make a difference Goals: Train health care providers Empower patients Share resources Mission: Working together to improve the health of all Minnesotans through clear communication http://healthlit.themlc.org The Minnesota Health Literacy Partnership was formed in 2006 as a program of the Minnesota Literacy Council. It is a collaboration of over 20 health care, public health, community and academic organizations We work to improve the health of all Minnesotans through our efforts to train health care providers, empower patients and share resources. If you would like more information about the Minnesota Health Literacy Partnership or to find health literacy resources, please visit our website at http://healthlit.themlc.org Slide 16 True or False? 1. Literate patients are insulted by low literacy materials. 2. You can tell by looking if someone has low health literacy. 3. A college degree means the patient will understand medical information. 4. Many of my patients have problems understanding health information. Now it’s time for the quiz…. True or False? 1. Literate patients are insulted by low literacy materials. False. Everyone appreciates easy to understand information about their health. We all feel “health illiterate” when hearing a new diagnosis 2. You can “tell” by looking someone has low health literacy. False. You can’t tell. Health Literacy is a universal problem. Health information is difficult for many people to understand regardless of race, education or socioeconomic background. 3. A college degree means the patient will understand medical information. False. On average people read 3 to 5 grades lower than the last year of school completed. Even some of those scoring at the highest general literacy levels still fell into basic and below basic health literacy categories. 4. Many of my patients have problems understanding health information. True. Only 12% of adult English speaking Americans are at a proficient health literacy level. Just in case you need more information: 67% of patients with low literacy had not told their spouse, over 50% had not told their children, and 19% had never told anyone. Ref: study by M.V. Williams Slide 30 Questions? Any questions? Slide 31 Resources • American Medical Association http://www.amafoundation.org • Institute of Medicine Health Literacy: A Prescription to End Confusion http://iom.edu/ • Joint Commission Resources http://www.jcrinc.com/education.asp?durki=11276&site=5&return=11114 • Agency for Healthcare Research & Quality (AHRQ) Health Literacy and Outcomes Evidence Report www.ahrq.gov • Multilingual Health Resource Exchange www.health-exchange.net My contact information: e-mail: alisha_ellwood@bluecrossmn.com & phone: 651-662-0986 Here are some additional resources where you can find more information about health literacy. You may also contact me with any further questions or comments. Please use your own contact information here or ask them to contact the Minnesota Health Literacy Partnership via our website. Slide 32 “Understanding is a two-way street.” Eleanor Roosevelt Remember that everyone plays a role in communication. Slide 33 Acknowledgements The Minnesota Health Literacy Partnership recognizes the following groups for content contributions: American Medical Association StratisHealth Blue Cross and Blue Shield of Minnesota MHLP provider training team The Minnesota Health Literacy Partnership would like to recognize the following groups for contributions to this presentation. Slide 34 A program of the Minnesota Literacy Council