Spirometry Quality Control and Misclassification
advertisement

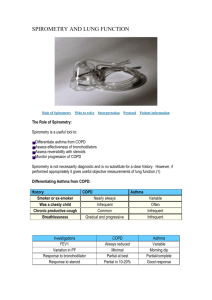
Spirometry Quality Control and Misclassification P.L. Enright*, M. Studnicka#, J. Zielinski (2005) Spirometry to detect and manage chronic obstructive pulmonary disease and asthma in the primary care setting. Eur Respir Mon 31, 1–14. http://www.carefusion.co.uk/pdf/Respiratory/HFOV/ra_ch1.pdf “Misclassification rate is around 5% in most research and sub-speciality settings. But research suggests this is higher in primary care settings. Common cause of error is inadequate spirometry training and experience of the practitioner.” _________________________________________________________________________ 1999 Trained Practitioners-only 3 acceptable blows in 18.9% of tests Untrained (‘usual) practitioners only 3 acceptable blows in 5.1% of tests 13.5% tests by trained group and 3.4% of untrained group achieved full acceptability and reproducibility. ___________________________________________________________________________ Patrick White,Wun Wong, Tracey Fleming and Barry Gray (2007) Primary care spirometry: test quality and the feasibility and usefulness of specialist reporting. British Journal of General Practice N=263 Specialists found: o 18% cases blow <6seconds o 8% cases failed to exhale quickly enough o 18% cases included a second breath/cough 29% disagreement in interpretation of diagnosis of obstructive disease (primary care clinicians didn’t interpret FEV1, FVC, FEV1/FVC appropriately) 8% cases primary care clinicians reported restrictive defects where the criteria were not met. 32% disagreement in severity of disease- Primary care clinicians did not adhere to national criteria for categorisation of obstruction. Over 15% of tests sent for reporting were incomplete 40% of completed tests were deemed unacceptable by specialists. There were also 49 tests without spirometry indices/flow loops/both; which when added to unacceptable tests provides a total of 52% tests deemed unacceptable. C.E. Bolton, A.A. Ionescu, P.H. Edwards, T.A. Faulkner, S.M. Edwards, D.J. Shale (2005) Attaining a correct diagnosis of COPD in general practice. Respiratory Medicine 99, 493–500 determined by questionnaire the availability, staff training, use and the interpretation results of spirometry in 72% of general practices in Wales Most practices had a spirometer (82.4%) and used it (85.6%) Confidence in use and interpretation of results varied widely: 58.1% were confident in use and 33.8% confident in interpretation Spirometry was performed more often if confident in use and interpretation (both Po0:001) and was related to greater training periods (Po0:001). Of the 125 patients previously diagnosed with COPD (without Spirometry), 61 had spirometric confirmation, while 25 had reversible obstruction (range 210–800 mls), 34 had normal and 5 had restrictive spirometry. Summary; only 49% of 125 patients were correctly diagnosed with COPD. 51% were incorrectly diagnosed Conclusion: Despite incentives to perform spirometry in general practice, lack of adequate training in use and interpretation suggests use is confounded and the diagnosis of COPD is likely to be made on imprecise clinical grounds.