Enteral Nutrition for Adult Patients
advertisement

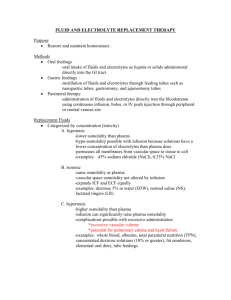
Enteral Nutrition for Adults: Administration Issues including material from Dietitians in Nutrition Support A DIETETIC PRACTICE GROUP OF AMERICAN DIETETIC ASSOCIATION “Your link to nutrition and health.” Contraindications for EN Severe acute pancreatitis High output proximal fistula Inability to gain access Intractable vomiting or diarrhea Aggressive therapy not warranted Expected need less than 5-7 days if malnourished or 7-9 days if normally nourished ASPEN. The science and practice of nutrition support. A case-based core curriculum. 2001; 143 Contraindications for EN Inadequate resuscitation or hypotension; hemodynamic instability Ileus Intestinal obstruction Severe G.I. Bleed Indicators of Adequate Fluid Resuscitation in Critically Ill Pts Urine output should be >30 ml/hour Heart rate <120 beats/minute; preferably <100 beats/minute Systolic BP should be ~100 Ask staff/medical team If patient is receiving fluid boluses in addition to continuous IVF, likely they are not adequately resuscitated Nasogastric Tubes Nasogastric Tubes Definition A tube inserted through the nasal passage into the stomach Indications: Short term feedings required Intact gag reflex Gastric function not compromised Low risk for aspiration French Units—Tube Size Diameter of feeding tube is measured in French units 1F = 33 mm diameter Feeding tube sizes differ for formula types and administration techniques Generally smaller tubes are more comfortable and better suited to NG or NJ feedings May be more likely to clog with viscous formula or formula mixtures Nasogastric Tubes Advantages: Ease of tube placement Surgery not required Easy to check gastric residuals Accommodates various administration techniques Nasogastric Tubes Disadvantages: Increases risk of aspiration (maybe) Not suitable for patients with compromised gastric function May promote nasal necrosis and esophagitis Impacts patient quality of life Nasoduodenal/Jejunal Definition A tube inserted through the nasal passage through the stomach into the duodenum or jejunum Indications: High risk of aspiration Gastric function compromised Nasoduodenal/Jejunal Advantages: Allows for initiation of early enteral feeding May decrease risk of aspiration Surgery not required EAL EN Tube Placement Guidelines Critical Care Enteral Nutrition (EN) administered into the stomach is acceptable for most critically ill patients. If your institution's policy is to measure GRV, then consider small bowel tube feeding placement in patients who have more than 250ml GRV or formula reflux in two consecutive measures. Small bowel tube placement is associated with reduced GRV. ADA EAL Critical Care Guidelines accessed 8-07 EAL EN Guidelines (Critical Care) Adequately-powered studies have not been conducted to evaluate the impact of GRV on aspiration pneumonia. There may be specific disease states or conditions that may warrant small bowel tube placement (e.g., fistulas, pancreatitis, gastroporesis), however they were not evaluated at this phase of the analysis. Fair; conditional ADA EAL Guidelines Critical Care accessed 8-07 Nasoduodenal/Jejunal Disadvantages: Transpyloric tube placement may be difficult Limited to continuous infusion May promote nasal necrosis and esophagitis Impacts patient quality of life Orogastric Tube is placed through mouth and into stomach Often used in premature and small infants as they are nasal breathers Not tolerated by alert patients; tubes may be damaged by teeth GastrostomyJejunosotomy Enterostomy Placement Gastrostomy Jejunostomy Gastrostomy Definition A feeding tube that passes into the stomach through the abdominal wall. May be placed surgically or endoscopically Indications: Long-term support planned Gastric function not compromised Intact gag reflex present Gastrostomy Disadvantages: May require surgery Stoma care required Potential problems for leakage or tube dislodgment Gastrostomy Jejunostomy Definition A feeding tube that passes into the jejunum through the abdominal wall. May be placed endoscopically or surgically Indications: Long-term feeding option for patients at high risk for aspiration or with compromised gastric function Jejunostomy Advantages: Post-op feedings may be initiated immediately Decreased risk of aspiration Suitable option for patients with compromised gastric function Stable patients can tolerate intermittent feedings Jejunostomy Disadvantages: Requires stoma care Potential problems related to leakage or tube dislodgement/clogging