Skeletal System Chapter 6
advertisement

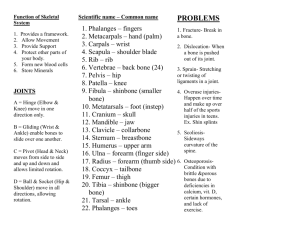
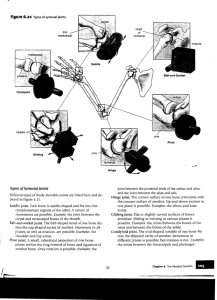
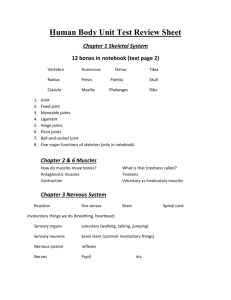
Chapter 7: Skeletal System 206 total named bones in the human body that come in various shapes and sizes o Long, Short, Irregular, Flat Formed of osseous tissue – (bone tissue) one of two hard connective tissues FUNCTIONS: 1. Support – provides a hard framework 2. Protection - skull, ribcage, vertebrae 3. Movement/Leverage – along with muscles create movement 4. Mineral storage – Mostly Ca+ and PO2+; lipids in yellow marrow 5. Hematopoiesis – blood cell formation, mostly RBCs Axial vs. Appendicular skeleton STRUCTURE OF BONE: a typical long bone Diaphysis: (shaft) longer than it is wide; shat has two distinct ends - Marrow Cavity: center shaft of diaphasis; contains yellow marrow (fat storage) Epiphysis: (proximal and distal expanded ends); contains spongy bone - Articular cartilage: Hyaline cartilage that covers and cushions bone ends - Epiphyseal plate: (epiphyseal line) remnants of bone growth COMPOSITION OF BONE: Cells: Osteocytes Mature bone cells - maintain composition Osteoblasts Bone building cells - produce matrix Osteoclasts Break down bone (monocyte) - resorption of minerals A. COMPACT BONE: - looks solid but contains few spaces where living tissue exists o Haversian system “osteons” – elongated cylinders parallel to the axis of long bone o Central (Haversian) canal – channel down the center of an osteon that contains bloodvessels and nerve fibers that serve bone cells Perforating canals run perpendicular to the axis to deliver vessels from outer to inner B. SPONGY (CANCELLOUS) BONE: - doesn't have Haversian System and has more spaces than compact bone o Trabeculae – honeycomb arrangement of bone tissue that lie along lines of stress consists of many spaces filled with marrow: - red marrow found in sternum, hip, ends of long bones Membranes: - Endosteum – interior covering that lies over spongy bone - Periosteum – entire external surface except where cartilage exists o Inner layer consists of osteoblasts (osteogenic tissue) and outer layer is fibrous connective tissue Organic Framework: - 65% of the mass is made up of mineral salts - Combination of fibers/salts makes bone hard and durable without being brittle DEVELOPMENT OF BONE: ossification or osteogenesis - Process is to convert cartilage cells into bone cells - Begins around week 5-6 during embryonic development INCREASE IN BONE LENGTH: Epiphyseal plate: site of growth Epiphyseal plate's cartilage cells reproduce to keep the thickness constant - cartilage forms tall column of cells, dividing quickly at the top to push the plate away from the diaphysis - the rate of cartilage growth on the epiphyseal side is equal to replacement of bony tissue on diaphysis side Plates become thinner and thinner as adolescence hits 18 to 21 yrs of age Growth of bones controlled by Human Growth Hormone and Thyroid hormones Bone Markings - Distinguishable markings on bone that are created for attachment, create joints, allow for passage through bone Bones of the Skeleton Broken down into two groups - Axial – 80 bones of the vertebral axis - Appendicular – 126 bones of the appendages & girdles Skull – separated into 14 facial bones and 8 cranial bones (plus hyoid and 6 ossicles) - sutures: immovable joints between o fontanels: - sinuses: air-filled chambers Vertebral Column – 30-32 bones that support the trunk and protect - 7 cervical,12 thoracic, 5 lumbar, 5 (fused) sacrum, 2-3 coccyx - Thoracic and lumbar curvature - Vertebrae structure Thoracic cage – 12 pairs of ribs, sternum - true vs false ribs - Connected to sternum by costal cartilages Pectoral Girdle and Upper limb - scapula, clavicle, humerus, ulna, radius, carpals, metacarpals, phalanges (phalanx) Gleno-humeral (shoulder joint) – ball in socket Pelvic Girdle and Lower limb - os coxae, femur, tibia, fibula, tarsals, metatarsals, phalanges (phalanx) Joints (articulations) •Point of contact between two bones •Joints structure determines how it functions •The closer the fit at the point of contact the stronger the joint. •Joints are the weakest points of the skeleton Types of joints •Synarthroses – immovable joints •Amphiarthroses – slightly immovable joints •Diarthroses – freely immovable joints - Synovial joints: o Capsule, synovial fluid, ligaments o Menisci, fat pads, bursae STABILITY OF SYNOVIAL JOINTS: 1. Shape of articular surface 2. Number and position of ligaments 3. Muscle tone ANGULAR MOVEMENTS: Increase or decrease the angle between two adjoining bones - Result of the action of muscles around the specific joint FLEXION: *DORSIFLEXION *PLANTAR FLEXION - EXTENSION: *HYPEREXTENSION - ABDUCTION: ADDUCTION: CIRCUMDUCTION: ROTATION: Special Movements: PRONATION: SUPINATION: Palms up ELEVATION: DEPRESSION: INVERSION: Sole turns EVERSION: Sole turns OPPOSITION: Thumb touches tips of other fingers Shapes of Synovial Joints: 1. gliding (plane) joints - between 2. Hinge joints 3. Pivot joints 4. Ellipsoidal Joints: one articular surface concave and the other convex. 5. Saddle: 6. Spheroid (ball & socket): FACTORS WHICH AFFECT BONE REMODELING 1. Stress: Bone grows in response to prolonged heavy load A. gravitational forces: B. functional forces: - regular exercise can alter the form of the skeleton 2. Hormones : negative feedback mechanisms A. PTH (parathormone) B. Calcitonin 3. The age of the individual: - osteopenia to osteoporosis 3 factors to decrease risk of osteoporosis: (box 7-2) 1. 2. 3. 4. Rates of Mineral absorption (Ca and P) 5. Genetic and Environmental factors: Examination of the Skeletal System involves: 1. Observation of any limitation of movement or stiffness 2. Understanding of the distribution of joint involvement and inflammation 3. Are there any sounds associated to joint movement 4. Observation of any abnormal bone deposits 5. Observation of abnormal posture Conditions of Clinical Significance for Bone Disorders: A. Congenital disorders (present at birth) - Marfan’s Syndrome - Cleft palate B. Infection - Osteomyelitis - Paget’s Disease (osteitis deformans) C. Nutritional - Ricket’s - Scurvy D. Trauma - Bone Bruise - Fractures: 1. simple: 2. compound: - Comminuted, depressed, impacted, transverse, spiral, Colles’, greenstick, epiphaseal, Pott’s, displaced vs nondispalced Healing process: 1. bleeding occurs froming a hematoma, formation of a fibrocartilaginous callus, formation of a bony callus within external callus, bone remodeling (from 3 weeks to over a year) E. Secondary disorders - Gigantism - Pituitary growth failure Conditions of Clinical Significance for Joint Disorders: A. Inflammation - Bursitis - Rheumatism and Arthritis - Rheumatic arthritis: - Prosthetic joints B. Degenerative – Osteoarthritis C. Infection – Rheumatic fever D. Metabolic – Gout E. Trauma - Dislocations and subluxations - Strains and sprains Arthroscopic Surgery – Use of optic fibers within a surgical tube to explore a joint without major surgery. – An additional scope may be used to repair damage at the same time