Source: Peter J. Barnes, MD
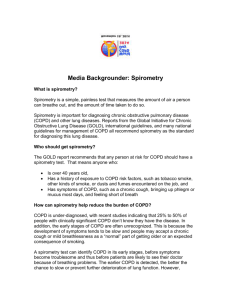
advertisement

COPD Consensus GOLD Global Initiative for chronic Obstructive Lung Disease Habib GHEDIRA, MD, Prof. Medical Faculty of Tunis Things we knew, things we did… Things we have learnt, things we should do Percent Change in Age-Adjusted Death Rates, U.S., 19651998 Proportion of 1965 Rate 3.0 3.0 2.5 2.5 Coronary Heart Disease Stroke Other CVD COPD All Other Causes –59% –64% –35% +163% –7% 2.0 2.0 1.5 1.5 1.0 1.0 0.5 0.5 0.0 0 1965 - 1998 1965 - 1998 1965 - 1998 1965 - 1998 1965 - 1998 Source: NHLBI/NIH/DHHS 2 Definition of COPD COPD is a preventable and treatable disease with some significant extrapulmonary effects that may contribute to the severity in individual patients. Its pulmonary component is characterized by airflow limitation that is not fully reversible. The airflow limitation is usually progressive and associated with an abnormal inflammatory response of the lung to noxious particles or gases. 3 Risk Factors for COPD Genes Exposure to particles Tobacco smoke Occupational dusts, organic and inorganic Indoor air pollution from heating and cooking with biomass in poorly ventilated dwellings Outdoor air pollution 4 Lung growth and development Oxidative stress Gender Age Respiratory infections Socioeconomic status Nutrition Comorbidities COPD : Pathology COPD ASTHMA Cigarette smoke Allergens Ep cells Mast cell CD4+ cell (Th2) Eosinophil Bronchoconstriction AHR Reversible 5 Alv macrophage Ep cells CD8+ cell (Tc1) Neutrophil Small airway narrowing Alveolar destruction Airflow Limitation Source: Peter J. Barnes, MD Irreversible Changes in Large Airways of COPD Patients Mucus hypersecretion Neutrophils in sputum Squamous metaplasia of epithelium No basement membrane thickening Goblet cell hyperplasia ↑ Macrophages ↑ CD8+ lymphocytes Mucus gland hyperplasia Little increase in airway smooth muscle Source: Peter J. Barnes, MD 6 Changes in Small Airways in COPD Patients Inflammatory exudate in lumen Disrupted alveolar attachments Thickened wall with inflammatory cells - macrophages, CD8+ cells, fibroblasts Peribronchial fibrosis Lymphoid follicle Source: Peter J. Barnes, MD 7 Changes in the Lung Parenchyma in COPD Patients Alveolar wall destruction Loss of elasticity Destruction of pulmonary capillary bed ↑ Inflammatory cells macrophages, CD8+ lymphocytes 8 Source: Peter J. Barnes, MD Diagnosis of COPD SYMPTOMS cough sputum shortness of breath EXPOSURE TO RISK FACTORS tobacco occupation indoor/outdoor pollution SPIROMETRY 9 Spirometry: Normal and Patients with COPD 10 Classification of COPD Severity by Spirometry 11 Stage I: Mild FEV1/FVC < 0.70 FEV1 > 80% predicted Stage II: Moderate FEV1/FVC < 0.70 50% < FEV1 < 80% predicted Stage III: Severe FEV1/FVC < 0.70 30% < FEV1 < 50% predicted Stage IV: Very Severe FEV1/FVC < 0.70 FEV1 < 30% predicted or FEV1 < 50% predicted plus chronic respiratory failure Therapy at Each Stage of COPD I: Mild II: Moderate III: Severe IV: Very Severe Add long term oxygen if chronic respiratory failure. Consider surgery Add inhaled glucocorticosteroids if repeated exacerbations Add regular treatment with one or more long-acting bronchodilators* (when needed); Add rehabilitation Active reduction of risk factor(s); influenza vaccination Add short-acting bronchodilator (when needed) * ß212 agonists, anticholinergics and methylxanthines Questions ? ~ Réponses ! Things we knew, things we did… Things we have learnt, things we should do