may arise May restrict ambulation Bolus feedings inappropriate (stable patients may tolerate intermittent feedings) Determining Method of Administration Feeding site Clinical status of patient Type of formula used Availability of pump Mobility of patient Initiation of Enteral Feedings Dilution of enteral formulas not generally recommended Initiate at full strength at slow rate and steadily advance Allows achievement of goal rates more quickly; less manipulation of formula Administration Bolus Intermittent Continuous Cyclic Bolus Feedings Definition Infusion of up to 500 ml of enteral formula into the stomach over 5 to 20 minutes, usually by gravity or with a large-bore syringe Indications: Recommended for gastric feedings Requires intact gag reflex Normal gastric function Bolus Feedings Advantages: More physiologic Enteral pump not required Inexpensive and easy administration Limits feeding time so patient is free to ambulate, participate in rehabilitation, or live a more normal life in the home Makes it more likely patient will receive full amount of formula Bolus Feeding Bolus Feeding Disadvantages: Increases risk for aspiration Hypertonic, high fat, or high fiber formulas may delay gastric emptying or result in osmotic diarrhea Initiation of Bolus Feedings Adults: Initiate with full strength formula 3- 8 times per day with increases of 60-120 ml q 8-12 hours as tolerated up to goal volume; does not require dilution unless necessary to meet fluid requirements Children: Initiate with 25% of goal volume divided into the desired number of daily feedings; increase by 25% each day divided among all feedings until goal volume is reached ASPEN Nutrition Support Practice Manual, 2005, 2nd ed, p. 78 Continuous Feedings Indications: Initiation of feedings in acutely ill patients Promote tolerance Compromised gastric function Feeding into small bowel Intolerance to other feeding techniques Continuous Feedings Definition Enteral formula administration into the gastrointestinal tract via pump or gravity, usually over 8 to 24 hours per day Advantages: May improve tolerance May reduce risk of aspiration Increased time for nutrient absorption Continuous Feedings Disadvantages: May reduce 24-hour infusion May restrict ambulation More expensive for home support Pumps are more accurate; useful for small-bore tubes and viscous feedings, but many payers have strict criteria for approval of pumps for home or LTC use Initiation of Continuous Feedings Adults: Initiate at full strength at 10-40 ml/hour and advance to goal rate in increments of 10 to 20 mL/hour q 8-12 hours as tolerated Can be used with isotonic or hyperosmolar formulas Children: Isotonic formula full strength at 12 mL/kg/hour and advanced by .5-1 mL/kg/hour q 6-24 hours until goal rate is achieved ASPEN Nutrition Support Practice Manual, 2005, 2nd ed, p. 78 Intermittent Feedings Definition Enteral formula administered at specified times throughout the day; generally in smaller volume and at slower rate than a bolus feeding but in larger volume and faster rate than continuous drip feeding Typically 200-300 ml is given over 30-60 minutes q 4-6 hours Precede and follow with 30-ml flush of tap water Indications: Intolerance to bolus administration Initiation of support without pump Preparation of patient for rehab services or discharge to home or LTC facility The A.S.P.E.N. Nutrition Support Practice Manual, 2nd Edition, 2005 Intermittent Feedings Advantages: May enhance quality of life – Allows greater mobility between feedings – More physiologic – May be better tolerated than bolus Intermittent Feedings Disadvantages: Increased risk for aspiration Gastric distention Delayed gastric emptying Cyclic Feedings Definition Administration of enteral formula via continuous drip over a defined period of 8 to 12 hours, usually nocturnally Indications: Ensure optimal nutrient intake when: – Transitioning from enteral support to oral nutrition (enhance appetite during the day) – Supplement inadequate oral intake – Free patient from enteral feedings during the day Cyclic Feedings Advantages: Achieve nutrient goals with supplementation Facilitates transition of support to oral diet Allows daytime ambulation Encourages patient to eat normal meals and snacks Cyclic Feedings Disadvantages: May require high infusion rates—may promote intolerance Enteral Feeding Tubes Types: pediatric vs adult; gastric vs small bowel Sizes: smaller sizes (5-8 Fr) for commercial products delivered via pump; larger sizes for viscous, blenderized, fiber-containing formulas, gravity