Pacemakers
advertisement

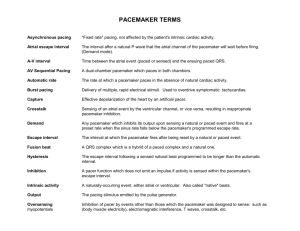
Pacemakers Saturday, March 14, 2009 OHOA JFICM and FANZCA Examinations Book – pages 176-178 Allen, M (2006) “Pacemakers and Implantable Cardioverter Defibrillators – Review Article” Anaesthesia 61, pages 883-890 - work by delivering a very short (<1ms), low voltage (<3V) electrical current via an insulated pacing lead to the heart muscle @ a preprogrammed rate. - also have the ability to detect the heart’s native electrical impulses and respond accordingly. - single or dual chamber device - radiofrequency reprogramming HISTORY - reason for pacemaker (bradyarrhythmias, severe heart failure – biventricular pacemaker, AV synchrony -> shown to reduce the risk of heart failure and AF) - how long patient has had it - whether functioning adequately - last interrogation (ideally within last 3 months) - battery life - base line rate - review device ‘passport’ Pacemaker Code = 5 letters - first 3 = anti-bradycardia functions (always stated) - last 2 = related to additional functions 1. Paced chamber (0 = none, V = ventricle, A = atrium, D = dual (A+V)) 2. Sensing chamber (0, V, A, D (A+V)) 3. Response to sensing (0 = none, T = triggered, I = inhibited, D = dual (T+I)) 4. Rate modulation or Programmability (0 = none, P = single programmable, M = multiprogrammable, R = rate modulation in response to minute ventilation or movement) 5. Anti-tachycardia functions (0 = none, P = pacing, S = shock, D = dual (P+S) or Multi-site pacing Acronym = PS RRA COMMON MODES VVI - ventricular pacing and sensing if no electrical impulse sensed then pacemaker will pace @ a pre-programmed rate if electrical impulse sensed then pacing inhibited asynchronous pacing VVIR - same as above but there is a rate-adaptive mechanism installed to match physiological needs of patient Jeremy Fernando (2011) DDD - both atrium and ventricle both sensed and paced - if both SA and AV node functioning then pacemaker will just sense - if either atrium or ventricle not conveyed -> pacemaker will take over DDDR - same as above except has a rate-adaptive mechanism VOO - mode that pacemaker should be set to for surgery (asynchronous pacing) ventricle paced at a pre-programmed rate sensing not interfered with by diathermy and other forms of electromagnetic interference monitor for R on T with diathermy -> - recent visit to cardiology clinic should confirm; adequate battery life and normal function of pacemaker system - pacemakers work but inducing a current between anode and cathode above the threshold of the myocardial cell -> depolarization - symptoms – chest pain, palpitations, black outs, collapses, orthopnoea, PND, SOBE, ankle swelling - exercise capacity - co-morbidities: IHD, HT, CVA, COPD, hyperlipidaemia, cardiomyopathy, valve dysfunction, HOCM, congenital QT syndromes - medications: relevant anti-arrhythmics and treatments for above conditions - recent cardioversions EXAMINATION - thorough CVS examination - pacemaker site – integrity, signs of infection, relation to operative site and diathermy. - signs of heart failure – tachycardia, hyper/hypotension, atrial fibrillation, JVP, HS and murmurs, RVH and apex displacement, crackles or pleural effusions in chest, enlarged liver, pitting oedema. INVESTIGATIONS - U+E – electrolytes balanced including Mg2+ (abnormalities can result in loss of capture) - relevant drug levels – digoxin - 12 Lead ECG – underlying rhythm and rate, pacing spikes, electrical activity followed by pacing spike, AV synchronicity - ECHO – LV function and valve function, signs of PHT - CXR: cardiac failure, position of pacemaker, leads position - Angiogram – coronary artery integrity - Recent interrogation - EPS studies Jeremy Fernando (2011) MANAGEMENT Pre-procedure - surgery – approach, duration, position of patient required (supine or beach chair), location of diathermy pad and type of diathermy - whether a device is to be altered prior to surgery is dependent on 4 things: 1. 2. 3. 4. anticipated amount of EMI type of device (pacemaker, ICD or CRT) pacemaker dependency rate adaptive features - if surgery is not around the pacemaker and use if diathermy minimal -> don’t have to alter - if rate modulated pacemaker -> deactivate prior to theatre Intraoperative - standard monitoring - turn paced mode on the ECG ELECTROMAGNETIC INTERFERENCE (EMI) Causes - diathermy (monopolar & bipolar) mobile phones (don’t place over pacemaker) MRI shivering faciculations alterations in heart size positive pressure ventilation peripheral nerve stimulators TENS machine defibrillation Possible Results - inappropriate triggering or inhibition of output asynchronous pacing reprogramming damage to device circuitry pacing wires may acts as aerials and cause heating of endocardium Prevention - use bipolar diathermy - if conventional diathermy required position plate so that most of current passes away from the pacemaker, use short, sharp bursts and watch SpO2 or art line. - ensure all devices are not in the same vector as the pacemaker current (between pacemaker and heart) Jeremy Fernando (2011) - if reason for pacemaker severe heart failure where loss of AV synchrony may precipitate haemodynamic compromise -> have a telemetric programmer and cardiac technician close @ hand - keep lithotripter atleast 6 inches away from pacemaker (should be timed with ECG and rate modulation deactivated) - if have to defibrillate keep pads as far from pace maker as possible - avoid sux c/o faciculations (if used in a patient with a sensing mode activated -> use defaciculating dose of NDNMBD) - avoid using defibrillation if at all possible (high level of EMI) -> if required use AP pad configuration and keep pad’s 10cm away from pacemaker. Magnets and Pacemakers - no longer recommended to place magnet over pacemakers -> only applicable to older nonreprogrammable pacemakers. - placement of a magnet would default mode to an asynchronous mode or a fixed rate - all modern pacemakers are reprogrammable. Management of Pacemaker Malfunction - have cardio-technician in OT praecordial thumps (percussive pacing) isoprenaline adrenaline transthoracic external pacing (capture around 80mA) trans-venous pacing trans-oesophageal pacing Post-procedure Management - cardiac technician should interrogate pacemaker and reprogram rate modulation or other specific modes PROBLEMS - pacemaker syndrome: single chamber pacing -> retrograde conduction from ventricular systole -> flows to atria and produces decreased Q, SOB, palpitations, syncope - pacemaker tachycardia: dual chamber pacing -> short circuit between the two electrodes. Jeremy Fernando (2011)