Jana's Enteral
advertisement

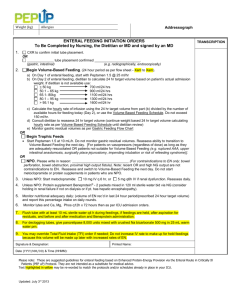
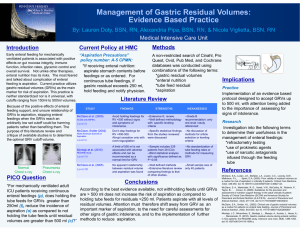
Enteral Nutrition What is enteral nutrion o Any form of administration that involves any part of the GI tract o Nutrients given in the GI tract o Preserves GI integrity Enteral routes o Orally o Rectally o Gastric – duodenal – jejunum TPN (aka HAL) – total parental nutrition o Has to be in a central line o Nonfunctional GI Tract o Extended Bowel Rest o Severe diarrhea o Pancreatitis o Inflammatory bowel disease Chromes, diverticulitis o Preoperative TPN o GI tract nonusable for greater than 4-5 days o Severe malnutrition – not under pre-op TPN Conditions requiring enteral feeding • Gastrointestinal problems – short bowel syndrome, fisula formation, infalmmatory bowel disease (chron’s disease, diverticulitis) • Cancer therapy – radiation and chemo (require enteral feeding cause cant keep food down) • Convalescent care – period needed for returning to health after illness • Hypermetabolic conditions – burns, trauma, AIDS, alcoholism, anorexia nervosa • Debilitation – in a state of not being able to do anything – coma, paralysis, stroke, respiratory distress, head injury • Surgical interventions – surgery – facial surgery, broken jaw Enteral Tubes • Deliver fluid to stomach – Salem sump – type of NG tube – Gastrostomy (G-tube) – directly into the stomach, surgically placed, cut into the stomach (from the outside in) and place the tube, long term • Deliver fluid to intestine (duodenum or jejunum) – Dobbhoff – nasoenteric tube into the duodenum – through the nose into the duodenum – J-tube and dobbhoff safer cause there is no chance for aspiration** Care of the gastrostomy tube site • • • PEG tubes – remove dressing 24 hrs after insertion unless otherwise ordered, by endoscopic, does not go under anesthesia, put through the mouth Other type of gastrostomy tubes – by surgery, sterile dressing change for 14 days, cover with sterile gauze x14 days or if draining it could be longer, ½ normal saline, ½ hydrogen peroxide, dry then dressing Findings to report to physician – redness, swelling, color and amount of drainage Types of enteral feedings • Intermittent – Usually gastric administration – Large amounts of solution 4-8 times/day – Typically administered over 30 minutes – Can be by pump or gravity • Bolus – Continuous feedings at faster rate over shorter time – By syringe or gravity – Example: ensure • Continuous – Usually intestinal administration – Continuous rate via pump • Cyclic – Over longer period of time – Usually on pump – Typically over several hours – Example: feeding infused over night- so pt has one going on during the day – remember: sit them up at the start Management of enteral tubes • Patient position – HOB up at least 30 degrees (#1) • Check for gastric residual – (#3) every 4 hours, withdraw all of it and return up to 150 mL in the stomach (return gastric enzymes and so there is not an electrolyte imbalance) – Rule: hold meds if more than 100 mL is withdrawn in the stomach or more than 2x the rate of the feeding – hold for 2 hrs and then recheck, if less than 100 mL give med and resume feeding, if still 100 or more mL then hold meds and food still and call the dr. • Verify placement – if its not continuous – on everything else (#2) – aspirate to visual contents and ascultate ove LUQ 10-20 mL of air (do not verify if continuous, jejunum, duodenum) • Maintaining tube patency – check for gastric residula every 4 hours – flush tube with 20-50 mL with warm tap water • If clogs then use “clog zapper” (carbonated liquid and wire) – 7-up • Maintaining equipment – have reserve battery just in case Enteral solutions • Choice depends on – Size & location of tube – small tubes need thinner solution/ formula – Caloric needs of patient – dietician and dr. collaborate to make sure the pts needs are met – (post-op – a pt needs 1500 calories per day) – Type of nutritional supplement – whatever the pt needs, extra fat, extra protein, extra carbs – Method of delivery – on and off (bolus, intermittent, cyclic) or continuous – Patient convenience – minimal prep in home care, most enteral feedings do not have to stay in the refrigerator – they can sit out at room temp Nutritional products • Commercial formulas (good for 24 hrs) – Fixed – components are predetermined and mixed – Modular – specific components can be mixed to pt specific needs – Disease specific – specific to the disease • Supplements – ensure, boost • Blenderized – normal foods that are liquefied Complications of enteral therapy • Gastrointestinal – – diarrhea (most common – caused by hyperosmolar formulas – can also be caused by cold formulas, different meds, a change in the feeding rate) – gas or cramps – caused by air in the tube – dumping syndrome- goes right through you – too rapid, cold formulas, too much fluid when flushing the tube – constipation – can be caused by lack of fiber, high milk content, inadequate fluid intake • Mechanical – tube obstruction – inadequate flushing or rate of formula or residue from med administration, unsecured tube will lead to improper placement – tube migration – can cause aspiration pneumonia (symptoms: coughing, vomiting) • Metabolic – hyperglycemia – if you get glucose intolerance from feeding formula and cause this, abnormal electrolytes, hydration problems – dehydration or fluid overload Minimizing complications • GI – Room temp formulas – if too hot or cold can stimulates peristalsis causing diarrhea or dumping syndrome – Monitor gastric residual (every 4 hrs) – Appropriate fiber & water content – constipation prevented by having adequate fiber and water • Mechanical – Check tube placement – to prevent aspiration • – HOB elevated 30 degrees – unless contraindicated – Appropriate medication formulation – get the liquid meds when possible and dilute them, if thick crush meds and mix with warm water Metabolic – Check blood glucose levels – check blood levels to determine hyperglycemia – I&O - could be experiencing dehydration (tenting, sticky mouth, tired) or fluid overload – Report and regulate feeding rates/formulation – work with dietician and dr to determine feeding rates and needs