and bolus feedings Weighted vs. unweighted: it was once thought that weighted tubes facilitated transpyloric passage; now dictated by personal preference Stylet vs. no stylet: stylet facilitates tube placement beyond the pylorus for small, flexible tubes Composition: silicone and polyurethane most comfortable Factors Affecting Tube Selection Will the patient be fed into the stomach or small bowel? How long will the patient need tube feedings? Is the patient expected to resume adequate oral feedings? Who can insert feeding tubes at my institution? Enteral Feeding Containers May be rigid or flexible Sterile or non-sterile Unbreakable, leakproof, and disposable Considerations in Choosing Enteral Feeding Containers Easy to fill, close and hang Easy to read calibrations and directions Appropriate size Adaptable tubing port Compatible with pump Requires minimal storage space Adapted from ASPEN. The science and practice of nutrition support. A casebased core curriculum. 2001; 179 Closed Systems Enteral Feeding Pumps Factors in Pump Selection Simple to use Dose function (intuitive) Alarm system Lightweight Long battery life Portable Volume infused indicator Flow rate accurate to within 10% Approved for age range in which it will be used Permanently attached cord Enteral Feeding Complications Mechanical Gastrointestinal Metabolic Infectious Mechanical Feeding tube obstruction Feeding tube dislodged Nasal irritation Skin irritation/excoriation at ostomy site Causes of Feeding Tube Obstruction Concentrated, viscous, and fiber-containing feeding products Tube feeding contamination Checking of gastric residuals Small diameter tubes Powdered or crushed medication flushed through tubes Acidic or alkaline medications passed through tubes Tubes not routinely flushed after feedings are stopped Prevention of Feeding Tube Obstruction Flush the feeding tube, especially before and after medication administration and bolus/intermittent feedings Use liquid formulations of medicines where possible (but be careful of osmolarity) Do not mix medications with enteral feedings unless shown to be compatible Avoid crushing sustained-release or entericcoated tablets Treatment of Feeding Tube Obstruction Declog with irrigants (warm water) or sodium bicarbonate/pancrealipase mixture or by mechanical means Cola beverages, cranberry juice, and tea not recommended The A.S.P.E.N. Nutrition Support Practice Manual, 2nd Edition, 2005 Aspiration Reported incidence of aspiration in tubefed patients varies from .8% to 95%. Clinically significant aspiration 5% gastric-fed pts Many aspiration events are “silent” and often involve oropharyngeal secretions Symptoms include dyspnea, tachycardia, wheezing, rales, anxiety, agitation, cyanosis May lead to aspiration pneumonia Aspiration Focus has been on detection of aspiration through use of coloring agents in enteral feedings or glucose testing of respiratory secretions These methods have low sensitivity and questionable specificity; they do not prevent aspiration but at best detect it after it has occurred Blue food coloring used for this purpose has been associated with morbidity/mortality in septic patients Aspiration Prevention Keep head of bed elevated 30-45 degrees during and 30-40 minutes after feedings Feed post-pylorically (research mixed on this) Small, frequent feedings or continuous drip Use of promotility agents Monitoring of gastric residuals may be helpful in identifying delayed gastric emptying and increased risk of aspiration The A.S.P.E.N. Nutrition Support Practice Manual, 2nd Edition, 2005 Gastrointestinal Complications Diarrhea Constipation Gastric distention/bloating Gastric residuals/delayed gastric emptying Nausea/vomiting Diarrhea Definition: >500 ml every 8 hours or more than 3 stools a day for at least two consecutive days. Relates more to stool consistency than frequency Diarrhea was a common consequence of enteral feedings when hyperosmolar feedings were routinely delivered via syringe Occurs in 2 to 63% of enterally-fed pts depending on how defined Causes/Treatments of Diarrhea Intestinal atrophy due to malnutrition – EN is the best stimulant for recovery. Increase rate slowly as tolerated – Albumin infusion is unlikely to be helpful; diarrhea is not caused by low albumin; it is a marker of malnutrition Bolus feeding in the small intestine: results in dumping syndrome. – Use an infusion pump to regulate flow The A.S.P.E.N. Nutrition Support Practice Manual, 2nd Edition, 2005 Causes/Treatments of Diarrhea Bacterial overgrowth of intestinal tract or