EUROPEAN
advertisement

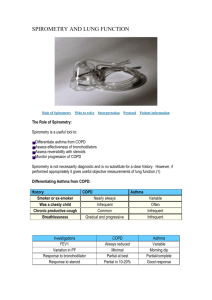
EUROPEAN RESPIRATORY JOURNAL October issue (Vol. 32, Number 4) CLINICAL GUIDELINES CAUSE SUBSTANTIAL OVERDIAGNOSIS OF COPD Following current clinical guideline definitions for airflow obstruction is leading to a substantial number of middle-aged and elderly people in primary care being misdiagnosed with chronic obstructive pulmonary disease (COPD), according to Dutch researchers. Tjard Schermer (Radboud University Nijmegen Medical Centre, Nijmegen, the Netherlands) and colleagues compared the diagnostic outcome when two recommended but different definitions for airflow obstruction based on the forced expiratory volume in one second to forced vital capacity ratio (FEV1/FVC) were applied in a large population of patients without a prior diagnosis of chronic respiratory disease referred for a diagnostic spirometry test by their general practitioner. Guidelines recommend a “one size fits all” fixed cut-off point of 0.70 for the FEV1/FVC ratio to decide on whether or not airflow obstruction is present, regardless of the age and gender of the person involved. Schermer and team used a gender- and age-specific “lower limit of normal” cut-off point for the FEV1/FVC ratio for comparison. Using data from diagnostic spirometry tests of 14,056 respiratory patients (53% female, 69% current or former smokers), the researchers calculated a sensitivity of 97.9% for the fixed cut-off relative to the lower limit of normal cut-off point for COPD, a specificity of 91.2%, a positive predictive value of 72.0% and a negative predictive value of 99.5%. The discrepancy between the recommended fixed 0.70 FEV1/FVC cut-off and the genderand age-specific lower limit of normal cut-off became more pronounced as the age of the patients analysed increased: in patients aged 50 years or older, at least 33% were misdiagnosed with airflow obstruction when the fixed cut-off point definition was used! "Although the negative predictive value of the fixed ratio definition was very high, the positive predictive value of the fixed ratio (72%) was insufficient," the authors write. "As spirometry is used as a diagnostic test to verify obstruction (instead of excluding it), these predictive values are insufficient." Schermer and team conclude: "Although diagnosing COPD obviously requires more than a spirometry test (i.e. symptoms, smoking history and additional diagnostic tests), a definition of airflow obstruction that is based on lower limits of normal from an appropriate reference population would diminish the rate of false positive interpretations". The authors add: "The individual, as well as the societal, burden of COPD is sufficiently large to warrant critical appraisal of the main criterion on which the diagnosis of the disease is based." TITLE OF THE ORIGINAL ARTICLE Current clinical guideline definitions of airflow obstruction and COPD overdiagnosis in primary care