contamination of the enteral feeding – Avoid prolonged use of broad-spectrum antibiotics – Use clean technique and closed system in handling enteral feedings – Limit hang time of open system formulas to 8 hours (4 hours for mixtures) – Change bag and tubing per protocol – Test for C difficile and other pathogens before using anti-motility agents Causes/Treatments of Diarrhea Steatorrhea: characterized by frothy, odiferous stools that float on water; caused by fat intolerance – Use lowfat enteral formula or one with higher percentage of MCT; pancreatic enzymes may help in pancreatic insufficiency Causes/Treatments of Diarrhea Lactose intolerance – Most enteral products are lactose free but this may occur with initiation of full liquid diet. Eliminate milk and dairy products Drug-induced diarrhea – Meds may cause up to 61% of diarrhea in tubefed pts due to hypertonicity or direct laxative action (magnesium, sorbitol, potassium). Diarrhea most common with antibiotics. Discuss with MD/pharmacist The A.S.P.E.N. Nutrition Support Practice Manual, 2nd Edition, 2005 Causes/Treatments of Diarrhea Infusion of hypertonic feeding solutions; rare unless delivered at very high rate or bolused into small bowel – Try a different product rather than diluting the original feeding GI disease: such as IBS, short gut, celiac disease, AIDS – May require PN or specially formulated EN Treatment of Diarrhea in General Add soluble fiber (such as banana flakes or Benefiber) or insoluble fiber such as psillium Consider an enteral formula with added fiber Use an antidiarrheal agent (loperamide, diphenoxylate, paregoric, octreotide) Change the formula Nausea/Vomiting 20% of patients on EN report nausea/vomiting Often related to delayed gastric emptying caused by hypotension, sepsis, stress, anesthesia, medications (analgesics and anticholinergics), surgery Nausea/Vomiting Treatment Consider reducing/discontinuing narcotic medications Switch to a lowfat formula Administer feeding solution at room temperature Reduce rate of infusion by 20-25 ml/hr Administer prokinetic agent (metoclopramide, erythromycin, domperidone, bethanechol) Check gastric residuals Consider antiemetics Metabolic Fluid and Electrolyte abnormalities Glucose intolerance Ca++, Mg++, PO4 abnormalities Other Fluid and Electrolyte Disturbances May result from long term nutrition deficits, acute stress, medications, medical conditions, improper nutrient prescription Electrolytes lost via stool, urine, ostomy or fistula drainage Dehydration most common complication (tube feeding syndrome) especially with high protein feeding and insufficient fluid Hyperglycemia Often reflects acute stress, infection, medications (especially steroids) or latent diabetes Macronutrient distribution: is generally not the primary issue; most enteral feeding formulas fall within established guidelines; could try formula lower in carbohydrate Insulin management Refeeding Syndrome At risk: when refeeding those with marginal body nutrient stores, stressed, depleted patients, those who have been unfed for 710 days, persons with anorexia nervosa, chronic alcoholism, weight loss Symptoms: Hypokalemia, hypophosphatemia and hypomagnesemia; cardiac arrhythmias, heart failure; acute respiratory failure Refeeding Syndrome Correct electrolyte abnormalities (via oral, enteral, parenteral route) before initiating nutrition support Administer volume and energy slowly Monitor pulse rate, intake and output, and electrolyte levels Provide appropriate vitamin supplementation Avoid overfeeding Infectious Complications Formula contamination Unsanitary equipment Failure to follow appropriate protocols re handling of enteral feedings/changing of bags and tubing Monitoring of Patients on EN Electrolytes BUN/Cr Albumin/prealbumin Ca++, PO4, Mg++ Weight Input/output Vital signs Stool frequency/consistency Abdominal examination Evaluating Adequacy of Support I’s and O’s (what % of prescribed feeding did patient receive?) Indirect calorimetry Nitrogen balance Weight Visceral proteins Other Home Support Discharge planning – May work with DME company to identify whether patient is a candidate for home EN, assure availability of product; complete CMN form in conjunction with physician Patient education – Patients going home on enteral feedings will need education on food safety, feeding administration, and self-monitoring Reimbursement Enteral Support Summary Preferred method of nutrition support Technology exists to facilitate implementation Can be successfully employed with careful patient and formula selection